Dialectical Behavior Therapy
Calm the Emotional Storm
Learn to Recognize and Regulate Emotion
Make Relationships Sustainable and Healthy
Stabilizing
Stage One focuses on stabilizing the individual and achieving behavioral control. This stage addresses and aims to reduce life-threatening behaviors, behaviors interfering with therapy, and behaviors that severely impact quality of life. It involves learning and applying skills to manage distress, regulate emotions, and improve interpersonal relationships.
Healing
Stage Two deals with processing and healing from past trauma. Here, the individual learns to fully experience emotions without needing to escape from them. This stage often involves exposure-based techniques to help clients confront and get past their traumatic experiences, reducing post-traumatic stress.
Achieving Goals

Life-Changing Yet Unintrusive
How is DBT Experiencing Different?
What happens in a DBT Session?
DBT Somatic and Experiential Integration
Dialectical Behavior Therapy: A Transformative Approach
Dialectical Behavior Therapy (DBT) is an innovative therapeutic approach designed to offer relief and healing for a wide range of mental health issues. Grounded in cutting-edge psychological research, this therapy provides a unique path to emotional wellness. Here’s how DBT can be instrumental in treating various conditions:
Stress and Anxiety Disorders:
DBT excels in treating stress and anxiety disorders. It aids individuals in identifying and managing emotional and cognitive aspects related to anxiety, promoting a sense of calm and mental clarity. This process helps in reducing the symptoms of anxiety and managing stress more effectively.
Emotional Trauma and PTSD:
This therapy is highly effective for individuals suffering from emotional trauma and Post-Traumatic Stress Disorder (PTSD). It empowers clients to process and integrate traumatic memories, facilitating a safe and gradual healing process. This approach is crucial in diminishing the impact of traumatic events and easing PTSD symptoms.
Chronic Emotional Distress:
DBT addresses the psychological aspects of chronic emotional distress. By focusing on emotional regulation and distress tolerance, it helps individuals understand and alleviate emotional suffering that may be linked to psychological factors, offering a pathway to emotional relief.
Depression:
For those grappling with depression, DBT offers a therapeutic route to explore and heal underlying emotional pain. This approach assists in processing past hurts and promotes emotional balance, contributing to a significant reduction in depressive symptoms.
Recovery from Emotional Setbacks:
This therapy is beneficial in the recovery process from emotional setbacks or life changes. It aids in managing emotional responses and stress related to these experiences, enhancing the individual’s resilience and coping strategies.
Enhancing Personal Development:
Individuals can benefit from DBT by addressing mental and emotional blocks that impact their personal development. This method aids in overcoming past emotional challenges or life stressors, fostering a stronger mental and emotional growth.
Improving Relationships:
DBT also aids in improving interpersonal relationships. It assists individuals in understanding and resolving emotional patterns from past relationships, leading to healthier and more fulfilling connections.
Dialectical Behavior Therapy offers a comprehensive and effective approach to treating a range of conditions, from mental health issues like anxiety and trauma to personal challenges like emotional distress and relationship problems. Its focus on emotional regulation, mindfulness, and interpersonal effectiveness makes it a versatile and powerful tool for holistic healing and wellness.
We have multiple clinicians availible at Taproot Therapy Collective that treat a wide variety of issues and conditions with training in many techniques and modalities of therapy.
What Does Dialectical Behavior Therapy Feel Like?
In the Therapy Office:
The experience of Dialectical Behavior Therapy (DBT) varies for each individual, as it taps into the mind’s natural ability to heal and manage emotional or psychological stress. In a DBT session, the therapist guides you to tune into your emotions, thoughts, and reactions related to past experiences. Unlike other therapies, there’s no strict chronological timeline; instead, the focus is on the present moment and how your mind processes past traumas and stress.
During the session, you might experience a range of emotions, thoughts, and insights as you connect with and process these mental memories. The therapist gently supports you in navigating these experiences, promoting healing and emotional regulation in a controlled and safe environment.
Out of the Therapy Office:
The impact of DBT often extends beyond the therapy room. You might continue to process emotions and thoughts after the session, leading to deeper insights and shifts in perception. These ongoing experiences are crucial for healing and should be shared in future sessions for further exploration and integration.
As you process these experiences, you may notice various emotional shifts, cognitive changes, and insights. This can include a greater awareness of emotional reactions, new psychological insights, and a changing perspective on past traumas. You might also experience a reduction in symptoms associated with emotional distress, like anxiety or mood fluctuations, as your mind integrates these experiences.
Changes in Emotional and Cognitive Experiences:
DBT is particularly effective in reducing symptoms tied to emotional stress or trauma. As you process and integrate these memories, manifestations such as heightened emotional responses or distress can diminish, demonstrating the deep connection between mind and emotions.
Transformation in Emotional Responses:
Through DBT, emotional responses related to past traumas often become less intense and more manageable. This can lead to improved mental health, with a decrease in symptoms of anxiety, depression, and PTSD.
Enhanced Emotional Awareness:
DBT fosters a heightened awareness of emotional states and thought patterns. This increased awareness can lead to a deeper understanding of how past experiences impact your present emotional and cognitive state, enhancing overall well-being.
Altered Perception of Trauma:
The therapy transforms your relationship with traumatic memories. By focusing on emotional regulation and mindfulness in the present moment, it helps you to recontextualize past traumas, leading to a sense of empowerment and the ability to engage more fully in life.
What Does Dialectical Behavior Therapy (DBT) Feel Like?
In the Therapy Office:
Dialectical Behavior Therapy (DBT) offers a unique experience that differs for each individual, as it engages the mind’s innate capacity to recover and manage emotional or psychological challenges. In a DBT session, the therapist assists you in connecting with your emotions, thoughts, and responses, particularly those linked to past experiences. DBT stands out from other therapies in its lack of a strict chronological focus. Rather, it emphasizes the present moment, concentrating on how your mind and emotions process past difficulties and traumas.
Throughout the session, you might navigate a spectrum of emotions and thoughts, gaining insights as you delve into and make sense of these mental and emotional experiences. The therapist provides gentle, supportive guidance, facilitating a process of healing and emotional regulation within a safe and supportive environment.
Outside the Therapy Office:
The effects of DBT often extend well beyond the confines of the therapy session. You may find yourself continuing to reflect on and process emotions and thoughts after the session, leading to deeper understanding and shifts in how you perceive your experiences. This ongoing internal work is essential for recovery and is beneficial to discuss in subsequent sessions for deeper exploration and further integration.
During this reflective process, you might observe a variety of emotional shifts, cognitive alterations, and newfound insights. These can manifest as an increased awareness of your emotional responses, fresh psychological insights, and evolving perspectives regarding past traumas. Additionally, you may notice a decrease in symptoms commonly associated with emotional distress, such as anxiety or mood fluctuations, as you integrate these experiences.
Impact on Emotional and Cognitive Processes:
DBT is particularly adept at alleviating symptoms related to emotional stress or trauma. As you process and assimilate these experiences, you might observe a reduction in intense emotional reactions or psychological distress, highlighting the profound link between the mind and emotional health.
Transformation of Emotional Responses:
DBT helps in modifying emotional responses associated with past traumas, making them less overwhelming and more manageable. This shift can significantly improve mental health, contributing to a reduction in symptoms of anxiety, depression, and PTSD.
Enhanced Emotional and Cognitive Awareness:
DBT encourages an increased awareness of your emotional states and thought processes. This heightened consciousness can foster a deeper understanding of the influence of past experiences on your current emotional and cognitive condition, promoting overall mental well-being.
Reframing Trauma:
DBT plays a pivotal role in altering your relationship with traumatic memories. By concentrating on emotional regulation and mindfulness in the present, it assists in reinterpreting past traumas, leading to a sense of empowerment and a more active engagement in life.
What are the parts of DBT therapy?
Dialectical Behavior Therapy (DBT) combines cognitive-behavioral techniques with mindfulness practices. It’s particularly effective for treating a range of mental health issues, including borderline personality disorder. Here’s a simplified overview of the main modules and techniques in DBT:
DBT Modules
Mindfulness:
Develops present-moment awareness and acceptance without judgment. This includes skills like observing, describing, and participating mindfully in activities like breathing, walking, and eating. It helps increase self-awareness, reduce impulsiveness, and enhance emotional regulation.
Distress Tolerance:
Focuses on surviving crises and tolerating distress without resorting to self-destructive behaviors. Skills include accepting reality (Radical Acceptance), calming techniques (like paced breathing), and distraction methods. These are crucial for managing extreme emotions and reducing harmful responses to stress.
Emotion Regulation:
Aims to understand and manage intense emotions. Techniques involve identifying and labeling emotions, acting in ways opposite to unhelpful emotions, and solving problems that trigger emotional responses. This leads to more emotional balance and improved relationships.
Interpersonal Effectiveness:
Enhances skills for effective communication and maintaining relationships. This involves being assertive, maintaining self-respect, and managing conflicts in relationships. Skills include learning to describe situations, express needs, and negotiate solutions.
DBT Techniques
Diary Cards:
Clients track their emotions, behaviors, and skill usage daily. This helps in monitoring progress and identifying patterns.
Chain Analysis:
Involves breaking down events to understand the causes of problematic behaviors. It’s a way to learn from mistakes and plan better strategies.
Behavioral Activation:
Encourages doing positive activities to improve mood and combat negative emotions. It involves planning and carrying out these activities.
Validation Strategies:
Acknowledges and accepts clients’ feelings and thoughts. This strengthens the therapist-client relationship and reduces emotional suffering.
Mindfulness Exercises:
Regular practice of mindfulness in daily life. This enhances awareness and acceptance of the present moment.
Exposure Techniques:
Gradually exposes clients to feared situations or emotions to reduce avoidance behaviors and fear.
DBT’s structured approach targets emotional and behavioral challenges, making it beneficial for those struggling with emotional regulation, interpersonal conflicts, and distress tolerance. Its effectiveness in treating various psychological disorders is well-supported by research.
How does DBT change the brain and reconsolidate memory?
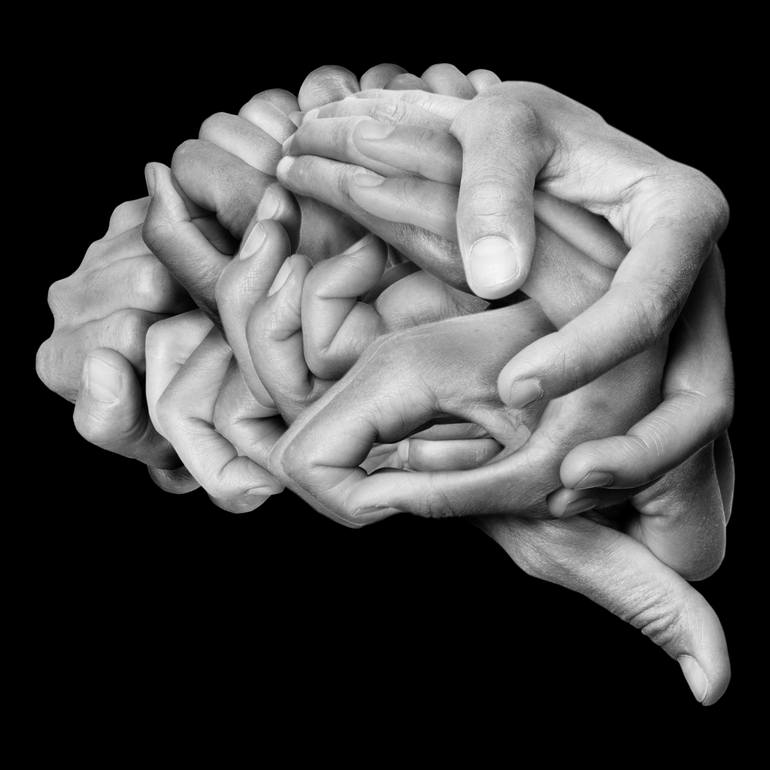
Dialectical Behavior Therapy (DBT) utilizes a whole-brain approach, incorporating principles from cognitive-behavioral therapy and mindfulness to facilitate holistic healing. Here’s how it engages different parts of the brain in the context of improving relationships, managing emotions, and addressing issues like eating disorders, addiction, and personality disorders:
Left Brain:
The left hemisphere, known for logical, analytical, and language-processing capabilities, is engaged in DBT through structured skill-building sessions. These include understanding the interplay between thoughts, emotions, and behaviors, and learning how to apply these skills in everyday life. This logical approach helps clients see the connections between their thoughts, feelings, and actions, particularly in the context of relationships and personal challenges.
Right Brain:
The right hemisphere, involved in emotional processing, creativity, and holistic thinking, is engaged through mindfulness practices and emotional regulation strategies in DBT. Clients learn to acknowledge and validate their emotions without judgment, which is crucial in managing conditions like eating disorders and addiction, where emotional dysregulation is often a core issue.
Mid-Brain:
The mid-brain, including areas like the amygdala and hippocampus that are key in emotional regulation and memory formation, is stimulated in DBT by addressing emotional responses and past traumas. Techniques like distress tolerance and mindfulness help alter the emotional impact of past experiences, contributing to a healthier emotional response system. This is particularly beneficial in addressing emotional aspects of personality disorders.
Frontal Brain:
The frontal lobes, especially the prefrontal cortex, responsible for decision-making, problem-solving, and emotional regulation, are engaged through the skills taught in DBT. These skills help clients make more thoughtful decisions, understand and manage their reactions, and behave in ways that are aligned with their personal values and goals. This is vital in improving interpersonal relationships and tackling impulsive behaviors seen in addiction and certain personality disorders.
DBT’s holistic approach not only promotes mental and emotional healing but also enhances interpersonal relationships and personal development. By addressing the interconnectedness of thoughts, emotions, and behaviors, DBT leads to profound and lasting changes, improving the overall quality of life for individuals struggling with a range of complex issues.
What You Need to Know About DBT
Dialectical Behavior Therapy (DBT) is a therapeutic technique that assists in healing trauma and emotional distress through a structured approach of revisiting life experiences. In DBT sessions, your therapist guides you through various processes including mindfulness, emotional regulation, distress tolerance, and interpersonal effectiveness. These processes may involve reflecting on past memories and experiences, but the focus is primarily on how these experiences impact your current emotional state and behaviors.
Your experience during DBT can be deeply personal and transformative. Many people experience a profound connection between their emotional states and thought patterns. DBT helps in creating a stronger mind-emotion connection, facilitating a healthier way to recognize, process, and integrate emotional trauma. This approach is particularly effective in teaching skills for managing intense emotions, improving relationships, and developing coping strategies for distressing situations.
Anxiety & PTSD
Chronic Depression
Men's & Women's Issues
Anger Management
Childhood Trauma
Sexual Trauma
Chronic Pain & Illness
Dissociation
Addiction & Substance Abuse
Discrimination Trauma
Panic Attacks
Eating Disorders
Mood Disorders
What is the History of Dialectical Behavior Therapy?
Dialectical Behavior Therapy (DBT) was founded by Dr. Marsha M. Linehan, a psychologist and professor at the University of Washington. The development of DBT is a story of innovation, driven by the need to find effective treatment for individuals struggling with complex mental health issues, particularly Borderline Personality Disorder (BPD).
Background of Dr. Marsha M. Linehan
Academic Background:
Dr. Linehan, who has a background in clinical psychology, was acutely aware of the challenges faced by individuals with BPD, including intense emotional pain, self-harming behaviors, and a high rate of treatment dropout.
Personal Motivation:
Dr. Linehan’s work was also influenced by her own struggles with mental health during her youth, which provided her with a deep understanding of the emotional turmoil faced by her clients.
Invention of DBT
Early Observations:
In the late 1970s and early 1980s, while working with clients with BPD, Dr. Linehan observed that conventional cognitive-behavioral therapy (CBT) was not entirely effective. Clients often felt misunderstood and invalidated, leading to high dropout rates and poor treatment outcomes.
Integrating Mindfulness:
Dr. Linehan introduced mindfulness and acceptance strategies into the treatment process, drawing from Eastern meditative practices. This approach aimed to help clients accept and tolerate their intense emotions.
Balancing Acceptance and Change:
A core principle of DBT is the dialectical philosophy, which involves holding two seemingly opposing perspectives at the same time: accepting reality as it is and simultaneously working to change it. This approach was novel in therapeutic settings and proved to be more effective for clients with BPD.
Development of Skills Training:
Dr. Linehan developed a structured skills training approach focusing on four key areas: mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness. These skills were designed to empower clients to manage their emotions, cope with stress, and improve their relationships.
Evolution of DBT
Initial Focus of DBT:
Originally, DBT was specifically designed to treat BPD, particularly for individuals exhibiting self-harming behaviors and suicidal ideation.
Expanding Applications: Over time, the effectiveness of DBT in teaching emotional regulation and distress tolerance led to its application in treating a range of other mental health disorders, including eating disorders, substance abuse disorders, depression, and anxiety.
Legacy of Dr. Linehan and DBT
Research and Recognition:
Dr. Linehan’s work has been widely recognized and supported by extensive research. DBT is now considered one of the most effective treatments for BPD and other complex mental health disorders.
Continued Development of DBT:
Dr. Linehan and other professionals continue to refine and develop DBT, adapting it to new research findings and therapeutic needs.
Global Impact of DBT:
Today, DBT is practiced worldwide, and Dr. Linehan’s contributions have had a significant impact on the field of psychology, offering hope and effective treatment to those struggling with challenging mental health conditions.
Dr. Marsha M. Linehan’s development of DBT stands as a testament to her dedication to finding effective therapeutic solutions for those in need, and her work continues to influence and shape the landscape of mental health treatment globally.
Precursors to DBT and Theoretical Underpinnings
Dialectical Behavior Therapy (DBT) is founded on various psychological theories. Primarily, it is influenced by cognitive-behavioral therapy (CBT), emphasizing the importance of understanding the relationship between thoughts, emotions, and behaviors. DBT also integrates concepts from Eastern mindfulness practices, focusing on present-moment awareness and acceptance. This combination is pivotal in DBT’s approach to managing intense emotions and improving interpersonal relationships.
Philosophical Foundations
Philosophically, DBT adopts a balanced view of accepting current reality while working towards change. It aligns with the principles of dialectical philosophy, which involves holding two seemingly opposite perspectives at once – acceptance and change. This perspective is crucial in helping clients navigate emotional and behavioral challenges.
Integration of Various Modalities
DBT is distinctive in its synthesis of cognitive-behavioral techniques and mindfulness practices. It incorporates strategies for emotional regulation, distress tolerance, mindfulness, and interpersonal effectiveness, enabling clients to develop a comprehensive set of skills for managing their emotions and relationships. Elements of mindfulness practices are integral in DBT, fostering present-moment awareness and non-judgmental acceptance.
Origin of Dialectical Behavior Therapy
DBT was developed by Marsha M. Linehan in the late 1980s. Linehan, drawing upon her experience in clinical psychology, created DBT initially as a method to treat borderline personality disorder (BPD). She recognized that traditional cognitive-behavioral techniques were not fully effective for clients with BPD, leading her to integrate mindfulness practices into the therapeutic process.
Early Development and Principles
Initially, DBT was focused on addressing the challenges of emotional dysregulation, impulsivity, and self-harm behaviors associated with BPD. Linehan’s approach involved teaching clients skills in mindfulness, emotional regulation, distress tolerance, and interpersonal effectiveness. The therapy emphasized balancing acceptance of the client’s experience with the need for change.
Innovative Techniques
A key component of DBT is its skills training aspect, which equips clients with practical strategies to manage emotions, cope with distress, and improve relationships. The use of diary cards for tracking emotions and behaviors, along with group skills training sessions, are unique features of DBT.
Expansion and Contemporary Applications
Over the years, DBT’s application has expanded beyond BPD to treat a variety of mental health issues, including depression, anxiety, eating disorders, and substance abuse. Its holistic approach to addressing emotional, cognitive, and interpersonal challenges makes it a versatile tool for therapy.
Recognition in Research
DBT’s history highlights its effectiveness in combining cognitive-behavioral strategies with mindfulness practices. It is recognized for its practical, empathetic treatment approach, offering significant benefits to those grappling with various mental health challenges. Its place in psychotherapy continues to grow, as evidenced by ongoing research and its widespread application in clinical settings.
The Future of Dialectical Behavior Therapy
With the growing emphasis on comprehensive mental health care, DBT’s balanced approach to addressing both acceptance and change positions it as a crucial component in the field. Its adaptability and effectiveness in treating a range of mental health issues suggest a continuing role in the evolving landscape of psychotherapy. As research expands and new techniques are integrated, DBT will likely continue to adapt and remain a vital tool for therapists and clients alike.
Lifespan Integration FAQs
How Does Dialectical Behavior Therapy Work?
Who invented DBT and why?
Dialectical Behavior Therapy (DBT) was developed by Dr. Marsha Linehan in the late 1980s. Dr. Linehan, a psychologist and researcher at the University of Washington, initially created DBT to treat borderline personality disorder (BPD), a condition characterized by extreme emotional instability, impulsivity, and often, a history of self-harm and suicidal behavior.
The invention of DBT was motivated by Dr. Linehan’s observation that traditional cognitive-behavioral therapy (CBT) was not fully effective for clients with BPD. CBT often emphasizes change, such as altering thoughts and behaviors, which could sometimes be invalidating or overwhelming for individuals with intense emotional experiences. Dr. Linehan sought to address this gap by incorporating acceptance and mindfulness strategies into the treatment approach.
The “dialectical” aspect of DBT comes from the integration of these two key elements: acceptance and change. This approach helps clients to both accept themselves and their experiences while simultaneously working on changing harmful behaviors. DBT also focuses heavily on building and applying skills in areas such as emotion regulation, distress tolerance, interpersonal effectiveness, and mindfulness, which are critical for individuals with BPD and other similar psychological disorders.
What does DBT feel like?
Experiencing Dialectical Behavior Therapy (DBT) can vary significantly from person to person, but there are some common elements that many clients report. Here’s a general idea of what it might feel like to engage in DBT:
-
Structured and Skill-Focused: DBT is highly structured, and much of the therapy involves learning and practicing new skills. Clients often appreciate this practical, skills-based approach because it provides clear guidance and tools that can be applied in everyday life.
-
Challenging but Empowering: DBT challenges clients to confront and change harmful behaviors and thought patterns. This process can be difficult and may evoke strong emotions, but many find it ultimately empowering as they develop greater control over their emotions and actions.
-
Balancing Acceptance and Change: DBT places a strong emphasis on accepting oneself and one’s current situation. This acceptance, combined with efforts to change, can feel like a validating and balanced approach, helping clients to acknowledge their worth while recognizing the need for change.
-
Supportive Group and Individual Sessions: DBT typically includes both individual therapy sessions and group skills training sessions. The group aspect can provide a sense of support and solidarity, as clients learn from and with others who have similar struggles. Individual sessions offer personalized guidance and support from a therapist.
-
Focus on Mindfulness: Many clients find the focus on mindfulness in DBT to be grounding and calming. Mindfulness practices can help in developing a greater awareness of the present moment and a more balanced perspective on emotions and thoughts.
-
Regular Homework Assignments: Homework is a key component of DBT, where clients practice the skills learned in sessions in their daily lives. This can make the therapy feel very hands-on and relevant to real-life situations.
-
Emotionally Intensive: Since DBT often involves working through intense and difficult emotions, sessions can sometimes feel emotionally draining. However, over time, many clients report a decrease in emotional suffering and an increase in emotional regulation.
-
A Sense of Progress and Achievement: As skills are mastered and applied effectively, clients often experience a sense of progress and achievement, which can be very rewarding.
-
Safe Space for Vulnerability: DBT creates a safe and non-judgmental space for clients to explore and express their vulnerabilities, which can be both challenging and healing.
It’s important to remember that therapy is a highly individual experience, and what one person feels in DBT may be different from another’s experience. The effectiveness and experience of DBT can also depend on the individual therapist, the specific issues being addressed, and the client’s own engagement with the therapy process.
Where Does DBT Fit into Treatment?
Dialectical Behavior Therapy (DBT) fits into mental health treatment in several significant ways:
-
Treating Borderline Personality Disorder (BPD): DBT was originally developed to treat BPD, a condition characterized by difficulty in regulating emotions, impulsivity, unstable relationships, and a chronic sense of emptiness. DBT is considered one of the most effective treatments for BPD.
-
Managing Self-Harm and Suicidal Behaviors: DBT is particularly effective in reducing self-harm behaviors and suicidal ideation, which are often present in individuals with BPD and other severe mental health disorders.
-
Treating Mood Disorders: DBT has been adapted to treat mood disorders, especially for individuals who have not responded well to other treatments. It’s beneficial in managing intense emotional swings and impulsive behaviors associated with these disorders.
-
Addressing Substance Abuse and Eating Disorders: DBT’s skills in emotional regulation, distress tolerance, and interpersonal effectiveness make it suitable for treating issues like substance abuse and eating disorders, where emotional dysregulation plays a significant role.
-
Helping with Trauma-Related Disorders: While not a first-line treatment for PTSD, DBT can be helpful in stabilizing individuals and helping them manage self-destructive behaviors before they engage in trauma-focused therapy.
-
Improving Emotional Regulation and Interpersonal Skills: DBT’s focus on skills training is beneficial for anyone struggling with emotional regulation or interpersonal relationships, regardless of a formal mental health diagnosis.
-
Supplementing Other Therapies: DBT can be used in conjunction with other forms of therapy, such as Cognitive Behavioral Therapy (CBT) or psychodynamic therapy, to enhance emotional regulation and skills training.
-
Group and Individual Settings: DBT’s flexibility allows it to be delivered in both individual therapy sessions and group skills training sessions, catering to different therapeutic needs and preferences.
-
Crisis Intervention: The skills taught in DBT, particularly those related to distress tolerance and mindfulness, are effective for crisis intervention and helping individuals cope with immediate stressors.
-
Long-Term Mental Health Maintenance: Beyond acute treatment, DBT skills can contribute to long-term mental health maintenance, helping individuals lead more stable and fulfilling lives.
DBT is a versatile therapy that can be adapted to a wide range of psychological issues and disorders. Its comprehensive approach, which combines cognitive-behavioral techniques with mindfulness principles, makes it a valuable tool in modern mental health treatment.
“When we are grounded in our awareness, we can be more present with what we are experiencing in our bodies — in all the spaces that live between our head and our feet.”
― Raegan Robinson
What Therapies are Similar to Dialectical Behavior Therapy (DBT)?
Dialectical Behavior Therapy (DBT) shares similarities with several other therapeutic modalities like Cognitive Behavioral Therapy (CBT), Acceptance and Commitment Therapy (ACT), Mindfulness-Based Cognitive Therapy (MBCT), Schema Therapy, and Eye Movement Desensitization and Reprocessing (EMDR). Here’s a comparison:
Cognitive Behavioral Therapy (CBT):
Similar to CBT, DBT is rooted in cognitive-behavioral principles, focusing on the interplay between thoughts, emotions, and behaviors. Both therapies aim to change harmful thinking patterns and behaviors, but DBT places more emphasis on emotional regulation and interpersonal effectiveness, along with the concept of mindfulness and acceptance.
Acceptance and Commitment Therapy (ACT):
DBT and ACT both incorporate mindfulness and acceptance strategies. ACT emphasizes accepting thoughts and feelings without judgment and committing to actions aligned with personal values, similar to DBT’s focus on balancing acceptance and change. However, DBT provides more structured skills training, especially in the areas of emotional regulation and interpersonal relationships.
Mindfulness-Based Cognitive Therapy (MBCT):
MBCT, like DBT, integrates mindfulness practices into cognitive therapy. Both aim to prevent relapse in depression and improve emotional regulation, but DBT has a broader scope, including specific skills for distress tolerance and interpersonal effectiveness, and it’s used for a wider range of psychological issues.
Schema Therapy:
Schema Therapy and DBT both address deep-rooted patterns or schemas. While Schema Therapy focuses on identifying and changing these long-standing patterns and themes in a person’s life, DBT offers more concrete skills and strategies for managing emotions and improving relationships in the here-and-now.
Eye Movement Desensitization and Reprocessing (EMDR):
Both EMDR and DBT are used in the treatment of trauma and PTSD. While EMDR focuses on desensitizing and reprocessing traumatic memories through bilateral stimulation, DBT provides a broader set of skills for managing distress, regulating emotions, and improving interpersonal relationships, which can be beneficial in a trauma-informed treatment approach.
How does Dialectical Behavior Therapy (DBT) Stimulate the Subcortical Brain?
Dialectical Behavior Therapy (DBT) engages the subcortical brain areas, such as the amygdala, hippocampus, and thalamus, which are crucial for emotional regulation and memory. This engagement is facilitated through various DBT techniques like mindfulness, emotional regulation exercises, and distress tolerance skills. Mindfulness practices in DBT help in calming the mind and bringing awareness to the present moment, which can positively affect the amygdala, known for its role in fear and emotional responses. Emotional regulation techniques aim to modify intense emotional reactions, potentially influencing the hippocampus, involved in forming and retrieving memories, especially those linked with emotions. The distress tolerance skills taught in DBT help in managing and coping with emotional pain, which might indirectly affect the thalamus, involved in processing and relaying sensory information to other parts of the brain. The repeated practice of these skills in DBT can contribute to changes in the brain’s emotional processing areas, leading to improved emotional control and psychological resilience over time.
How does DBT Affect the Basal Ganglia?
Dialectical Behavior Therapy (DBT), through its comprehensive approach to emotional and psychological well-being, might indirectly impact the basal ganglia, a group of nuclei in the brain associated with a variety of functions including motor control, emotions, and cognitive processing. DBT’s emphasis on stress reduction, emotional regulation, and mindfulness could lead to a decrease in stress-related neurotransmitters and hormones, potentially benefiting the basal ganglia’s functioning. For instance, as DBT techniques reduce anxiety and stress, they might help in normalizing the neurotransmitter levels, which are crucial for the basal ganglia’s role in emotional and cognitive processing. However, it’s important to note that the direct effects of DBT on specific brain structures, like the basal ganglia, are a subject of ongoing research, and the outcomes may vary among individuals. Further studies are required to explore these neurobiological impacts in detail.
FAQ about Dialectical Behavior Therapy (DBT)
Can DBT Be Used on Children?
Yes, Dialectical Behavior Therapy (DBT) can be adapted and used effectively with children and adolescents. DBT for younger populations is modified to suit their developmental level, cognitive abilities, and emotional needs. It is particularly beneficial for children who struggle with emotional regulation, experience intense emotional responses, or exhibit behavioral issues. In sessions tailored for children, techniques might include age-appropriate skill-building activities, games, and possibly family involvement to reinforce the skills learned in therapy.
How Does DBT Differ from Other Therapies?
DBT is unique in its synthesis of cognitive-behavioral techniques with mindfulness principles, focusing on both acceptance and change. It is distinct in its structured approach, involving both individual therapy and group skills training. The core components of DBT – mindfulness, distress tolerance, emotional regulation, and interpersonal effectiveness – are specific to this modality, setting it apart from therapies that may focus more exclusively on cognitive restructuring (like traditional CBT) or trauma processing (like EMDR).
What If DBT Doesn’t Seem to Work?
If DBT doesn’t seem to be effective, it’s important to discuss this with your therapist. They may adjust their approach or suggest integrating other therapeutic techniques. Remember that therapy is a personal and evolving process; self-care practices and a supportive environment can enhance the effectiveness of therapy. Healing takes time, and being patient with yourself and the process is crucial. If necessary, seeking a second opinion or exploring alternative therapeutic options is also advisable.
It’s essential to recognize that therapy’s effectiveness can vary from person to person. Collaborating closely with a qualified therapist is essential in identifying and pursuing the most suitable approach for your needs.
List of Notable Dialectical Behavior Therapy (DBT) Practitioners
Dr. Marsha Linehan
Dr. Marsha Linehan is the founder and original developer of Dialectical Behavior Therapy. She is a key figure in the field of psychology, particularly for her work in treating borderline personality disorder (BPD) and chronic suicidal ideation. Linehan’s contributions through her research, writings, and development of DBT have been fundamental in advancing the treatment of BPD and other disorders characterized by emotional dysregulation.
Dr. Alec Miller
Dr. Alec Miller is a well-known psychologist who has specialized in adapting DBT for adolescents. His work in this area has been influential in addressing the unique challenges faced by this age group, particularly those with emotional and behavioral dysregulation. Miller’s contributions include developing treatment protocols, training materials, and clinical research in adolescent DBT.
Dr. Jill Rathus
Dr. Jill Rathus has co-authored significant literature on DBT, especially in its application to adolescents. She is recognized for her expertise in integrating DBT with treatment for teenagers and young adults, focusing on issues such as self-harm, suicidal behaviors, and emotion regulation difficulties.
Dr. Charles Swenson
A prominent psychiatrist and DBT expert, Dr. Charles Swenson has been instrumental in promoting and teaching DBT. His work includes training therapists in DBT, contributing to research, and advancing the understanding of how DBT can be effectively applied in various clinical settings.
Dr. Kelly Koerner
Dr. Kelly Koerner is known for her contributions to DBT, especially in training and treatment innovations. She has played a significant role in disseminating DBT knowledge and skills to practitioners and has contributed to the literature on effective implementation of DBT in therapy.
Dr. Melanie Harned
Dr. Melanie Harned is recognized for her work in integrating DBT with trauma-focused treatments. Her research and clinical practice have significantly contributed to understanding how DBT can be effectively used in treating individuals with complex trauma and PTSD.
