What is AuDHD?
Attention Deficit Hyperactivity Disorder (ADHD) and Autism Spectrum Disorder (ASD) are two distinct neurodevelopmental conditions that frequently co-occur. Recent research suggests that 50-70% of autistic individuals also have ADHD, and two-thirds of those with ADHD may have co-existing conditions like autism. When someone has both autism and ADHD, it’s often referred to as AuDHD.
The Diagnostic Evolution of AuDHD
Despite the high co-occurrence, it wasn’t until relatively recently that AuDHD could be diagnosed. Prior to the release of the DSM-5 in 2013, the diagnostic criteria did not allow for co-diagnosis of autism and ADHD. They were considered mutually exclusive conditions.
This diagnostic separation meant that research before 2013 only studied autism and ADHD in isolation, potentially skewing findings if a significant portion of study participants unknowingly had both conditions. It also resulted in many individuals, especially those diagnosed before 2013, only receiving one diagnosis even if they met criteria for both.
The DSM-5’s allowance for co-diagnosis reflects an improved understanding of the overlap and distinctions between autism and ADHD. However, the two conditions are still frequently treated separately in clinical practice. The ICD (International Classification of Diseases) tends to align more closely with clinical realities, being based on behavior and objective measurements.
The Neurological Complexity of AuDHD
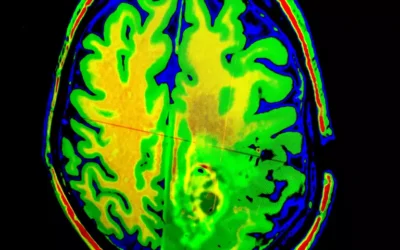
Brain imaging techniques like QEEG brain mapping suggest that the behaviors we label as “ADHD” may actually arise from 5-6 distinct neurological processes. In other words, the same outward symptoms could stem from multiple conditions with shared behavioral manifestations. This may explain the wide variation in how individuals respond to different treatments.
AuDHD introduces additional neurological complexity. What looks like a single condition based on observable traits may involve multiple underlying processes that are difficult to untangle. This has significant implications for understanding lived experiences and developing effective supports.
The Push-Pull of Opposing Traits
AuDHD is often described as feeling like a tug-of-war in the brain. The traits associated with autism and ADHD can directly conflict with each other, creating an exhausting internal struggle:
- Autism craves routine and sameness, while ADHD seeks novelty and spontaneity
- Autism is prone to sensory overload, while ADHD desires stimulation
- Autism enables deep focus on specific interests, while ADHD causes distraction and impulsivity
These contradictory traits can result in:
- Difficulty maintaining organization despite a strong desire for order
- Periods of intense focus followed by struggles with attention and follow-through
- Anxiety when deviating from routines, even when bored by those same routines
- Sensory sensitivities coupled with a need for stimulation to regulate
- Social challenges related to missing cues, oversharing, and feeling like an “outcast”
The constant effort to satisfy competing needs can be disorienting and depleting. As another person shared: “I want to be systematic and precise but struggle with it, which leaves me constantly feeling not good enough.”
Gender Differences in Presentation
AuDHD traits can manifest differently across genders, adding to the diagnostic complexity:
- Autistic girls and women are more likely to camouflage or mask their traits, leading to missed or late diagnosis
- ADHD is often overlooked in girls because their symptoms tend toward inattention rather than stereotypical “hyper” behavior
- Women with AuDHD describe intense difficulties with emotional regulation, household management, and parenting demands
These differences contribute to misunderstanding and delayed support. Many women in particular express feeling invalidated, misdiagnosed with other conditions, or like they’ve “failed” at being neurotypical before recognizing their AuDHD.
Rethinking Treatment for AuDHD
Traditional therapies for autism and ADHD are not always well-equipped to address the unique needs of AuDHD. While medication and standard behavioral interventions can help manage certain symptoms, they may not get to the neurological roots or adequately support the whole person.
Emerging approaches offer new hope:
- Cognitive Behavioral Therapy (CBT) and Dialectical Behavioral Therapy (DBT) teach specific skills for emotional regulation, distress tolerance, and navigating social demands
- Occupational therapy addresses sensory integration and adaptive living skills
- Brainspotting and neurofeedback aim to “rewire” the brain and process underlying traumas that exacerbate executive dysfunction
QEEG brain mapping is also a promising assessment tool to better pinpoint an individual’s precise neurological differences and customize treatment.
Alongside these clinical supports, AuDHD-informed accommodations in school and work settings are essential. These may include sensory-friendly environments, organizational tools, social skills groups, and flexibility with communication and productivity styles.
Just as important is helping AuDHD individuals understand and accept their unique brain wiring. Unmasking, self-advocacy, and connection with other neurodivergent people can be powerfully validating and healing.
The Gifts of an AuDHD Mind
Though the challenges of AuDHD are significant, this intersection of neurotypes also confers distinct strengths:
- Creativity and outside-the-box thinking
- Ability to hyperfocus and persist on personally meaningful projects
- Rich inner world and vivid imagination
- Empathy, compassion, and attunement to emotions
- Honesty and aversion to “fakeness”
- Keen observation skills and appreciation of details and patterns
- Dedication to social justice and making the world better
When AuDHDers have insight into their needs and access to the right supports, these gifts can truly shine. As one person expressed: “If I’m given the space, I can do wonderful things.”
Embracing the AuDHD Experience
AuDHD is a complex neurotype that cannot be reduced to its individual components of autism and ADHD. It is a unique way of perceiving, thinking, and engaging with the world that comes with both struggles and strengths.
Understanding AuDHD requires a holistic view of a person’s traits and how they interact. It means moving beyond the pathology paradigm to appreciate neurodiversity. And it demands advocacy to reshape environments to be more inclusive and affirming of all kinds of minds.
For AuDHD individuals, self-understanding is critical. Connecting the dots between one’s lived experiences and this neurotype can be revelatory and empowering.
If you resonate with the above descriptions, consider pursuing an assessment with a neurodiversity-affirming provider. Remember that no two AuDHD individuals are alike, and your particular constellation of characteristics is valid and valuable.
You are not alone, and supports are available to help you better understand and meet your needs. Embrace all that your marvelous mind has to offer. AuDHD may be challenging, but it is also a gift.
Strategies for Managing AuDHD Traits in Daily Life
While professional support is important for thriving with AuDHD, there are also many strategies individuals can implement in their daily lives to work with their unique brains:
- Create “structured flexibility.” Establish loose routines that have some constants but also allow for choice and variation. Build in sensory and movement breaks.
- Find the right environments. Look for spaces that balance your needs for both stimulation and quiet, familiarity and novelty. Don’t be afraid to make accommodations.
- Use visual organizers. Calendars, color-coding, lists, and reminders can help compensate for executive functioning difficulties. Experiment to find what works for you.
- Communicate your needs. Let trusted people know what you struggle with and what helps you. Practice scripts for setting boundaries and advocating for accommodations.
- Leverage special interests. Bring elements of your fascinations into mundane tasks to boost motivation. Let yourself get absorbed as a way to recharge.
- Prioritize self-discovery. Read, listen to podcasts, join online communities to deepen your understanding of AuDHD and connect with relatable experiences.
Reframing Disability and Appreciating Neurodiversity
A key part of living well with AuDHD is releasing stigma and internalizing a positive neurodivergent identity. This doesn’t mean denying disability – AuDHD is disabling in many ways. But it does mean locating that disability in a society not built for neurodivergent brains, rather than as an individual flaw.
The neurodiversity paradigm asserts that diversity in brain wiring is a natural and valuable form of human variation. It challenges the notion that there is one “right” way to think, learn, and behave. Through this lens, AuDHD is a minority neurotype rather than a disorder.
Connecting with the broader neurodivergent community can foster disability pride, normalize challenges, and expand access to resources and representation. It can help shift the narrative from “I’m broken” to “My brain works differently, and that’s okay.”
AuDHD and Intersectionality
AuDHD does not exist in a vacuum. Like any neurotype, it intersects with a person’s other identities and experiences – race, ethnicity, gender, sexuality, socioeconomic status, disability, trauma history.
Being neurodivergent and part of another marginalized group often creates a double bind, where neither community feels fully accessible or affirming. Discrimination in clinical and educational settings leads to underdiagnosis and undertreatment. Cultural differences in how neurodevelopmental conditions are understood and treated also impact people’s experiences and access to support.
Additionally, rates of gender diversity are much higher in the autistic and ADHD communities than in the general population. Being neurodivergent and transgender and/or non-binary can involve added layers of social navigation and self-advocacy.
These intersections highlight the need for culturally responsive, affirming care and for uplifting diverse AuDHD voices. True inclusion means considering the whole person.
AuDHD Across the Lifespan
Like any neurotype, AuDHD shows up differently in different stages of life. Many people, especially those with more subtle traits, make it to adulthood without ever receiving a formal diagnosis. Others may have been identified as children but struggled to get support that fit.
Common challenges in adulthood include:
- Executive dysfunction interfering with higher education and/or employment
- Difficulty maintaining stable relationships and social connections
- Higher risk for anxiety, depression, and substance use
- Delayed “launching” and feeling behind peers in reaching milestones
At the same time, AuDHD adults often have a breadth of knowledge, skills, and life experiences to draw from. Diagnosis and self-understanding can be a catalyst for making empowered changes and accessing accommodations. Many people find their niche in fields that complement their strengths and interests.
Midlife and beyond can bring new concerns like aging parents, changes in career and family roles, and cognitive shifts. It’s never too late to seek diagnosis and support. In fact, many older adults find self-advocacy gets easier with time and practice.
Supporting Loved Ones with AuDHD
If someone you care about is AuDHD, educating yourself is an important first step. Learn about what AuDHD really means, common myths and misconceptions, and how it impacts your loved one specifically.
Some tips for being a supportive ally:
- Believe them. AuDHD is an invisible disability and its consequences can be hard for outsiders to see. Trust your loved one’s experiences, even if you can’t always relate.
- Balance structure and flexibility. Offer support with creating a predictable environment, while staying open to accommodating fluctuating needs.
- Communicate openly and regularly. Make space for both of you to share challenges and needs. Resist giving unsolicited advice.
- Celebrate strengths. Point out what you see and admire about how your loved one’s mind works. Remind them of their unique value and abilities.
Innovative Treatment Approaches for AuDHD
While medication and traditional talk therapy can help manage some AuDHD symptoms, they often fail to address the underlying neurological differences and emotional wounds that can accompany this neurotype. Fortunately, several cutting-edge treatment approaches are showing promise for better supporting AuDHD individuals.
Brainspotting and Emotional Transformation Therapy
Brainspotting is an innovative brain-body-based therapy that helps individuals process unresolved trauma and emotional distress. Developed by Dr. David Grand, this approach is based on the understanding that where we focus our eyes can affect our neurophysiology and reveal key “brainspots” holding traumatic memories.
During a brainspotting session, the therapist guides the client to focus on a specific external point while simultaneously attending to their internal experience. This dual awareness can help unlock and resolve stuck emotional patterns, leading to profound psychological healing.
For AuDHD individuals, brainspotting can be particularly powerful for addressing the chronic stress and feelings of inadequacy that often accompany navigating a neurotypical world. By releasing this emotional baggage, AuDHDers can experience greater self-acceptance, emotional regulation, and ability to harness their cognitive strengths.
Dialectical Behavior Therapy (DBT)
Dialectical Behavior Therapy (DBT) is a skills-based approach that helps individuals regulate intense emotions, tolerate distress, communicate effectively, and practice mindfulness. Originally developed by Dr. Marsha Linehan for treating borderline personality disorder, DBT has since been adapted for a range of conditions involving emotional dysregulation.
For AuDHDers, DBT can be a game-changer for managing the mood swings, impulsivity, and interpersonal conflicts that often arise from co-occurring autism and ADHD traits. The DBT skill of “wise mind” – balancing emotion and logic – can be particularly helpful for AuDHDers caught between competing neurological needs.
Other key DBT strategies include:
- Mindfulness practices to increase self-awareness and reduce reactivity
- Distress tolerance techniques like self-soothing and radical acceptance
- Emotion regulation skills such as identifying triggers and reframing thoughts
- Interpersonal effectiveness tools for setting boundaries and communicating needs
By building these core competencies, AuDHD individuals can experience greater emotional stability and resilience.
Cognitive Behavioral Therapy (CBT)
Cognitive Behavioral Therapy (CBT) is a well-established treatment that helps individuals identify and change unhelpful thought patterns and behaviors. CBT is based on the understanding that our thoughts, emotions, and actions are interconnected – by shifting one, we can impact the others.
For AuDHD, CBT can be useful for:
- Challenging negative self-talk and cognitive distortions related to living with a stigmatized neurotype
- Building behavioral coping strategies for executive functioning difficulties
- Developing social skills and scripts for navigating neurotypical environments
- Implementing lifestyle changes to better accommodate sensory and attentional needs
CBT’s emphasis on concrete, present-focused problem-solving can be a good fit for AuDHD individuals who struggle with abstract thinking and staying motivated.
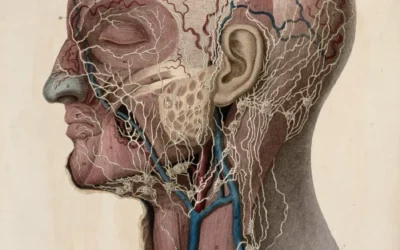
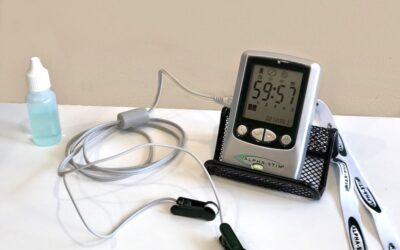
QEEG Brain Mapping and Neurostimulation
Quantitative electroencephalography (QEEG) is a non-invasive brain imaging technique that measures electrical activity in the brain. By mapping this activity, clinicians can identify patterns associated with various neurological conditions, including AuDHD.
QEEG brain mapping can be a valuable assessment tool for pinpointing an individual’s specific cognitive strengths and challenges. This information can then guide more targeted treatment planning, such as:
- Neurofeedback training to increase focus and emotional regulation
- Transcranial magnetic stimulation (TMS) to modulate brain activity in underactive regions
- Personalized cognitive training exercises to strengthen specific skills
By directly addressing the neurological underpinnings of AuDHD, these brain-based interventions can complement and enhance the effects of therapy and medication.
The Evolution of AuDHD Understanding: A Timeline
Our understanding of AuDHD as a unique neurotype has developed over several decades. Here are some key milestones:
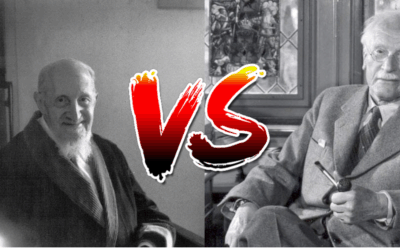
- 1902: Sir George Still describes “an abnormal defect of moral control in children.” He notes cases of impulsive behavior and difficulties with sustained attention. This is often cited as the first scientific description of what we now know as ADHD.
- 1943: Leo Kanner publishes a paper outlining the characteristics of “autistic disturbances of affective contact.” This is considered the first formal description of autism.
- 1944: Hans Asperger describes a group of children with similar traits to Kanner’s descriptions, but with strong verbal skills and intense special interests. This later becomes known as Asperger’s Syndrome.
- 1960s-1970s: Autism and ADHD are conceptualized as distinct conditions. Autism is understood as a form of childhood psychosis, while ADHD is seen as minimal brain dysfunction.
- 1980: DSM-III is published, establishing autism and ADHD as separate diagnoses. However, the criteria for each are quite narrow compared to current understandings.
- 1987: DSM-III-R broadens the criteria for autism and ADHD, reflecting evolving clinical insights. However, it still does not allow for dual diagnosis.
- 1994: DSM-IV further expands diagnostic criteria for autism and ADHD but maintains that they cannot be diagnosed together. Asperger’s Syndrome is added as a distinct diagnosis on the autism spectrum.
- 2013: DSM-5 is published, merging all subcategories into a single diagnosis of Autism Spectrum Disorder (ASD). It also, for the first time, allows for co-diagnosis of ASD and ADHD.
- 2010s-present: Research increasingly explores the overlap and intersection of autism and ADHD. Studies reveal high rates of co-occurrence and shared genetic and neurological underpinnings.
- 2018: “AuDHD” and “AutiADHD” emerge as popular terms within online neurodivergent communities to capture the distinct experiences of having both autism and ADHD.
- 2020s-present: Clinicians, researchers, and self-advocates push for greater recognition of AuDHD as a unique neurotype requiring tailored supports. Neurodiversity-affirming resources and treatment approaches expand.
This timeline represents significant progress in our understanding of neurodevelopmental differences. However, much work remains to fully appreciate and support the diversity of the AuDHD experience. Ongoing research, improved diagnostic tools, and first-hand insights from AuDHD individuals will continue to shape our evolving understanding.
Online Resources
General ADHD Resources
- CHADD (Children and Adults with Attention-Deficit/Hyperactivity Disorder)
- Website: CHADD
- Provides education, advocacy, and support for individuals with ADHD.
- ADDitude
- Website: ADDitude
- Offers articles, expert advice, and strategies for managing ADHD.
- National Institute of Mental Health (NIMH) – ADHD
- Website: NIMH
- Research-based information about ADHD.
- ADDA (Attention Deficit Disorder Association)
- Website: ADDA
- Focuses on adult ADHD, offering resources and community support.
General ASD Resources
- Autism Speaks
- Website: Autism Speaks
- Comprehensive resources on autism, including toolkits, research, and advocacy.
- Autistic Self Advocacy Network (ASAN)
- Website: ASAN
- An organization run by and for autistic individuals, promoting self-advocacy.
- National Autism Center
- Website: National Autism Center
- Focuses on evidence-based practices for autism.
- Autism Society
- Website: Autism Society
- Provides resources, advocacy, and support for individuals and families affected by autism.
Combined ADHD and ASD Resources
- Understood
- Website: Understood
- A resource for learning and attention issues, including ADHD and ASD.
- ADHD & Autism Resource Center
- Website: ADHD & Autism Resource Center
- Offers tools and support specifically for those with both ADHD and autism.
Books
ADHD
- “Driven to Distraction” by Edward M. Hallowell and John J. Ratey
- A classic book on ADHD covering symptoms, treatments, and strategies.
- “The ADHD Effect on Marriage” by Melissa Orlov
- Discusses the impact of ADHD on relationships and offers practical advice.
- “Smart But Stuck” by Thomas E. Brown
- Features stories and insights about adults with ADHD.
Autism
- “The Reason I Jump” by Naoki Higashida
- An insightful memoir by a non-verbal autistic teen.
- “Uniquely Human: A Different Way of Seeing Autism” by Barry M. Prizant
- Offers a compassionate perspective on understanding autism.
- “NeuroTribes: The Legacy of Autism and the Future of Neurodiversity” by Steve Silberman
- Explores the history of autism and the neurodiversity movement.
Combined ADHD and ASD
- “The ADHD and Autism Connection” by Diane M. Kennedy and Rebecca S. Banks
- Focuses on the overlap of ADHD and autism, offering practical strategies.
- “Uniquely Wired: A Story About Autism and Its Gifts” by Julia Cook
- A children’s book that provides insight into autism.
Articles and Research
- “The Overlap Between ADHD and Autism” – Psychology Today
- Link: Psychology Today Article
- Discusses common traits and differences between ADHD and autism.
- “Understanding the Intersection of ADHD and Autism” – ADDitude
- Link: ADDitude Article
- Explores how ADHD and autism can co-occur.
- “Is ADHD a Risk Factor for Autism?” – National Center for Biotechnology Information (NCBI)
- Link: NCBI Research
- A research article examining the relationship between ADHD and autism.
Support Groups and Community Resources
- ADHD Support Groups (Local Chapters)
- Find local support groups through CHADD or ADDA.
- Autism Support Groups
- Many local autism organizations offer support groups for individuals and families.
- Facebook Groups
- Search for ADHD or autism-focused groups for peer support and community.
Apps and Tools
- Todoist
- Task management app that helps with organization, great for ADHD.
- Evernote
- Note-taking app that helps with organization and keeping track of information.
- MindNode
- Mind-mapping tool to help visualize thoughts and ideas.
- Social Skills Apps (e.g., “Social Express”)
- Helps individuals with autism develop social skills through interactive scenarios.



















0 Comments