Alabama Therapists’ Complete Regulatory and Financial Survival Guide 2025
Critical Updates for Practice Sustainability in an Era of Unprecedented Change
Alabama therapists face transformative regulatory changes in 2025 that require immediate attention to paperwork, compliance procedures, and practice operations. The landscape has fundamentally shifted with the introduction of Lucet as BCBS Alabama’s behavioral health manager, Senate Bill 101’s medical consent age changes, the transition from Drug Courts to Accountability Courts, and the devastating impact of the One Big Beautiful Bill Act’s $824 million annual Medicaid cuts to Alabama. Combined with Medicare reimbursement rates for mental health billing decreasing by approximately 14% in 2025, therapists must implement comprehensive documentation and strategic adaptations to survive this complex regulatory and financial storm.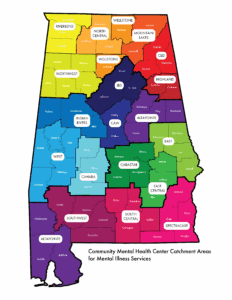
PART I: IMMEDIATE CRISIS MANAGEMENT – THE LUCET REVOLUTION
Understanding the BCBS-Lucet Partnership Impact
Blue Cross and Blue Shield of Alabama has partnered with Lucet as their business associate, transferring all behavioral health services management to this independent company. This represents the most significant operational change for Alabama therapists since the implementation of electronic health records, affecting every aspect of BCBS interactions. The partnership places Lucet in control of authorization processes, utilization review, case management, and Applied Behavior Analysis services for all BCBS behavioral health clients.
Lucet utilizes specific medical necessity criteria including the Level of Care Utilization System (LOCUS) to evaluate behavioral health treatment requests. Your documentation must now align with LOCUS standards rather than traditional BCBS criteria. This fundamental shift requires comprehensive revision of treatment planning, progress documentation, and authorization request procedures for all BCBS clients.
All BCBS behavioral health services now require pre-authorization through Lucet’s system rather than direct BCBS authorization. Documentation must include detailed clinical justification using LOCUS criteria, specific treatment goals with measurable outcomes, evidence-based treatment modality justification, and clear demonstration of medical necessity at the requested level of care. The authorization process now involves multiple steps including initial screening, clinical review, and potential peer-to-peer consultations with Lucet clinical staff.
Therapists must contact Lucet Provider Relations at 1-888-611-6285 for information on becoming a behavioral health network provider. Existing BCBS contracts may not automatically transfer to Lucet network participation, requiring new credentialing processes and contract negotiations. Provider enrollment with Lucet involves separate applications, credentialing verification, and network participation agreements distinct from original BCBS contracts.
Why This Change Is Happening and Its Long-Term Implications
The shift to Lucet represents a nationwide trend of insurance companies outsourcing behavioral health management to specialized third-party companies to reduce costs and standardize care protocols. For Alabama therapists, this change reflects BCBS’s strategy to control behavioral health expenses through enhanced utilization management and standardized treatment protocols. Lucet’s primary function is reducing behavioral health costs for BCBS while maintaining compliance with mental health parity requirements.
This transition introduces standardized treatment protocols that may reduce flexibility in treatment approaches and session frequencies. Therapists will face enhanced utilization review processes requiring more frequent treatment plan reviews and justifications for continued care. The system emphasizes data analytics oversight where treatment patterns are analyzed for compliance with cost-effective care models and adherence to evidence-based practice standards.
The change also reflects broader healthcare industry consolidation trends where specialized companies manage specific service categories to achieve economies of scale and standardized care delivery. For Alabama therapists, this means adapting to corporate-style utilization management rather than the more flexible approach traditionally used by BCBS Alabama.
Implementation Requirements and Timeline
By September 15, 2025, therapists must contact Lucet Provider Relations to verify network status and begin any necessary credentialing processes. All BCBS authorization procedures must be updated to route through Lucet’s system rather than traditional BCBS channels. Treatment plan templates require revision to incorporate LOCUS criteria and enhanced medical necessity justification language. Staff training on new authorization and appeals processes becomes mandatory to avoid service interruptions.
By October 1, 2025, practices must implement enhanced documentation requirements for all BCBS clients, incorporating LOCUS criteria and Lucet-specific clinical justification standards. Direct communication channels with Lucet case managers must be established to facilitate authorization processes and address utilization review questions. Tracking systems for Lucet-specific authorization timelines become essential, as processing times may differ significantly from previous BCBS procedures. Contingency plans for authorization delays or denials require development to maintain continuity of care for clients.
Essential Compliance Resources Lucet Provider Relations: 1-888-611-6285 | Lucet Website: https://lucethealth.com/ | Provider Resources: https://lucethealth.com/providers/resources/ | Network Application: https://lucethealth.com/providers/resources/process-guidance/ | BCBS Provider Portal: https://providers.bcbsal.org/portal/web/pa/login | BCBS Behavioral Health: https://providers.bcbsal.org/portal/resources/-/resources/category/1082899
PART II: SENATE BILL 101 – MEDICAL CONSENT AGE CRISIS
The Fundamental Change in Minor Treatment
Senate Bill 101 represents a seismic shift in how therapists provide services to minors, increasing the age of medical consent from 14 to 16 years old and introducing sweeping parental involvement requirements that fundamentally alter therapeutic relationships with adolescent clients. The legislation affects all medical, dental, and mental health services, creating new consent requirements for clients aged 14-15 who previously could consent to their own treatment.
The bill introduces specific restrictions on school-based mental health services, requiring enhanced parental consent for mental health interventions in public school settings. These requirements create significant barriers to crisis intervention and ongoing support services for adolescents who may be experiencing family conflict, abuse, or other situations where parental involvement could be harmful or contraindicated.
Current therapeutic relationships with clients aged 14-15 require immediate review and potential restructuring to comply with new consent requirements. Therapists must obtain parental consent for continued treatment where previously the minor’s consent was sufficient. This change affects confidentiality protocols, emergency treatment procedures, and the fundamental therapeutic alliance with adolescent clients who may have initially sought services independently.
Every intake form, consent document, and treatment agreement requires comprehensive revision to comply with new age-based consent requirements. Documentation must now capture parental involvement in treatment decisions and consent processes for all clients under 16. The change also affects billing procedures, as parental consent may be required for insurance claims processing for services to 14-15 year olds.
Operational Impact and Client Relationship Management
This legislative change will significantly impact practices serving adolescent populations by reducing the number of self-referring teenage clients and increasing administrative burden for consent management. Many adolescents aged 14-15 who previously accessed mental health services independently may discontinue treatment if parental involvement is required, particularly in cases involving family dysfunction, abuse, or other sensitive issues.
The change potentially disrupts established therapeutic relationships where parental involvement could be contraindicated or harmful to the therapeutic process. Therapists must navigate the complex balance between legal compliance and clinical best practices when parental involvement conflicts with the adolescent’s therapeutic needs or safety.
Administrative burden increases substantially as practices must implement new procedures for obtaining, documenting, and maintaining parental consent for 14-15 year old clients. This includes developing protocols for situations where parents are divorced, separated, or have complex custody arrangements affecting consent authority.
Implementation Protocol and Risk Management
Immediate actions required by September 1, 2025 include reviewing all current clients aged 14-15 for consent compliance and obtaining parental consent for continued treatment where required. All intake and consent forms require revision to reflect new age requirements, and staff need training on new consent procedures and documentation requirements to avoid liability exposure.
Client transition protocols must include scripts for discussing consent changes with current teenage clients and procedures for obtaining retroactive parental consent where legally required. Practices need established protocols for clients who refuse parental involvement or where parental involvement could create safety concerns for the adolescent client.
Documentation of all consent-related conversations and decisions becomes critical for legal protection and compliance verification. Practices must maintain detailed records of attempts to obtain parental consent, client responses to consent requirement changes, and clinical decisions made regarding continued treatment in complex consent situations.
🔗 Essential Compliance Resources: Alabama Legislature Official Site: http://www.legislature.state.al.us/aliswww/default.aspx | SB 101 Full Text: https://alison.legislature.state.al.us/files/pdf/SearchableInstruments/2025RS/SB101-enr.pdf | Bill Tracking: https://alison.legislature.state.al.us/SearchableInstruments/2025RS/BillSearch.aspx | Alabama Board of Medical Examiners SB 101 Info: https://www.albme.gov/press-release/al-sb-101-would-raise-medical-age-of-consent-from-14-to-16
PART III: THE ONE BIG BEAUTIFUL BILL ACT, CBD REGULATIONS, AND CASCADING FINANCIAL DEVASTATION
The CBD and Hemp Regulatory Revolution
House Bill 445, signed into law by Governor Kay Ivey on May 14, 2025, and effective July 1, 2025, fundamentally transforms Alabama’s approach to CBD and hemp products with direct implications for mental health practitioners and their clients. The bill explicitly bans smokable hemp products and certain psychoactive cannabinoids but defines “consumable hemp product” broadly as any finished product intended for human or animal consumption that contains any part of the hemp plant or its derivatives.
Under the proposed legislation, hemp-derived products would be restricted to individuals 21 and older, THC content would be capped at 5 milligrams per serving, and marketing targeted at minors would be banned. The bill also establishes a 7% excise tax, licensing fees for manufacturers, wholesalers, creating a comprehensive regulatory framework that affects how therapists discuss and document client use of these products.
The new regulations create specific documentation requirements for therapists whose clients use CBD or hemp products for anxiety, depression, or other mental health conditions. Smokable hemp and CBD products including flower buds and vapes will soon be banned in Alabama, requiring therapists to update treatment plans that previously incorporated or acknowledged client use of these now-prohibited products.
Client Education Requirements Under HB 445
Therapists must now educate clients about the legal changes affecting their access to CBD and hemp products. The age restriction to 21 years old significantly impacts adolescent and young adult clients who may have been using CBD products for anxiety or sleep issues. Documentation must reflect discussions about legal alternatives and the transition away from now-prohibited smokable products.
The 5-milligram THC cap per serving creates new parameters for discussing product potency with clients. Therapists need updated knowledge about legal product limits to provide accurate information during treatment planning. Clients using products exceeding these limits must be informed about compliance requirements and potential legal consequences.
Treatment plans incorporating CBD or hemp products require revision to reflect current legal parameters. Documentation must demonstrate awareness of HB 445 requirements and include client education about legal compliance. Progress notes should track client responses to product availability changes and document any adjustments to treatment approaches necessitated by regulatory changes.
🔗 Essential Compliance Resources: Centers for Medicare & Medicaid Services: https://www.medicare.gov/coverage/mental-health-care-outpatient | Alabama Medicaid Agency: https://medicaid.alabama.gov/content/10.0_Contact/10.3_Provider_Contacts.aspx | Alabama Department of Mental Health: https://mh.alabama.gov/ | Congressional Budget Office: https://www.cbo.gov/ | Alabama Alcoholic Beverage Control Board: https://alabcboard.gov/ | Alabama Department of Agriculture CBD Info: https://agi.alabama.gov/ | HB 445 Full Text: http://www.legislature.state.al.us/aliswww/default.aspx
Understanding Federal Medicaid Cuts and Systemic Impact
President Trump signed the One Big Beautiful Bill Act (OBBB) into law on July 4, 2025, implementing a 15% reduction in federal Medicaid funding totaling $1 trillion over 10 years. Alabama faces losing $824 million in annual Medicaid funding, potentially eliminating healthcare coverage for hundreds of thousands of Alabama residents who rely on federally funded programs. The Congressional Budget Office estimates that the OBBB will remove at least 10.5 million people from Medicaid and CHIP programs by 2034, with 11.8 million people losing health insurance coverage over the next decade.
This dramatic reduction in Medicaid funding creates a cascade effect throughout Alabama’s healthcare system that extends far beyond Medicaid providers. Hospitals and healthcare systems that previously relied on Medicaid reimbursement for a significant portion of their patient population will face substantial revenue reductions, forcing them to shift costs to other payer sources to maintain financial viability.
The elimination of Medicaid coverage for hundreds of thousands of Alabamians creates an unprecedented burden on emergency departments, community health centers, and safety net providers who cannot legally turn away patients requiring emergency care regardless of insurance status. These uncompensated care costs must be absorbed somewhere in the healthcare system, ultimately affecting all providers and payers through cost-shifting mechanisms.
The Ripple Effect on Private Insurance and Commercial Payers
Hospitals and healthcare systems absorbing increased uncompensated care costs from formerly Medicaid-covered patients will shift these expenses to Americans covered by marketplace plans and private insurance through higher premiums and reduced benefit coverage. Commercial insurance premiums are projected to increase 10-15% annually as providers negotiate higher reimbursement rates to offset uncompensated care losses.
Private insurance plans will implement more restrictive prior authorization requirements and reduced mental health benefits to control costs in response to overall healthcare cost inflation driven by Medicaid cuts. Even therapists who never accepted Medicaid will experience reduced reimbursements from commercial payers as insurance companies seek to control expenses across all service categories.
The reduction in Medicaid mental health services will overwhelm community mental health centers and public sector providers, creating increased demand for private practice services from clients who cannot afford full private pay rates. This demand pressure combined with reduced commercial insurance reimbursements creates an impossible financial situation for many private practices.
Ten-Year Economic Projection for Alabama Mental Health Services
The first three years following OBBB implementation (2025-2027) will create immediate crisis conditions with a 15% reduction in clients served through Medicaid programs and a 20-30% increase in requests for uninsured services. Private insurance premium increases of 10-15% annually will make commercial coverage unaffordable for many middle-income families, expanding the uninsured population beyond those directly affected by Medicaid cuts. Practice consolidation will begin as smaller independent practices become financially unsustainable under reduced reimbursement conditions.
Years four through six (2028-2030) will see market adjustment as the healthcare system adapts to permanently reduced federal funding. The community mental health system will become overwhelmed and underfunded as state resources prove insufficient to replace federal Medicaid dollars. Private practice mental health services will become increasingly limited to higher-income clients who can afford full private pay rates or premium insurance coverage with adequate mental health benefits.
The final phase (2031-2034) will establish a new healthcare landscape where mental health services are primarily delivered through integrated healthcare systems that can absorb uncompensated care costs across multiple service lines. Independent private practices will serve primarily affluent populations, while the majority of Alabamians will receive mental health services through consolidated healthcare systems, federally qualified health centers, or limited volunteer and charity-based programs.
PART IV: ENHANCED ACCOUNTABILITY COURTS DOCUMENTATION REQUIREMENTS
Critical Legislative Changes Requiring Immediate Documentation Updates
The Alabama Legislature has fundamentally restructured the state’s approach to criminal justice-involved mental health services through the renaming and expansion of Drug Courts to Accountability Courts. This change, formalized through House Bill 360 and Senate Bill 200, carries the official title of the Honorable Pete Johnson Alabama Drug Offender Accountability Court Act, honoring retired Jefferson County District Court Judge Pete Johnson who pioneered drug courts in Alabama.
For therapists, this transformation requires comprehensive documentation updates. The expanded scope now encompasses not only substance abuse cases but also individuals with mental illness, veterans with PTSD, and those facing unemployment-related criminal justice involvement. Your intake forms must now include specific screening questions to identify clients who may qualify for Accountability Court diversion programs. These questions should address military service history, trauma exposure, employment status, and the relationship between mental health symptoms and any criminal justice involvement.
Treatment plans for Accountability Court participants require new language reflecting the court’s dual emphasis on accountability and rehabilitation. Documentation must demonstrate how your therapeutic interventions address both the mental health needs and the accountability requirements established by the court. Progress notes should explicitly track compliance with court mandates, attendance patterns, engagement levels, and specific behavioral changes related to the client’s accountability plan.
Regional Mental Health Authority Board Reforms (SB 236)
Senate Bill 236, sponsored by Senator Will Barfoot, reforms the governance of regional mental health authority boards, creating new requirements that directly impact how therapists interact with these crucial funding and oversight bodies. The legislation mandates that each executive committee delegated by a regional mental health authority board must include at least one active sheriff and one active judge of probate, fundamentally changing the decision-making structure for mental health services across Alabama.
These boards govern the community mental health centers that serve as designated points of entry for mental health and substance use disorder services in Alabama. The 310 Boards system, which includes centers such as AltaPointe Health, Cahaba Center for Mental Health, and JBS Mental Health Authority, will now operate under reformed governance structures that may affect referral patterns, funding allocations, and service requirements.
Therapists must update their referral agreements and memorandums of understanding with these centers to reflect the new governance structures. Documentation should acknowledge the enhanced role of law enforcement and probate judges in mental health service oversight. This change particularly affects involuntary commitment procedures, as probate judges now have increased influence over the systems that process these cases.
School Psychologist Interstate Licensure Compact (SB 61/HB 214)
The Alabama Board of Examiners in Psychology’s entry into the School Psychologist Interstate Licensure Compact represents a significant shift in how school-based mental health services operate across state lines. This compact allows school psychologists to have equivalent licenses in member states, creating new opportunities and requirements for documentation.
School-based therapists must update their credentialing files to reflect compact participation status. Client consent forms require revision to address the possibility of interstate consultation and the sharing of records across state lines under compact provisions. Privacy notices must explain how the compact affects information sharing and specify which states participate in the agreement.
Administrative Relocations and Procedural Changes
The Alabama Board of Examiners in Counseling’s relocation from its current location to 2740 Zelda Road, third floor, effective June 26, 2025, requires updates to all correspondence addresses, return envelopes, and contact information in client documentation. The Board emphasizes that during the transition period from June 23-25, 2025, email communication should be prioritized as remote phone access will be unavailable.
This physical relocation coincides with administrative rule updates affecting application procedures. The Board maintains authority under Administrative Rule 255-X-4-.06 to require additional academic work, supervised experience, references, or clarifications of intent of practice when questions arise about an applicant’s competence. Documentation systems must accommodate potential requests for supplementary materials during licensure renewal or supervision processes.
🔗 Essential Compliance Resources: Alabama Administrative Office of Courts: https://www.alacourt.gov/ | Alabama District Attorneys Association: http://www.adaa-alabama.org/ | Alabama Department of Veterans Affairs: https://va.alabama.gov/vets-treatment-courts/ | Alabama Department of Mental Health Court Services: https://mh.alabama.gov/
PART V: MEDICARE AND MEDICAID DOCUMENTATION REQUIREMENTS
Medicare Reimbursement Documentation Adaptations
The 14% Medicare reimbursement reduction demands meticulous documentation to maximize remaining reimbursements. The national reimbursement rate for CPT Code 90791 decreases from $195.46 in 2024 to $166.91 in 2025, requiring precise coding to capture all billable services. Documentation must justify the medical necessity of each service with greater specificity than previous years.
Progress notes require enhanced detail demonstrating measurable therapeutic progress to support continued treatment authorization. The Medicare Economic Index projects a 3.5% rise in service provision costs despite frozen reimbursement rates, necessitating documentation that supports efficiency without compromising quality. Each session note must clearly articulate the specific intervention provided, the client’s response, and the clinical rationale for continued treatment.
Medicaid Coverage Limitations and Documentation Strategies
Alabama Medicaid’s restriction of mental health counseling coverage to individuals under 21 creates unique documentation challenges. Alabama Medicaid covers mental health counseling by therapists for children and people under 21, but not for other adults, requiring careful age verification and eligibility documentation.
For clients approaching their 21st birthday, transition planning documentation becomes critical. Files must include detailed discharge planning beginning at least six months before aging out of coverage, documentation of referrals to alternative funding sources, and clear communication with clients about coverage termination. Consider developing a standardized transition protocol that includes timelines for notification, alternative payment arrangements, and continuity of care planning.
Federal Medicaid Changes and State Responses
The federal “One Big Beautiful Bill Act” (H.R.1) mandates a 15% cut in federal Medicaid funding, or $1 trillion, over 10 years, with projected loss of coverage for 11.8 million individuals nationally. Alabama’s share of these cuts could reach $824 million annually, necessitating documentation that positions your practice for survival regardless of Medicaid’s future.
Documentation must now include multiple funding source verifications for each client. Create systematic tracking of primary, secondary, and tertiary payment sources. Implement sliding scale documentation that clearly demonstrates financial need while maintaining sustainability. Develop written policies for transitioning clients between funding sources as coverage changes occur.
🔗 Essential Compliance Resources: Alabama Medicaid Agency: https://medicaid.alabama.gov/content/10.0_Contact/10.3_Provider_Contacts.aspx | Centers for Medicare & Medicaid Services: https://www.medicare.gov/coverage/mental-health-care-outpatient | Healthcare Revenue Integrity Association: https://hcmarketplace.static.hcprostage.com/national-association-of-healthcare-revenue-integrity | Healthcare Financial Management Association: https://www.hfma.org.uk/
PART VI: TELEHEALTH REGULATORY COMPLIANCE AND DOCUMENTATION
Alabama Telehealth Requirements Under Act 2022-302
Alabama’s comprehensive telehealth regulations, effective since July 11, 2022, continue to evolve in 2025 with specific documentation requirements for mental health providers. The law defines telehealth as the use of electronic and telecommunications technologies for medical care delivery, with mental health services receiving special exemptions from certain in-person follow-up requirements.
Consent documentation for telehealth services must be obtained before service delivery, with special requirements for minors. Parents or legal guardians must attend telehealth visits for clients under the age of medical consent. Your consent forms must specify the technology platform used, security measures implemented, and acknowledgment of telehealth-specific limitations.
The DEA’s extension of COVID-19 prescribing flexibilities through December 31, 2025, allows continued prescription of Schedule II-V controlled substances via telehealth without initial in-person evaluation, but documentation must demonstrate compliance with all applicable requirements. Maintain detailed records of the telehealth platform used, verification of patient identity and location, and specific clinical justifications for telehealth versus in-person treatment.
Interstate Practice Considerations
While Alabama participates in various interstate compacts, therapists must document their authorization to practice across state lines carefully. The state allows limited practice without an Alabama license for irregular or infrequent services (less than ten days per calendar year or ten patients per calendar year), but exceeding these limits requires full licensure.
Documentation must track out-of-state client contacts meticulously to avoid inadvertent violations. Implement a monitoring system that alerts you when approaching the ten-day or ten-patient thresholds. For regular interstate practice, maintain separate files demonstrating compliance with each state’s requirements.
🔗 Essential Compliance Resources: Alabama Department of Public Health: https://www.alabamapublichealth.gov/ | DEA Prescribing Guidelines: https://telehealth.hhs.gov/providers/telehealth-policy/prescribing-controlled-substances-via-telehealth | Alabama Medical Board: https://www.albme.gov/ | Psychology Interjurisdictional Compact: https://psypact.gov/ | State Psychology Boards Association: https://www.asppb.net/
PART VII: BUILDING ADAPTIVE DOCUMENTATION SYSTEMS
Electronic Health Records Optimization
The convergence of regulatory changes demands sophisticated electronic health records (EHR) systems capable of managing multiple compliance requirements simultaneously. Your EHR must accommodate Accountability Court reporting requirements, Medicare coding changes, Medicaid age-based eligibility tracking, and telehealth-specific documentation needs.
Configure automated alerts for critical compliance deadlines including license renewals, continuing education requirements, client age-based coverage changes, and interstate practice limitations. Implement templates that ensure consistent capture of required elements for different funding sources and referral pathways. Create custom reports that demonstrate compliance with various regulatory requirements without manual compilation.
Billing System Adaptations
The 14% Medicare reimbursement reduction combined with varying commercial insurance rates requires sophisticated billing system management. Documentation must support maximum reimbursement under tightened criteria. Implement pre-authorization tracking that documents medical necessity with enhanced specificity. Create denial management protocols that systematically address common rejection reasons with supporting documentation.
Track reimbursement rates by payer and CPT code to identify trends and optimize service delivery. Document time spent on administrative tasks to support potential future advocacy for administrative burden compensation. Maintain detailed records of underpayments or delayed payments to support contract negotiations or payer disputes.
Quality Assurance Documentation
Implement measurement-based care documentation that demonstrates treatment effectiveness despite reduced resources. Select validated outcome measures appropriate for your client population and funding sources. Document baseline scores, treatment targets, and progress toward goals using standardized metrics that satisfy both clinical and administrative requirements.
Create quality improvement documentation that shows proactive practice enhancement. Track patient satisfaction, treatment completion rates, and functional improvements. Document how reduced reimbursements affect service delivery and patient outcomes to support advocacy efforts and grant applications.
🔗 Essential Compliance Resources: Healthcare IT Resources: https://www.healthit.gov/ | HIPAA Security Rule: https://www.hhs.gov/hipaa/for-professionals/security/ | Alabama Board of Examiners in Counseling: https://abec.alabama.gov/licensees/
PART VIII: STRATEGIC PLANNING DOCUMENTATION FOR PRACTICE SUSTAINABILITY
Financial Resilience Planning
Develop written financial plans that account for continued reimbursement reductions and potential Medicaid elimination. Document multiple revenue scenarios ranging from status quo to worst-case Medicaid elimination. Create contingency plans with specific triggers for implementing cost reduction measures or service modifications.
Maintain detailed documentation of practice expenses correlated with reimbursement rates. Track the growing gap between service delivery costs and reimbursements to support future rate negotiations and advocacy efforts. Document attempts to negotiate better rates with payers, including proposal submissions and payer responses.
Workforce Development Documentation
The expansion of Accountability Courts and reformed mental health authority boards creates new opportunities for specialized practice. Document staff competencies in areas relevant to expanded court services including trauma-informed care, veterans’ mental health, and integrated treatment for co-occurring disorders.
Create professional development plans that position your practice for emerging opportunities. Document supervision provided to associate licensed counselors, tracking hours toward the 3,000-hour requirement for full licensure. Maintain records of continuing education that exceeds minimum requirements, demonstrating commitment to excellence despite financial pressures.
Community Partnership Agreements
Formalize relationships with referral sources through written agreements that reflect new regulatory requirements. Document collaborative relationships with primary care providers, understanding that integrated care models may become necessary for financial survival. Create memorandums of understanding with Accountability Courts specifying service expectations and reporting requirements.
Develop written protocols for involuntary commitment procedures that acknowledge the enhanced role of sheriffs and probate judges under SB 236. Create clear documentation pathways for cases requiring civil commitment, ensuring compliance with statutory requirements while maintaining therapeutic relationships.
🔗 Essential Compliance Resources: Alabama Psychological Association: https://www.alapsych.org/ | Social Workers Alabama: https://www.socialworkers.org/chapters/alabama | Alabama Department of Mental Health: https://mh.alabama.gov/
PART IX: COMPLIANCE MONITORING AND RISK MANAGEMENT
Regulatory Compliance Tracking Systems
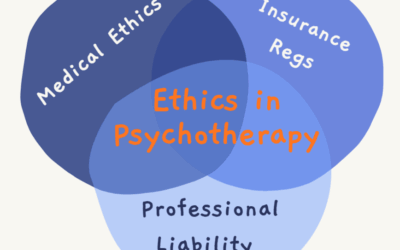
Implement comprehensive compliance tracking that addresses multiple regulatory bodies simultaneously. The Alabama Board of Examiners in Counseling requires 40 hours of continuing education biennially with 6 hours in ethics for LPCs. The Board of Examiners in Marriage and Family Therapy maintains separate requirements. Document completion of requirements well before deadlines to avoid practice interruptions.
Create audit trails for all compliance activities. Document not just completion but also the process of maintaining compliance. Maintain correspondence with regulatory boards, including routine renewals and any requests for additional information. Keep copies of all submitted materials and confirmation receipts.
Professional Liability Management
The changed landscape increases professional liability exposure. Document risk management activities including professional liability insurance reviews, coverage limit assessments, and claim prevention strategies. Maintain detailed incident documentation protocols that protect both client welfare and practice interests.
Create written policies addressing the unique risks of Accountability Court participation, telehealth delivery, and interstate practice. Document staff training on these policies with signed acknowledgments of understanding. Implement regular policy reviews that incorporate regulatory changes and lessons learned from near-miss incidents.
Ethical Decision-Making Documentation
The pressure of reduced reimbursements and expanded service demands creates ethical challenges requiring careful documentation. Create written protocols for managing situations where optimal treatment exceeds available funding. Document ethical consultations when facing dilemmas between financial sustainability and client needs.
Maintain records of pro bono services provided, demonstrating commitment to access despite financial pressures. Document decisions to terminate services due to non-payment, ensuring compliance with ethical obligations for continuity of care. Create clear policies for sliding scale determinations that balance accessibility with sustainability.
🔗 Essential Compliance Resources: Alabama Board of Examiners in Counseling: https://abec.alabama.gov/licensees/ | Phone: (334) 420-7229 | New Address: 2740 Zelda Road, Third Floor, Montgomery, AL 36106 | License Search: https://abec.alabama.gov/licensee-search/ | Marriage & Family Therapy Board: https://mft.alabama.gov/ | Psychology Board: https://al.accessgov.com/abepmain | Administrative Rules: https://admincode.legislature.state.al.us/administrative-code/255
PART X: PREPARING FOR FUTURE LEGISLATIVE CHANGES
Anticipated Regulatory Developments
The 2025 legislative session has already produced significant changes, with more likely as the session continues. Monitor proposed legislation affecting mental health services, particularly bills addressing rural healthcare access, workforce development, and funding mechanisms. Document how proposed changes would affect your practice to enable rapid response when legislation passes.
Track federal healthcare policy developments that could affect Alabama. The potential for additional Medicaid cuts, Medicare Advantage expansion, and value-based payment models requires ongoing preparation. Create flexible documentation systems that can accommodate new requirements without complete overhaul.
Advocacy Documentation
Compile data demonstrating the impact of reimbursement cuts and regulatory changes on service delivery. Document specific cases where funding limitations prevented optimal treatment, maintaining appropriate de-identification for privacy compliance. Create compelling narratives that illustrate the human impact of policy decisions while protecting client confidentiality.
Prepare testimony materials for legislative hearings and regulatory comment periods. Document practice-level data that supports policy arguments including client demographics, service utilization patterns, and outcome metrics. Maintain relationships with professional associations that aggregate individual practice data for systemic advocacy.
Innovation and Adaptation Records
Document innovations implemented in response to regulatory and financial pressures. Track the effectiveness of new service delivery models, technology implementations, and operational efficiencies. Create case studies of successful adaptations that could be replicated by other practices or scaled within your own organization.
Maintain records of failed experiments and lessons learned. Document why certain approaches did not work, saving time and resources in future adaptation efforts. Share learnings with professional communities while protecting proprietary practice advantages.
🔗 Essential Compliance Resources: Alabama Legislature: http://www.legislature.state.al.us/aliswww/default.aspx | Bill Tracking: https://alison.legislature.state.al.us/SearchableInstruments/2025RS/BillSearch.aspx | Governor’s Office: https://governor.alabama.gov/ | Committee Information: http://www.legislature.state.al.us/aliswww/default.aspx
PART XI: IMPLEMENTATION TIMELINE AND ACTION STEPS
Immediate Actions (By September 1, 2025)
Update all correspondence to reflect the Alabama Board of Examiners in Counseling’s new address at 2740 Zelda Road, third floor. Revise intake forms to capture Accountability Court eligibility factors including military service, trauma history, and employment status. Implement Medicare documentation requirements reflecting the 14% reimbursement reduction with enhanced medical necessity justification.
Review and update all telehealth consent forms to ensure compliance with current regulations and DEA prescribing flexibility extensions. Create age-tracking systems for Medicaid-covered clients approaching 21 to enable smooth coverage transitions. Establish baseline metrics for financial performance under reduced reimbursement rates to track impact over time.
Contact Lucet Provider Relations to verify BCBS network status and begin any necessary credentialing processes. Implement Senate Bill 101 compliance procedures for clients aged 14-15, including parental consent requirements and updated documentation protocols. Begin staff training on all new regulatory requirements to ensure smooth transitions.
Short-Term Implementations (September-December 2025)
Develop comprehensive referral agreements with reformed regional mental health authority boards reflecting new governance structures. Create Accountability Court participation protocols including documentation templates and reporting procedures. Implement measurement-based care systems that demonstrate treatment effectiveness despite resource constraints.
Negotiate updated contracts with commercial payers reflecting Medicare reimbursement trends and Lucet authorization requirements. Develop alternative revenue streams including private pay packages, corporate contracts, and grant-funded services. Create workforce development plans that position staff for emerging opportunities in specialized service areas.
Establish direct communication channels with Lucet case managers and implement enhanced documentation requirements for all BCBS clients. Create tracking systems for Lucet-specific authorization timelines and develop contingency plans for authorization delays or denials.
Medium-Term Objectives (January-June 2026)
Evaluate the effectiveness of documentation system changes implemented in response to 2025 regulatory changes. Refine procedures based on audit results and operational experience. Expand successful service innovations while discontinuing unsuccessful experiments.
Prepare for potential additional Medicaid cuts by diversifying funding sources and improving operational efficiency. Strengthen community partnerships that provide referral streams independent of traditional insurance reimbursement. Develop specialized expertise in areas aligned with Accountability Court expansion and reformed mental health governance structures.
Long-Term Strategic Positioning (July 2026 and Beyond)
Position practice for value-based payment models that reward outcomes rather than service volume. Create sophisticated data systems that demonstrate cost-effectiveness and quality outcomes. Build reputation as a leader in adaptive practice management despite challenging reimbursement environments.
Develop succession planning that ensures practice sustainability beyond individual practitioner involvement. Create systems and protocols that maintain compliance and quality regardless of staff changes. Build practice value that transcends current reimbursement challenges through innovation, efficiency, and demonstrated effectiveness.
🔗 Essential Compliance Resources: 988 Suicide & Crisis Lifeline: 988 | https://988lifeline.org/ | NAMI Alabama: https://namialabama.org/ | Professional Liability Insurance: Contact your provider | Legal Consultation: Contact healthcare attorneys
Essential Compliance Resources and Contact Information
The 2025 regulatory landscape presents Alabama therapists with unprecedented challenges requiring comprehensive documentation updates, strategic planning, and operational adaptation. The introduction of Lucet as BCBS Alabama’s behavioral health manager, Senate Bill 101’s consent age changes, the transformation of Drug Courts to Accountability Courts, and the devastating impact of the One Big Beautiful Bill Act’s Medicaid cuts demand immediate action to ensure practice survival and continued service to vulnerable populations.
Success requires more than reactive compliance; it demands proactive transformation of practice operations, documentation systems, and strategic positioning. Therapists who view these changes as opportunities for innovation rather than merely obstacles to overcome will be best positioned for long-term success. The documented commitment to quality care despite financial pressures, demonstrated through comprehensive compliance systems and outcome tracking, will distinguish sustainable practices from those unable to adapt.
The path forward requires courage to make difficult decisions, creativity to develop new service models, and commitment to maintaining therapeutic excellence despite resource constraints. By implementing the documentation updates and strategic planning outlined in this guide, Alabama therapists can navigate the current challenges while building foundations for future success. The need for mental health services in Alabama has never been greater, and therapists who adapt effectively to the new landscape will continue serving their communities while maintaining viable practices.
Disclaimer
This guide provides information for educational and planning purposes based on legislation and regulations current as of August 2025. Healthcare laws, regulations, and reimbursement rates change frequently. Readers must verify all information with appropriate regulatory bodies, legal counsel, and professional advisors before implementing any strategies or making practice decisions.
The author and publisher make no warranties regarding the completeness, accuracy, or applicability of this information to individual practice circumstances. Reliance on this guide does not create any professional relationship or guarantee any particular outcome. Each practice must evaluate its unique circumstances and seek appropriate professional consultation when making compliance, financial, or strategic decisions.
References to specific legislation, regulatory bodies, or reimbursement rates are based on publicly available information and may not reflect subsequent changes or amendments. Therapists must maintain current knowledge of applicable laws and regulations through direct monitoring of official sources and professional association updates. This guide does not constitute legal, financial, or professional advice and should not be used as a substitute for consultation with qualified advisors.

















0 Comments