Evidence-Based Supplements and Complementary Therapies

Panic disorder affects millions worldwide, characterized by sudden, intense episodes of fear accompanied by overwhelming physical symptoms such as racing heart, chest pain, shortness of breath, dizziness, and a sense of impending doom. These panic attacks can be so distressing that individuals often develop anticipatory anxiety—fear about when the next attack might occur—leading to avoidance behaviors that can significantly restrict daily activities and quality of life.
While conventional treatments, including cognitive-behavioral therapy and medication, remain the foundation of panic disorder treatment, many individuals seek complementary approaches, either as alternatives or adjuncts to standard care. This growing interest has spurred research into the potential benefits of various nutritional supplements, herbal remedies, and mind-body practices for panic symptoms.
This article examines the evidence behind natural approaches to panic disorder, exploring which supplements and complementary therapies show promise, their mechanisms of action, safety considerations, and how they might be integrated with conventional treatments for optimal outcomes.
Understanding Panic Disorder: Beyond the Attack
Panic disorder is more than just experiencing occasional anxiety. The condition involves recurrent, unexpected panic attacks along with persistent concern about having additional attacks or significant behavioral changes related to the attacks. These episodes typically peak within minutes and include intense physiological and psychological symptoms that can mimic serious medical conditions like heart attacks.
The neurobiological underpinnings of panic disorder involve dysregulation in several brain regions, particularly the amygdala (fear center) and related limbic structures. Neurotransmitter systems, including GABA (gamma-aminobutyric acid), serotonin, and norepinephrine, play crucial roles in modulating fear responses and anxiety states. Dysfunction in these systems contributes to the characteristic symptoms of panic disorder.
Environmental factors often interact with genetic vulnerabilities, with stress, trauma, and certain health conditions potentially triggering or exacerbating panic symptoms. Understanding these mechanisms provides a foundation for exploring how various natural approaches might address the underlying factors contributing to panic attacks.
Nutritional Supplements with Evidence for Panic Disorder
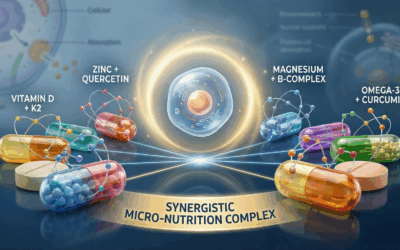
Omega-3 Fatty Acids
Omega-3 fatty acids, particularly EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid) found in fatty fish, have received significant attention for their potential mental health benefits. These essential fatty acids serve as critical components of neural cell membranes and influence neurotransmitter function, inflammation processes, and neuroplasticity.
A 2018 systematic review and meta-analysis published in JAMA Network Open examined 19 clinical trials and concluded that omega-3 supplementation showed promise for reducing anxiety symptoms, including those associated with panic disorder. The researchers found that higher doses of omega-3s (above 2000mg daily) demonstrated greater effectiveness compared to lower doses.
The anti-inflammatory properties of omega-3s may be particularly relevant, as increasing evidence points to connections between inflammation and anxiety disorders. Additionally, these fatty acids appear to modulate serotonin and dopamine transmission, potentially enhancing the benefits of conventional treatments that target these neurotransmitter systems.
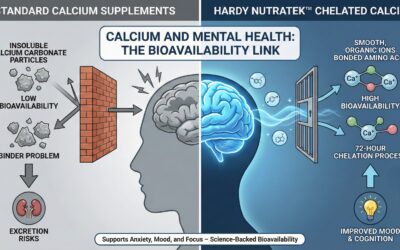
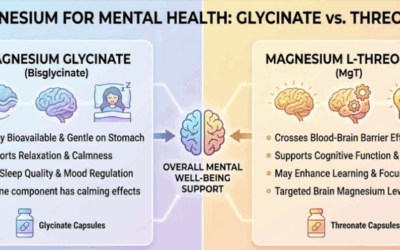
Magnesium
Magnesium plays essential roles in over 300 enzymatic reactions in the body and has particular relevance to nervous system function. This mineral helps regulate neurotransmitters, modulates stress responses, and supports healthy muscle function—all factors that can influence panic symptoms.
Research investigating magnesium for anxiety disorders has yielded promising results. A systematic review published in the journal Nutrients found that magnesium supplementation appeared effective for mild anxiety and anxiety-related disorders, particularly when combined with other nutrients. Magnesium’s mechanisms for addressing anxiety symptoms likely involve multiple pathways, including:
- Modulation of the hypothalamic-pituitary-adrenal (HPA) axis, which regulates stress responses
- Regulation of NMDA receptors, which influence excitatory neurotransmission
- Support for GABA function, which provides inhibitory (calming) signals in the brain
- Reduction of inflammatory processes that may contribute to anxiety states
Given magnesium’s excellent safety profile and the prevalence of insufficient intake in modern diets, supplementation represents a reasonable approach for individuals with panic symptoms, particularly those with suboptimal dietary magnesium consumption.
B Vitamins
B vitamins serve as essential cofactors in numerous enzymatic reactions in the brain, particularly those involved in neurotransmitter synthesis and energy production. Deficiencies in various B vitamins have been linked to increased anxiety, depression, and impaired stress resilience.
Vitamin B6 (pyridoxine) is particularly relevant for panic symptoms, as it functions as a cofactor in the production of GABA, the primary inhibitory neurotransmitter in the brain. Adequate GABA activity helps prevent the excessive neuronal excitation associated with anxiety and panic states.
Vitamin B12 (cobalamin) and folate (B9) support methylation processes necessary for monoamine neurotransmitter production, including serotonin, which plays crucial roles in mood regulation and anxiety modulation. A study in the Journal of Affective Disorders found that supplementation with B vitamins, particularly folate, improved outcomes for individuals with depression and anxiety symptoms who were receiving antidepressant treatment.
While research specifically focused on B vitamins for panic disorder remains limited, their fundamental roles in neurological function and mood regulation suggest potential benefits, particularly for individuals with suboptimal vitamin status.
Inositol
Inositol, sometimes considered part of the B-vitamin complex, has demonstrated efficacy for panic disorder in several controlled trials. This naturally occurring isomer of glucose serves as a precursor for phosphatidylinositol, a key component of cell membranes and second messenger systems involved in neurotransmitter signaling.
A double-blind, placebo-controlled crossover study published in the Journal of Clinical Psychopharmacology found that high-dose inositol (12g daily) significantly reduced the frequency and severity of panic attacks compared to placebo. Additional research in the American Journal of Psychiatry demonstrated that inositol produced effects comparable to fluvoxamine (a selective serotonin reuptake inhibitor) in treating panic disorder, but with fewer side effects.
Inositol’s mechanisms appear to involve modulation of serotonin receptors, potentially enhancing serotonergic transmission in a manner similar to but distinct from SSRIs. This unique mechanism may explain why some individuals who don’t respond adequately to conventional medications might benefit from inositol supplementation.
Herbal Remedies with Evidence for Panic Symptoms
Kava (Piper methysticum)
Kava has a long history of traditional use in Pacific Island cultures for its calming and anxiolytic effects. The active compounds, kavalactones, appear to work through multiple mechanisms, including modulation of GABA receptors, effects on voltage-gated ion channels, and mild inhibition of norepinephrine reuptake.
A rigorous randomized, double-blind, placebo-controlled study published in Psychopharmacology found that kava extract (containing 70% kavalactones) significantly reduced anxiety in patients with generalized anxiety disorder. While specific studies focused exclusively on panic disorder are limited, the anxiolytic effects demonstrated in clinical research suggest potential benefits for panic symptoms.
However, safety concerns have emerged regarding kava’s potential for hepatotoxicity, leading to restrictions in some countries. Current evidence suggests that hepatotoxic reactions are rare and may be associated with poor-quality products, alcohol use, or genetic factors. When considering kava, it’s essential to use standardized extracts from reputable sources and to consult with healthcare providers, particularly for individuals with liver conditions or those taking medications metabolized by the liver.
Passionflower (Passiflora incarnata)
Passionflower has demonstrated anxiolytic effects comparable to benzodiazepines in some studies, but with fewer side effects and lower addiction potential. The herb contains flavonoids and alkaloids that appear to modulate GABA receptors, promoting inhibitory neurotransmission that helps calm excessive neural activity.
A randomized controlled trial published in the Journal of Clinical Pharmacy and Therapeutics compared passionflower extract to oxazepam (a benzodiazepine) for generalized anxiety disorder. While both treatments showed similar efficacy, passionflower produced fewer side effects and less impairment of job performance.
For individuals with panic disorder, particularly those with accompanying generalized anxiety, passionflower may offer a gentler alternative to pharmaceutical anxiolytics. Its favorable safety profile makes it suitable for consideration as part of a comprehensive approach to managing panic symptoms.
Lemon Balm (Melissa officinalis)
Lemon balm contains bioactive compounds that appear to inhibit GABA transaminase, the enzyme responsible for breaking down GABA, potentially increasing GABAergic activity in the brain. Additional mechanisms include modulation of muscarinic and nicotinic acetylcholine receptors, which influence cognitive function and anxiety states.
Research published in Phytomedicine demonstrated that a standardized lemon balm extract reduced laboratory-induced stress and improved self-rated calmness in healthy volunteers. While specific studies in panic disorder populations are lacking, the documented anxiolytic effects suggest potential benefits for individuals experiencing panic symptoms.
Lemon balm’s excellent safety profile and mild sedative properties make it particularly suitable for individuals with concurrent sleep disturbances, which frequently accompany panic disorder. When used as a tea or standardized extract, it represents one of the gentler herbal approaches for anxiety symptoms.
Ashwagandha (Withania somnifera)
This adaptogenic herb from Ayurvedic medicine has gained attention for its potential to modulate stress responses and reduce anxiety symptoms. Ashwagandha contains withanolides and other bioactive compounds that appear to attenuate cortisol levels and normalize hypothalamic-pituitary-adrenal (HPA) axis function, potentially reducing the physiological stress response that can trigger panic attacks.
A double-blind, randomized controlled trial published in the Journal of Clinical Psychopharmacology found that ashwagandha root extract significantly reduced anxiety scores compared to placebo in adults with anxiety disorder. Participants receiving ashwagandha also showed reduced serum cortisol levels, suggesting modulation of physiological stress responses.
For individuals with panic disorder, particularly those with elevated baseline anxiety and stress sensitivity, ashwagandha may offer benefits by enhancing stress resilience and attenuating the body’s physiological response to stressors that might otherwise trigger panic attacks.
Mind-Body Approaches for Panic
Mindfulness Meditation
Mindfulness practices involve cultivating non-judgmental awareness of present-moment experiences, including physical sensations, thoughts, and emotions. This approach can be particularly valuable for panic disorder, as it helps individuals develop a different relationship with the physical sensations and catastrophic thoughts that characterize panic attacks.
A meta-analysis published in the Journal of Anxiety Disorders examined mindfulness-based interventions for anxiety disorders and found moderate effects for reducing anxiety symptoms. Specific research on panic disorder has demonstrated that mindfulness-based cognitive therapy (MBCT) significantly reduced panic symptoms and improved quality of life in affected individuals.
The mechanisms through which mindfulness practices benefit panic disorder likely include:
- Interoceptive exposure: Mindfully observing bodily sensations without attempting to control or avoid them serves as a form of exposure therapy for panic-related sensations
- Decentering: Learning to view thoughts (including catastrophic misinterpretations) as mental events rather than facts or threats
- Autonomic regulation: Regular practice appears to enhance parasympathetic tone, counteracting the sympathetic dominance seen during panic states
- Prefrontal cortical engagement: Mindfulness strengthens activity in brain regions associated with attention regulation and emotional control
Mindfulness-based approaches can be learned through formal programs like MBCT or Mindfulness-Based Stress Reduction (MBSR), as well as through apps, books, and other resources that make these practices increasingly accessible.
Breathing Retraining
Breathing pattern disorders, particularly chronic hyperventilation, frequently accompany panic disorder and may contribute to symptoms like dizziness, tingling sensations, and chest tightness. Breathing retraining techniques aim to normalize respiratory patterns, particularly by slowing the breathing rate and shifting from chest to diaphragmatic breathing.
Research in the Journal of Behavior Therapy and Experimental Psychiatry found that capnometry-assisted breathing training, which provides feedback on carbon dioxide levels to guide breathing regulation, significantly reduced panic symptoms and improved quality of life in individuals with panic disorder.
Simple diaphragmatic breathing exercises, practiced regularly outside of panic episodes and implemented during early signs of panic, can help interrupt the escalation of symptoms. The physiological rationale includes normalization of blood gases (particularly carbon dioxide levels), reduction in physiological arousal, and engagement of the parasympathetic nervous system.
Progressive Muscle Relaxation
Progressive muscle relaxation (PMR) involves systematically tensing and then releasing different muscle groups to achieve a deep state of physical relaxation. This technique can be particularly helpful for individuals with panic disorder who experience significant muscle tension as part of their anxiety response.
A study in the Journal of Clinical Psychology found that PMR, when combined with cognitive interventions, significantly reduced panic symptoms compared to wait-list controls. Regular practice appears to help individuals recognize and counteract tension patterns that may serve as triggers or maintaining factors for panic attacks.
The accessibility of PMR makes it an excellent adjunct to other treatments. Individuals can learn this technique through guided recordings, apps, or in-person instruction, then practice independently as part of a comprehensive self-management approach to panic symptoms.
Lifestyle Factors Affecting Panic Symptoms
Caffeine Reduction
Caffeine sensitivity varies considerably among individuals, but those with panic disorder often show heightened reactivity to this stimulant. Caffeine affects multiple neurotransmitter systems, including adenosine (which it blocks), and indirectly influences dopamine, norepinephrine, and cortisol levels. These effects can mimic or exacerbate many symptoms associated with panic attacks.
Research published in the Archives of General Psychiatry found that caffeine provocation significantly increased anxiety, nervousness, fear, restlessness, and panic in patients with panic disorder compared to healthy controls. Even moderate doses (equivalent to 2-3 cups of coffee) produced panic attacks in a substantial percentage of susceptible individuals.
A caffeine reduction or elimination trial represents a low-risk intervention with potential benefits for panic symptoms. Many individuals report noticeable improvements within days to weeks of reducing caffeine intake, though temporary withdrawal symptoms may occur during this transition period.
Regular Physical Activity
Exercise has demonstrated anxiolytic effects through multiple mechanisms, including increased endorphin production, enhanced GABA function, reduced HPA axis reactivity, and improved sleep quality. For panic disorder specifically, regular physical activity may help reduce both the frequency and intensity of panic attacks.
A randomized controlled trial published in Psychosomatic Medicine found that a 10-week aerobic exercise program significantly reduced anxiety sensitivity (fear of anxiety-related sensations)—a key cognitive factor in panic disorder. Participants also reported fewer panic attacks and less anticipatory anxiety following the intervention.
Interestingly, both moderate-intensity activities (like brisk walking) and higher-intensity interval training have shown benefits for anxiety symptoms. The neurobiological effects appear dose-dependent, with consistent activity over time producing more substantial improvements in mood regulation and stress resilience.
Sleep Optimization
Sleep disturbances frequently co-occur with panic disorder and may serve as both a trigger for and consequence of panic symptoms. Insufficient or poor-quality sleep can increase autonomic instability, enhance threat sensitivity, and impair cognitive control mechanisms that help manage anxiety.
Research in the Journal of Psychiatric Research found that sleep problems predicted the subsequent development of panic attacks, while improving sleep quality was associated with reduced panic frequency and severity. Cognitive-behavioral therapy for insomnia (CBT-I) has shown promise as an adjunctive treatment for panic disorder with comorbid sleep disturbances.
Basic sleep hygiene principles—maintaining consistent sleep-wake times, creating a comfortable sleep environment, limiting evening screen exposure, and establishing relaxing pre-sleep routines—represent foundational strategies for optimizing sleep quality. For individuals with more significant sleep disruption, supplements like melatonin or herbs like valerian root may offer additional benefits, though these should be used with appropriate medical guidance.
Integrating Natural Approaches: Creating a Comprehensive Strategy
While individual natural interventions may offer benefits for panic symptoms, the most effective approach typically involves combining multiple strategies tailored to each person’s specific needs and symptom patterns. This integrated approach recognizes the multifaceted nature of panic disorder and addresses various contributing factors simultaneously.
Personalized Assessment
Before implementing natural interventions, a comprehensive assessment should identify key factors relevant to each individual’s panic symptoms. This may include:
- Nutritional status and dietary patterns
- Sleep quality and potential sleep disorders
- Physical activity levels and autonomic function
- Stress management capabilities and resources
- Specific symptom patterns and triggers
- Comorbid conditions that may influence treatment response
This personalized assessment helps prioritize interventions most likely to address each person’s specific contributing factors, rather than applying a one-size-fits-all approach.
Hierarchical Implementation
Rather than implementing multiple changes simultaneously, a step-wise approach often proves more manageable and allows for clearer evaluation of each intervention’s effects. A typical hierarchy might include:
- Foundation: Optimize sleep, reduce caffeine and alcohol, establish regular physical activity, and address obvious nutritional gaps
- First-line supplements: Consider well-supported options like magnesium, omega-3s, and B-complex vitamins
- Targeted supplements: Add specific herbs or nutrients based on individual symptom patterns
- Mind-body practices: Introduce and gradually build competence in techniques like mindfulness meditation and breathing exercises
- Advanced strategies: Consider more specialized approaches as needed based on response to initial interventions
This staged approach helps prevent overwhelm while building a sustainable foundation for long-term symptom management.
Integration with Conventional Treatment
Natural approaches often work best when integrated thoughtfully with evidence-based conventional treatments like cognitive-behavioral therapy (CBT) and, when appropriate, medication. Potential synergies include:
- Nutritional supplements like omega-3s or magnesium may enhance neurotransmitter function, potentially improving response to medications that target the same systems
- Mind-body practices like mindfulness meditation can complement cognitive therapy techniques, enhancing awareness of thought patterns and bodily sensations
- Exercise and improved sleep may reduce baseline anxiety and stress, making exposure-based treatments more tolerable and effective
- Some supplements may help mitigate side effects of medications, potentially improving adherence and outcomes
Open communication with healthcare providers about all interventions being used is essential to ensure safety and optimize integrated care.
Safety Considerations and Potential Interactions
While many natural approaches offer favorable safety profiles compared to some conventional medications, they still require careful consideration, particularly regarding quality, dosing, potential interactions, and individual factors that may influence safety.
Supplement Quality and Standardization
The quality of nutritional and herbal supplements varies considerably, with potential concerns including:
- Inconsistent active ingredient levels
- Contamination with heavy metals or other toxins
- Adulteration with undeclared pharmaceuticals
- Misidentification or substitution of herbal materials
Choosing products from reputable manufacturers that follow Good Manufacturing Practices (GMP) and ideally have third-party testing can mitigate these risks. For herbal products, standardized extracts with specified levels of active compounds typically provide more consistent effects compared to unstandardized preparations.
Medication Interactions
Several supplements with benefits for panic symptoms may interact with commonly prescribed medications:
- St. John’s Wort can reduce the effectiveness of many medications through induction of hepatic enzymes
- Kava may potentiate the effects of sedatives and anxiolytics
- Some adaptogens may affect blood pressure and interact with antihypertensive medications
- High-dose omega-3 supplements may increase bleeding risk when combined with anticoagulants
Full disclosure of all supplements being used to healthcare providers is essential for identifying potential interactions and ensuring safe integration with conventional treatments.
Special Populations
Certain groups require additional caution when considering natural interventions:
- Pregnant and breastfeeding women should avoid many herbal remedies due to limited safety data
- Individuals with liver or kidney disease may have altered metabolism of certain supplements
- Those with bipolar disorder should use caution with stimulating herbs that could potentially trigger manic episodes
- Children and adolescents may respond differently to supplements compared to adults
Personalized medical advice is particularly important for these populations to ensure safe and appropriate implementation of natural approaches.
Future Directions in Research and Practice
The field of complementary and integrative approaches to panic disorder continues to evolve, with several promising areas for future research and clinical application:
Precision Nutrition and Nutrigenomics
Emerging research suggests that individual genetic variations may influence response to nutritional interventions. For example, polymorphisms in genes related to methylation pathways, neurotransmitter receptors, and inflammatory processes may affect how individuals respond to supplements like B vitamins, omega-3s, and herbal adaptogens.
As testing becomes more accessible and interpretive algorithms improve, tailoring nutritional interventions based on genetic profiles may enhance efficacy and efficiency of supplementation strategies for panic and anxiety disorders.
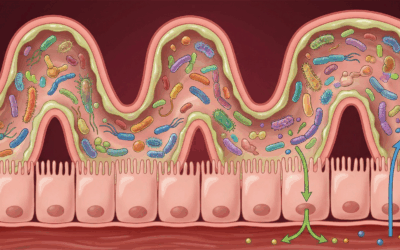
Microbiome-Targeted Interventions
The gut-brain axis represents an exciting frontier in mental health research, with growing evidence for bidirectional communication between gut microbiota and brain function. Studies have identified differences in microbiome composition between individuals with anxiety disorders and healthy controls, suggesting potential for microbiome-targeted interventions.
Prebiotics, probiotics, and dietary patterns that support gut health may ultimately prove valuable in addressing anxiety and panic symptoms through modulation of inflammation, neurotransmitter production, and vagal tone. Research examining specific bacterial strains and their metabolites for anxiety management continues to expand our understanding of these connections.
Technology-Enhanced Delivery of Mind-Body Practices
Digital platforms, wearable devices, and mobile applications offer promising vehicles for delivering mind-body interventions with greater accessibility and personalization. Biofeedback-enhanced breathing practices, app-guided progressive muscle relaxation, and virtual reality-based exposure therapy represent innovative approaches to addressing panic symptoms.
These technology-enabled approaches may prove particularly valuable for individuals with limited access to in-person mind-body instruction or those who benefit from ongoing feedback to optimize their practice.
Conclusion: Balancing Optimism with Realistic Expectations
Natural approaches offer valuable options for individuals seeking to manage panic symptoms, particularly when implemented thoughtfully as part of a comprehensive strategy that may include conventional treatments. The growing evidence base for certain supplements, herbal remedies, and mind-body practices provides reasonable grounds for cautious optimism about their potential benefits.
However, realistic expectations remain essential. Natural interventions typically produce modest effects that develop gradually over weeks to months, rather than the more rapid symptom relief sometimes seen with pharmaceutical approaches. Individual responses vary considerably, and finding the most effective combination of approaches often requires patience and systematic experimentation.
For most individuals with panic disorder, optimal outcomes result from an integrative approach that combines evidence-based conventional treatments with carefully selected natural interventions, personalized lifestyle modifications, and ongoing self-management strategies. This balanced approach leverages the strengths of multiple therapeutic paradigms while minimizing the limitations of any single modality.
By approaching panic disorder through this multifaceted lens—addressing neurobiological factors through nutrition and supplementation, modifying behavioral patterns through lifestyle changes, and developing psychological skills through mind-body practices—individuals can build a robust foundation for lasting symptom improvement and enhanced quality of life.
For more information on supplemens for mental health consult our comprehensive guide for micronutrient and supplement therapy and how it can treat specific issues and enhance certain modalities of therapy.
If you’re interested in exploring micronutrient therapy as part of your anxiety treatment plan, Hardy Nutritionals offers a range of products to fit your specific needs. Their Daily Essential Nutrients clinical strength formula provides comprehensive, research-backed dosages in convenient capsule or powder form.
For 15% off in savings, use the offer code “Taproot” at checkout on the Hardy Nutritionals website to receive 15% off your order. @ GetHardy.com
It’s important to remember that while micronutrient therapy can be a powerful tool for managing anxiety, it is not a replacement for professional mental health care. Always consult with a qualified healthcare provider before starting any new supplement regimen, particularly if you have pre-existing health conditions or are taking medications.
Disclaimer: These statements have not been evaluated by the Food and Drug Administration. These products are not intended to diagnose, treat, cure, or prevent any disease. Please consult with a qualified healthcare professional before beginning any supplement regimen, particularly if you are pregnant, nursing, have a medical condition, or are taking medications. The information on this website doesnot constitute medical advice. We recieve a small commision on sales with Hardy Nutritionals through our offer code. Our affiliation does not effect treatment or recomendations made by Taproot authors, therapists or other staff.
References
- Kessler, R. C., Chiu, W. T., Jin, R., Ruscio, A. M., Shear, K., & Walters, E. E. (2006). The epidemiology of panic attacks, panic disorder, and agoraphobia in the National Comorbidity Survey Replication. Archives of General Psychiatry, 63(4), 415-424.
- Sarris, J., Byrne, G. J., Cribb, L., Oliver, G., Murphy, J., Macdonald, P., … & Ng, C. H. (2019). L-theanine in the adjunctive treatment of generalized anxiety disorder: A double-blind, randomised, placebo-controlled trial. Journal of Psychiatric Research, 110, 31-37.
- Su, K. P., Tseng, P. T., Lin, P. Y., Okubo, R., Chen, T. Y., Chen, Y. W., & Matsuoka, Y. J. (2018). Association of use of omega-3 polyunsaturated fatty acids with changes in severity of anxiety symptoms: A systematic review and meta-analysis. JAMA Network Open, 1(5), e182327.
- Boyle, N. B., Lawton, C., & Dye, L. (2017). The effects of magnesium supplementation on subjective anxiety and stress—A systematic review. Nutrients, 9(5), 429.
- Lakhan, S. E., & Vieira, K. F. (2010). Nutritional and herbal supplements for anxiety and anxiety-related disorders: Systematic review. Nutrition Journal, 9(1), 1-14.
- Sarris, J., Byrne, G. J., Bousman, C. A., Cribb, L., Savage, K. M., Holmes, O., … & Schweitzer, I. (2015). Kava for generalised anxiety disorder: A 16-week double-blind, randomised, placebo-controlled study. Australian & New Zealand Journal of Psychiatry, 49(S1), 36-36.
- Mah, L., Szabuniewicz, C., & Fiocco, A. J. (2016). Can anxiety damage the brain? Current Opinion in Psychiatry, 29(1), 56-63.
- Bandelow, B., Michaelis, S., & Wedekind, D. (2017). Treatment of anxiety disorders. Dialogues in Clinical Neuroscience, 19(2), 93-107.
- Benjamin, J., Levine, J., Fux, M., Aviv, A., Levy, D., & Belmaker, R. H. (1995). Double-blind, placebo-controlled, crossover trial of inositol treatment for panic disorder. American Journal of Psychiatry, 152(7), 1084-1086.
- Carpenter, J. K., Andrews, L. A., Witcraft, S. M., Powers, M. B., Smits, J. A., & Hofmann, S. G. (2018). Cognitive behavioral therapy for anxiety and related disorders: A meta‐analysis of randomized placebo‐controlled trials. Depression and Anxiety, 35(6), 502-514.
- Craske, M. G., & Barlow, D. H. (2007). Mastery of your anxiety and panic: Therapist guide. Oxford University Press.
- Duan, W., & Labuschagne, I. (2019). Implications for neuropsychiatric disorders: Effects of L-theanine on stress-related symptoms and cognitive function. Current Neuropharmacology, 17(5), 374-391.
- Guthrie, S. K., & Stowell, J. (2016). Treatment of panic disorder. Psychiatric Clinics, 39(4), 583-593.
- Hofmann, S. G., Sawyer, A. T., Witt, A. A., & Oh, D. (2010). The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology, 78(2), 169.
- Kennedy, D. O., Little, W., & Scholey, A. B. (2004). Attenuation of laboratory-induced stress in humans after acute administration of Melissa officinalis (Lemon Balm). Psychosomatic Medicine, 66(4), 607-613.

















0 Comments