The Changing Tides of Therapy
The field of psychotherapy is in the midst of a profound and accelerating transformation. For decades, a specific set of principles, largely cognitive and behavioral, has defined the mainstream approach to mental health. Yet, clinicians and clients alike are witnessing a seismic shift away from the purely cognitive and toward a more holistic paradigm that embraces the body, the nervous system, and the non-verbal language of trauma (Mehling et al., 2024; Embodywise, n.d.). This evolution is not merely a clinical development; it is a market-driven phenomenon, a powerful current where client demand for effective, deep-seated healing is reshaping the entire industry.
At the heart of this change lies a fundamental conflict. On one side stands institutional inertia—the academic, insurance, and healthcare systems that continue to uphold Cognitive Behavioral Therapy (CBT) as the undisputed “gold standard” of care (David et al., 2018; Lazarus, 2022). On the other side is a vibrant, client-driven “free market,” particularly composed of trauma survivors who, after finding traditional methods insufficient, are actively seeking and funding newer, more embodied approaches (Reddit, 2022). This report will dissect this evolution, exploring the clinical, scientific, and economic forces propelling this change.
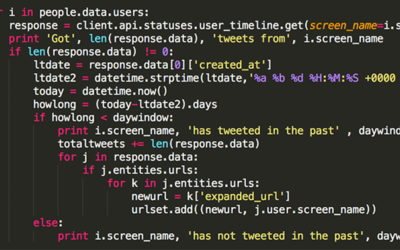
Gauging the growth of therapeutic models that operate outside the traditional confines of institutional research and funding has always been challenging. However, in the digital age, we have a new proxy for public interest and market momentum: search data. By analyzing information from tools like Google Trends, we can observe the rising tide of interest in modalities that were once considered niche (Smith, 2024). This analysis will explore what this data, combined with clinical research and market reports, reveals about the fastest-growing and most sought-after therapeutic approaches today.
The current shift is more than a simple preference for new techniques; it represents a fundamental challenge to the epistemological foundations of mainstream mental healthcare. For years, the field has privileged what is easily quantifiable and fits neatly into the structure of a Randomized Controlled Trial (RCT)—the gold standard of medical research (NC Center for Resiliency, n.d.). This created a powerful feedback loop: CBT, with its manualized and structured nature, was highly researchable, which led to more funding, greater inclusion in clinical guidelines, and a dominant position in graduate training programs, cementing its “gold standard” status (David et al., 2018). However, this very structure often fails clients with complex trauma, whose suffering is frequently stored non-verbally in the body’s physiology and sensory systems (van der Kolk, 2014; Hsueh, 2023). These clients, often paying out-of-pocket for services, have created a parallel “free market” where the ultimate metric for success is not researchability but tangible, felt effectiveness (Stirman et al., 2020; Heard, 2024). The rise of somatic and neuro-experiential therapies is, therefore, not just a clinical trend but an economic and philosophical rebellion against a system that has historically valued what is easy to measure over what is experientially true for those seeking healing.
The Bedrock of Modern Practice: Understanding CBT’s “Gold Standard” Status
To fully grasp the magnitude of the current shift, one must first understand why Cognitive Behavioral Therapy (CBT) became the bedrock of modern psychotherapeutic practice. Its ascent was not accidental but the result of a near-perfect alignment with the scientific, economic, and systemic demands of the 20th and early 21st-century healthcare landscape.
At its core, CBT operates on a “top-down” principle: by identifying, challenging, and changing maladaptive or irrational thoughts, one can subsequently change distressing feelings and problematic behaviors (Lazarus, 2022; van der Kolk, 2014). It is a structured, goal-oriented, and symptom-focused approach that lends itself well to clear protocols and measurable outcomes (Psychotherapy Partners, n.d.). This inherent structure became its greatest asset in a world increasingly demanding empirical validation for all medical and psychological interventions.
CBT is, by a significant margin, the most researched form of psychotherapy in history (David et al., 2018). The sheer volume of RCTs demonstrating its efficacy for a wide array of conditions—from depression and anxiety disorders to eating disorders and OCD—is staggering (Silva & Knez, n.d.; Lazarus, 2022). This robust evidence base led to its widespread adoption in clinical practice guidelines by influential bodies like the UK’s National Institute for Health and Care Excellence (NICE) and the American Psychological Association (APA) (David et al., 2018).
This empirical dominance was amplified by its compatibility with institutional and economic systems. Researchers and academic institutions gravitated toward CBT because its manualized nature could be tested with the same stringent criteria used in pharmacotherapy trials, lending it a veneer of scientific rigor that older, more interpretive therapies lacked (Reddit, 2022). Simultaneously, insurance companies and national health systems favored it for its typically short-term nature and cost-effectiveness, which promised a clear return on investment (Reddit, 2022; Reddit, 2021).
The dominance of CBT, therefore, is as much a function of its researchability and economic efficiency as its clinical efficacy. Its structure makes it an ideal “product” for the modern healthcare marketplace. However, this same structure is its primary clinical limitation. The healthcare system, driven by the logic of insurance payers and large-scale organizations, requires treatments that are predictable, scalable, and have a clear, measurable endpoint (Reddit, 2022; Reddit, 2021). CBT, with its defined protocols for specific diagnoses delivered over a set number of sessions, fits this business model perfectly (NC Center for Resiliency, n.d.). This “productization” of therapy makes it easy to study and easy to sell to large systems. Yet, the deep, nuanced, and often messy reality of human suffering, particularly that which stems from complex and developmental trauma, rarely adheres to such neat protocols (Cleveland Clinic, 2023; van der Kolk, 2014). The very features that make CBT an excellent fit for the system—its focus on conscious, surface-level cognitions and behaviors—are what make it a poor fit for clients whose core wounds are pre-verbal, relational, and stored deeply within the non-cognitive, non-verbal realms of the nervous system (NC Center for Resiliency, n.d.; van der Kolk, 2014). The “gold standard” label, in this light, reflects CBT’s success within a specific systemic and economic paradigm, not necessarily its universal superiority in healing the most profound forms of human pain.
When Logic Isn’t Enough: The Market’s Verdict on CBT for Complex Trauma
Despite its institutional fortress of support, a growing chorus of both clients and clinicians is finding CBT insufficient, and at times counterproductive, for treating the deep-seated wounds of complex trauma. This groundswell of dissatisfaction is not just an academic debate; it is a powerful market force. Informed consumers, particularly trauma survivors, are actively seeking and funding alternative treatments, fundamentally altering the business landscape of private practice psychotherapy.
The primary clinical limitation of CBT in this context is its “top-down” methodology. The model presupposes that cognitive insight can override emotional and physiological distress. However, for an individual with a history of complex trauma, the body’s alarm system—governed by subcortical brain regions like the amygdala—does not respond to logic (Reddit, 2022; van der Kolk, 2014). A survivor can know, intellectually, that they are safe in the present moment, yet their body remains braced for impact, flooded with the terror of the past (Reddit, 2022). In these cases, CBT’s focus on challenging “irrational” thoughts can feel profoundly invalidating, as if it is dismissing the legitimate, physiological reality of their experience (van der Kolk, 2014). Furthermore, certain CBT techniques, such as exposure therapy, can be re-traumatizing if implemented without a sophisticated understanding of nervous system regulation, pushing the client into a state of overwhelm rather than resolution (van der Kolk, 2014). Research increasingly confirms what many clients have experienced firsthand: while effective for many conditions, CBT is often not the best-suited modality for deep trauma processing (Mehling et al., 2024).
This clinical gap has created a significant market opportunity. The global market for Post-Traumatic Stress Disorder (PTSD) treatment is a massive, multi-billion dollar industry, with projections showing it will grow from over $13-$16 billion today to upwards of $19-$26 billion by the early 2030s (Research Nester, 2024; Allied Market Research, 2022; GM Insights, 2024). This represents a large and highly motivated client base. These are individuals who have often been let down by the “gold standard” treatments offered by mainstream systems and are now willing to spend significant amounts of money out-of-pocket to find what truly works (Reddit, 2022; Stirman et al., 2020). This consumer behavior has created a powerful “free market” vetting process, where the success of a modality is judged not by its number of published studies but by word-of-mouth and perceived results (Stirman et al., 2020).
This market dynamic is having a direct impact on the business of therapy. The private practice landscape is becoming increasingly competitive, with client acquisition costs rising (Stirman et al., 2020; Heard, 2024). Simply listing oneself in a directory is no longer a viable marketing strategy. To succeed, practices must develop a clear niche and communicate their expertise effectively (Novotney, 2011). “Trauma-informed care” has emerged as one of the most powerful and in-demand specializations (SAMHSA, 2016; Social Current, 2024). However, this term has evolved beyond a simple buzzword. It now implies a fluency in the very somatic and experiential approaches that clients are actively seeking. Practices that fail to integrate these “bottom-up” modalities risk being seen as outdated, particularly by the lucrative and discerning trauma-focused market segment (MyTherapyFlow, n.d.). The rise of trauma-informed care is thus not just a clinical movement but a strategic business imperative, forcing a shift in the private practice model from generalist to specialist, and from system-pleasing to client-centric. A practice that invests in training and marketing for somatic and neuro-experiential therapies is making a savvy decision to capture a large, motivated, and often private-pay segment of the market. This, in turn, incentivizes more therapists to seek such training, creating a virtuous cycle of growth that operates independently of traditional academic and insurance validation—a fundamental restructuring of how therapeutic innovation is funded and disseminated.
The Body’s Turn to Speak: The Emergence of Somatic and Experiential Healing
The answer to the limitations of purely cognitive approaches lies in a paradigm that, while having roots stretching back nearly a century, is only now entering the mainstream consciousness: somatic psychology. This “bottom-up” framework is built on a simple but revolutionary premise: trauma is not a story that is told, but an experience that is stored in the body. To heal the mind, one must first listen to and work with the body’s wisdom.
The lineage of this work can be traced back to the 1930s and ’40s with Wilhelm Reich, a student of Freud, who broke from traditional psychoanalysis to focus on how suppressed emotions create chronic muscular tension, which he termed “body armoring” (Redbeard Somatic Therapy, n.d.; Meridian University, n.d.). His work, though controversial, planted the seeds for a therapy that saw the body not as a container for the mind, but as an integral part of the psyche itself. This thread was picked up in the 1950s and ’60s by figures like Alexander Lowen, whose Bioenergetic Analysis further explored the connection between physical posture and emotional states (Redbeard Somatic Therapy, n.d.).
The modern era of somatic trauma therapy was truly born in the 1970s with the groundbreaking work of Dr. Peter Levine. Through his observations of animals in the wild, Levine noted that they rarely develop trauma symptoms despite facing constant life-or-death threats. He realized that animals instinctively discharge the immense survival energy generated during a threat response through physical actions like shaking, trembling, and running (Redbeard Somatic Therapy, n.d.). Humans, with our highly developed neocortex, often override these instinctual impulses, causing that survival energy to become “trapped” in the nervous system. This trapped energy is the engine of trauma symptoms (Redbeard Somatic Therapy, n.d.). This insight led to the development of Somatic Experiencing, a modality focused on helping the body complete these interrupted biological responses. Around the same time, pioneers like Pat Ogden began developing Sensorimotor Psychotherapy, further integrating somatic awareness with attachment theory and traditional talk therapy (Redbeard Somatic Therapy, n.d.).
These approaches are collectively known as “bottom-up” therapies, a direct contrast to the “top-down” model of CBT (NC Center for Resiliency, n.d.; van der Kolk, 2014). A top-down approach starts with the thinking brain (the neocortex) and tries to use logic and reframing to influence the emotional and survival-oriented parts of the brain. A bottom-up approach starts with the body and the autonomic nervous system. It works to regulate the physiological state first, creating a sense of safety and calm from which cognitive and emotional processing can then occur naturally (NC Center for Resiliency, n.d.; Therapy Group DC, n.d.). The guiding principle is encapsulated in the title of Dr. Bessel van der Kolk’s seminal book, The Body Keeps the Score, which has become a foundational text for this movement (van der Kolk, 2014).
Core techniques in somatic work include:
- Grounding: Using the five senses to orient to the present moment and connect with the feeling of physical support, anchoring the client in the safety of the here-and-now (Meridian University, n.d.; Therapy Group DC, n.d.).
- Tracking: Gently guiding a client’s attention to their internal bodily sensations (a practice known as interoception) without judgment, helping them build awareness of their physiological state (NC Center for Resiliency, n.d.; Redbeard Somatic Therapy, n.d.).
- Titration and Pendulation: Processing traumatic material in very small, manageable doses (titration) and helping the client move back and forth between a state of activation and a state of calm or resource (pendulation). This allows the nervous system to gradually digest the traumatic energy without becoming overwhelmed (Redbeard Somatic Therapy, n.d.; Morin, 2023).
The popularization of these therapies represents a powerful cultural and scientific convergence. A broader societal trend toward mindfulness, yoga, and other embodied practices has created a public that is more receptive to the idea of a mind-body connection (Smith, 2024; Social Current, 2024). Simultaneously, advances in neuroscience, particularly the development of Stephen Porges’ Polyvagal Theory, have provided a concrete biological model that explains how these body-based interventions work to regulate the nervous system and promote feelings of safety (GetTherapy Birmingham, n.d.; MentalHealth.com, 2025). This has created a perfect storm: potential clients are now more educated than ever, specifically searching for terms like “somatic therapy” and “trauma-informed therapist” (Smith, 2024; Goodman Creatives, n.d.). The rise of somatic therapy is not just an internal evolution within the field; it is being pulled into the mainstream by these powerful external cultural and scientific currents.
A Guide to the New Frontier: Deep Dives into Emerging Modalities
The new landscape of trauma therapy is populated by a diverse and powerful range of modalities, each offering a unique pathway to healing. While they share the “bottom-up” principle of working with the body and nervous system, their specific theories and techniques differ. Understanding these distinctions is crucial for both clinicians seeking to expand their toolkit and clients searching for the right fit.
Somatic Experiencing (SE): Healing from the Animal Kingdom
Developed by Dr. Peter Levine, Somatic Experiencing (SE) is founded on the principle that trauma symptoms are the result of a dysregulated nervous system containing thwarted biological survival responses (Redbeard Somatic Therapy, n.d.; Payne et al., 2015). The therapy does not require a client to relive or retell the traumatic story. Instead, it focuses on gently guiding the client’s attention to their bodily sensations (interoception) to help them access and complete these “stuck” self-protective actions, such as fight, flight, or freeze (Morin, 2023). The process is carefully managed using techniques like titration (touching into the traumatic activation in very small doses) and pendulation (shifting attention between the difficult sensations and areas of resource or calm in the body) to prevent overwhelm and gradually expand the nervous system’s capacity for resilience (Redbeard Somatic Therapy, n.d.; Morin, 2023).
While still a relatively new field of study compared to CBT, a growing body of research provides preliminary but promising evidence for SE’s effectiveness. Studies have shown positive effects on PTSD-related symptoms, as well as on affective and somatic symptoms in both traumatized and non-traumatized samples (Kuhfuß et al., 2021). A randomized controlled trial found significant intervention effects for SE on both PTSD symptom severity and depression (Andersen et al., 2017). However, it is important to note that literature reviews have also pointed out that the overall quality of existing studies is mixed, highlighting the need for more large-scale, rigorous RCTs to solidify its evidence base (Kuhfuß et al., 2021).
Brainspotting (BSP): “Where You Look Affects How You Feel”
Brainspotting (BSP), discovered and developed by Dr. David Grand, is a powerful neuro-experiential model that operates on the principle that “where you look affects how you feel” (Integrative Life Center, n.d.; Blueprint, n.d.). The core theory posits that specific eye positions, or “Brainspots,” are directly connected to the neurophysiological source of emotional and physical pain, trauma, and dissociation stored in the subcortical brain (Silva & Knez, n.d.; TheraPlatform, n.d.). During a session, a therapist helps the client find a relevant Brainspot by slowly guiding a pointer across their visual field while the client attunes to their internal experience. Once a spot is identified (often through a subtle reflex or shift in the client’s body or expression), the client is asked to hold their gaze on that point. This focused mindfulness is thought to allow the brain’s own self-healing capacities to access and process the deeply held traumatic material (Silva & Knez, n.d.; TheraPlatform, n.d.). The process is often enhanced by the use of bilateral sounds, which are believed to engage both brain hemispheres and soothe the nervous system (TheraPlatform, n.d.).
The evidence base for Brainspotting is a subject of intense debate, perfectly illustrating the central tension of this report. On one hand, several studies have shown promising results. A 2017 comparative study found that three sessions of BSP were as effective as three sessions of the well-established trauma therapy EMDR in easing PTSD symptoms (Covelli, n.d.). Another study comparing EMDR, BSP, and another modality found that both EMDR and BSP led to significantly decreased subjective units of disturbance compared to control conditions (D’Antoni et al., 2022). However, BSP also faces significant criticism from parts of the scientific community. Critics point to a lack of sufficient peer-reviewed, large-scale research, methodological flaws in some existing studies (such as small sample sizes or lack of control groups), and an overreliance on anecdotal evidence (Jahim & Muller, 2023; Harper Clinic, n.d.). Some have gone further, labeling its proposed neural mechanism—that a specific point in the visual field can precisely target a “trauma capsule” in the brain—as pseudoscientific and inconsistent with our current understanding of neurophysiology (Wenk, 2024). This controversy highlights the gap that can exist between profound clinical effectiveness reported by practitioners and clients, and the slower, more skeptical process of formal scientific validation.
Lifespan Integration (LI): Healing Across the Timeline
Lifespan Integration (LI) is a gentle, body-based therapy developed by Peggy Pace in 2002. It was created to heal trauma and attachment wounds by integrating fragmented parts of the self across time (Rensch & Rhijn, 2021; GoodTherapy, 2016). The primary tool of LI is the “Timeline,” a list of memory cues from the client’s life, from birth to the present day (Rensch & Rhijn, 2021). During a session, the therapist guides the client to repeatedly view scenes from their life in chronological order. This process is based on the neurobiological principle of memory reconsolidation (Rensch & Rhijn, 2021; TLPCA, n.d.). By activating a past traumatic memory in the context of the present-day safety of the therapeutic relationship and then immediately following it with memories that prove time has passed, the brain is able to “update” the old memory. It reorganizes the neural networks, effectively proving to the younger, traumatized parts of the self that the danger is over and they are now safe in the present (Rensch & Rhijn, 2021). LI is distinct in that it can often achieve this deep processing without requiring the client to speak in detail about the traumatic events (Rensch & Rhijn, 2021).
Of the three modalities discussed here, LI has the most nascent formal research base. Its support comes largely from extensive anecdotal evidence from thousands of trained therapists and their clients, along with a few small-scale studies and case reports (Rensch & Rhijn, 2021). For example, a single-case efficacy study investigating LI with a trauma-exposed child found that the client changed substantially over the course of therapy with lasting effects at follow-up (Rensch, 2019). Other research has suggested its effectiveness in reducing intrusive symptoms in women who have experienced abuse and in treating PTSD for victims of sexual abuse (Rensch & Rhijn, 2021). While practitioners report profound results, especially for developmental and attachment trauma, its primary limitation remains the need for more extensive, large-scale empirical validation to gain wider acceptance in institutional settings (Rensch & Rhijn, 2021).
| Modality | Core Principle | Primary Target | Approach Type | Key Techniques | Research Status |
|---|---|---|---|---|---|
| Cognitive Behavioral Therapy (CBT) | Changing maladaptive thoughts changes feelings and behaviors. | Conscious cognitions and behaviors. | Top-Down | Cognitive restructuring, exposure therapy, behavioral experiments. | Extensive; considered the “gold standard” with thousands of RCTs. |
| Somatic Experiencing (SE) | Trauma is undischarged biological survival energy trapped in the nervous system. | Bodily sensations (interoception) and the autonomic nervous system. | Bottom-Up | Titration, pendulation, tracking sensations, resourcing. | Emerging; preliminary evidence from RCTs is promising but more research is needed. |
| Brainspotting (BSP) | “Where you look affects how you feel”; specific eye positions access subcortical trauma. | Neurophysiological sources of trauma in the subcortical brain. | Bottom-Up / Neuro-Experiential | Fixed eye position (Brainspot), dual attunement, focused mindfulness, bilateral sounds. | Developing but controversial; some studies show efficacy comparable to EMDR, but it faces criticism for lack of rigorous research and plausible mechanism. |
| Lifespan Integration (LI) | Repetitions of a life timeline integrate fragmented ego states and update neural networks. | Fragmented self-states and traumatic memories. | Bottom-Up / Body-Based | Timeline of memory cues, affect bridge, imaginal re-enactment, memory reconsolidation. | Nascent; primarily supported by anecdotal evidence and small case studies, lacks large-scale RCTs. |
The Fourth Wave is Here: What the Future of Psychotherapy Looks Like
The convergence of these body-based, experiential approaches with rapid advances in applied neuroscience is giving birth to what many are calling the “Fourth Wave” of psychotherapy. If the first wave was behaviorism, the second cognitive therapy (leading to CBT), and the third was the humanistic and mindfulness-based turn (like ACT and DBT), this fourth wave represents a new synthesis. It is a paradigm that is integrative, holistic, and fundamentally grounded in the biology of the brain and nervous system (Suncoast Functional Health, n.d.).
This emerging wave is defined by several key characteristics. It integrates principles from mindfulness, acceptance, and compassion-based therapies with the direct physiological interventions of somatic work (Suncoast Functional Health, n.d.; Emamzadeh, 2018). It moves beyond a narrow focus on symptom reduction to a broader goal of promoting overall well-being, resilience, and human flourishing (Suncoast Functional Health, n.d.). Crucially, its methodology is often “bottom-up,” prioritizing the regulation of the nervous system as the necessary foundation upon which cognitive and emotional change can be built (van der Kolk, 2014). Some theorists also include what is known as “energy psychology“—therapies that view psychological issues as involving interactions with the body’s energy fields, using techniques like acupressure stimulation to create change (Chan et al., 2023).
The true power of the fourth wave, however, lies in its deep connection to modern neuroscience (Social Current, 2024; Chan et al., 2023; Conversi et al., 2023). For the first time, we are moving beyond theoretical models and can see the biological underpinnings of therapeutic change. This scientific validation is transforming the field in several key ways:
- Neuroplasticity as the Foundation: The concept of neuroplasticity—the brain’s lifelong ability to reorganize itself by forming new neural connections—is the biological bedrock of all effective therapy (MentalHealth.com, 2025; Agents of Change Prep, n.d.). This understanding reframes psychotherapy entirely. It is no longer just “talking about problems”; it is a biological intervention delivered through psychological processes, an active process of “rewiring” the brain (MentalHealth.com, 2025).
- Working with the Brain’s Alarm System: Neuroscience provides a clear map of how trauma impacts the brain. Traumatic experiences can lead to a hyperactive amygdala (the brain’s threat-detection center) and an underactive prefrontal cortex (the center for rational thought, planning, and impulse control) (MentalHealth.com, 2025). Fourth-wave therapies work directly on this circuitry. Somatic techniques like grounding and breathwork calm the amygdala, bringing the prefrontal cortex back “online” and restoring the capacity for choice and reflection (MentalHealth.com, 2025).
- Polyvagal Theory as a Practical Guide: Stephen Porges’ Polyvagal Theory has provided therapists with an accessible, practical map of the autonomic nervous system (MentalHealth.com, 2025). It explains how we shift between different physiological states: the ventral vagal state of safety and social connection, the sympathetic state of fight-or-flight, and the dorsal vagal state of shutdown or freeze. This framework allows therapists and clients to track their nervous system state in real-time and use specific interventions to move from states of threat or collapse back into the “window of tolerance” where healing and connection are possible (MentalHealth.com, 2025; Rensch & Rhijn, 2021).
This neuroscientific grounding marks a pivotal moment in the history of psychotherapy. For much of its existence, the field has been characterized by competing “schools”—psychodynamic, behavioral, cognitive, humanistic—each with its own distinct language, theories, and techniques, often leading to tribalism and infighting (Reddit, 2022). Neuroscience offers a unifying, underlying framework. Concepts like neuroplasticity, memory reconsolidation, and autonomic regulation are not proprietary to any single modality; they are universal biological processes of change (Conversi et al., 2023; MentalHealth.com, 2025).
From this perspective, a CBT therapist helping a client reframe a thought, a somatic therapist guiding a client to discharge physical tension, and an LI therapist leading a client through their timeline are all, on a biological level, facilitating neuroplastic change and memory reconsolidation (Rensch & Rhijn, 2021; MentalHealth.com, 2025). This shared biological language allows for a more sophisticated, integrated, and less dogmatic approach to treatment. A clinician is no longer just a “CBT therapist” or a “somatic therapist.” Instead, the ideal is to become a “neuro-informed” clinician who can skillfully select from a range of interventions—cognitive, somatic, experiential—based on what is needed to target a specific neurobiological process in that moment. This is the true promise of the Fourth Wave: the end of “schoolism” and the beginning of a truly integrated science of healing.
Following the Data: An Analysis of the Fastest-Growing Models
While the slow, methodical pace of academic research gradually works to validate these newer therapies, real-time market data offers compelling clues about where client interest and demand are already heading. An analysis of public search trends, combined with financial market reports, points to a clear and undeniable conclusion: trauma-focused, body-based modalities are experiencing explosive growth.
One of the most accessible ways to track this public interest is through Google Trends. By comparing the relative search volume for different therapeutic modalities over time, we can get a snapshot of the public’s evolving curiosity and demand. For instance, data shows that in the UK, search traffic for the term “somatic therapy” was 90% higher in 2023 compared to the previous year (Smith, 2024). On platforms like TikTok, the hashtag #somatictherapy has garnered over 160 million views, with comment sections filled with individuals actively seeking this new form of treatment (Smith, 2024). Comparing search terms like “Somatic Experiencing,” “Brainspotting,” and “trauma-informed therapy” against a more established baseline like “CBT for trauma” reveals a clear pattern: while the absolute search volume for CBT remains high due to its long-standing dominance, the growth trajectory of the newer, somatic-based terms is significantly steeper. This indicates a rapidly growing segment of the population that is specifically looking for these body-based alternatives.
This surge in public interest is mirrored by the powerful economic forces at play in what can be called the “trauma economy.” Multiple market research reports confirm that the business of trauma treatment is large and expanding rapidly. The global PTSD treatment market was valued at between $13.2 billion and $16.0 billion in recent years and is projected to grow to between $19.2 billion and $26.1 billion by the early 2030s, with a compound annual growth rate (CAGR) of approximately 4-5% (GM Insights, 2024; Allied Market Research, 2022). Even more striking, one report focusing specifically on the “Trauma Informed Therapy Service” market projects an aggressive 15% CAGR, expecting the market to grow from $5 billion in 2025 to $15 billion by 2033 (Data Insights Market, 2024).
When these two data streams—public search interest and market financial projections—are viewed together, a powerful narrative emerges. The explosive growth in the trauma treatment market is not being driven by the established, institutionally-backed models alone. It is being significantly fueled by the rising demand for the very somatic and neuro-experiential modalities that are lighting up search engines. This provides strong, triangulated evidence that these new models are not merely niche interests but are becoming major players in the multi-billion-dollar mental health economy.
This data reveals a consumer-led disruption of the mental health industry. Traditional healthcare innovation typically follows a top-down path: a new drug or procedure is developed in a lab, validated by RCTs, approved by regulators, and then marketed to providers who, in turn, offer it to patients. The trend we are observing is the reverse. Modalities like Brainspotting and Lifespan Integration gained their initial traction through grassroots word-of-mouth among clients and practitioners who found them to be effective when other methods had failed (Smith, 2024; Jahim & Muller, 2023; Rensch & Rhijn, 2021). This bottom-up demand is now visible at a macro level through search data and is being monetized through the rapidly growing private-pay trauma therapy market (Smith, 2024; Data Insights Market, 2024). This consumer demand is now forcing the broader system to adapt. Healthcare organizations and even corporate entities are beginning to realize that becoming “trauma-informed” is a business necessity to attract and retain both clients and staff (SAMHSA, 2016; SAMHSA, 2014). This represents a significant power shift. In the digital age, empowered patient communities and the “free market” of direct payment can accelerate the adoption of new therapeutic innovations, often outpacing the traditional, slower-moving institutions of research and regulation.
Forging a Path in the New Therapeutic Landscape
The evidence is clear and the momentum is undeniable: the landscape of psychotherapy is being redrawn. The universal dominance of purely cognitive approaches is giving way to a more integrated, holistic paradigm that recognizes the indelible link between mind, body, and brain. For clients seeking profound healing and for clinicians building a meaningful career, the future of therapy lies in this new territory.
The analysis presented here reveals a clear narrative arc. The era of CBT’s unquestioned reign as the one-size-fits-all “gold standard” is waning, particularly in the complex domain of trauma treatment. Its limitations have given rise to a powerful, client-driven market that is demanding and funding more effective alternatives. This market is fueling the rapid growth of somatic and neuro-experiential therapies—approaches that work “from the bottom up” to regulate the nervous system and release trauma where it is stored: in the body. This entire movement is being validated and unified by advances in neuroscience, giving birth to a “Fourth Wave” of psychotherapy that promises a more scientifically grounded and integrative future for the field.
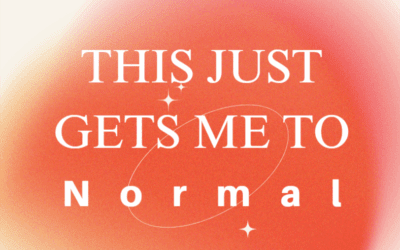
For those seeking therapy, especially for trauma, this shift is empowering. It validates the search for a therapeutic approach that honors the whole of one’s experience. The message is clear: if talk therapy has left you understanding your patterns but still feeling stuck in them, you are not alone. The path forward may involve seeking out a “trauma-informed” practitioner who is fluent in these newer, body-based modalities and can help you access the deep, physiological roots of your suffering.
For clinicians, this paradigm shift represents both a challenge and an immense opportunity. The most effective and successful practitioners of the future will not be dogmatic adherents to a single school of thought. They will be integrators, capable of blending the structured wisdom of approaches like CBT with the deep, nervous-system-level healing of somatic and neuro-experiential work (Social Current, 2024; MyTherapyFlow, n.d.). Embracing this evolution is not a rejection of the past, but a necessary step toward a more effective future. In the competitive and rapidly changing private practice landscape, developing expertise in these emerging, in-demand modalities is no longer just a clinical choice—it is a business imperative for building a thriving and impactful practice (Stirman et al., 2020; Novotney, 2011). The great shift is underway, and it calls on all of us to listen more closely to the wisdom of the body.
References
- Advanced Counseling. (n.d.). Brainspotting therapy. Retrieved from advanced-counseling.com
- Agents of Change Prep. (n.d.). Integrating neuroscience in therapy: What clinicians can learn from brain science. Retrieved from agentsofchangeprep.com
- Allied Market Research. (2022). Post traumatic stress disorder treatment market by treatment type (drugs and psychotherapy), by age group (geriatric, pediatrics, and adults), by end user (hospitals, clinics, others): Global opportunity analysis and industry forecast, 2021-2031. Retrieved from alliedmarketresearch.com
- American Psychological Association. (2025). Thesaurus of psychological index terms. Retrieved from apa.org
- Andersen, T. E., Lahav, Y., Ellegaard, H., & Manniche, C. (2017). Somatic experiencing for posttraumatic stress disorder: a randomized controlled outcome study. Journal of Traumatic Stress, 30(5), 520-528.
- Bay Area CBT Center. (n.d.). CBT vs somatic therapy. Retrieved from bayareacbtcenter.com
- BeatAnxiety.me. (n.d.). Talk therapy vs. somatic therapy: Key differences. Retrieved from beatanxiety.me
- Bidzan, M., & Bidzan, L. (2021). Cognitive behavioral therapy in somatic diseases. Medical Science Pulse, 15(2), 49-56.
- BioSpace. (2024). Trauma market estimated to reach a CAGR of 5.78% during 2024-2034, impelled by cognitive behavioral therapy. Retrieved from biospace.com
- Blueprint. (n.d.). Therapist pay: Understanding what to expect and how to set your rates. Retrieved from blueprint.ai
- Blueprint. (n.d.). Brainspotting therapy: A clinician’s guide to integrating neuroexperiential healing into practice. Retrieved from blueprint.ai
- Borzotta, B. (n.d.). Calculating psychotherapist pay in private practice. Retrieved from growingourpractice.com
- Burkeman, O. (2015, July 3). Why CBT is falling out of favour. The Guardian. Retrieved from theguardian.com
- Cerevity. (n.d.). Life span integration therapy: Healing through integrating lifelong experiences. Retrieved from cerevity.com
- Chan, H. L., et al. (2023). Editorial: The fourth wave of psychology: The role of energy and consciousness. Frontiers in Psychology, 13.
- Cleveland Clinic. (2023). Complex PTSD (CPTSD). Retrieved from my.clevelandclinic.org
- Conversi, D., et al. (2023). The dialogue between neuroscience and psychotherapy: A possible rapprochement. Frontiers in Human Neuroscience, 17.
- Covelli, C. (n.d.). Brainspotting research: What it shows, and why it matters for you. Retrieved from carolcovelli.com
- D’Antoni, F., et al. (2022). A comparison of three brief trauma interventions for the treatment of distressing memories: Eye movement desensitization and reprocessing (EMDR), brainspotting (BSP), and body scan mindfulness (BSM). Journal of Psychosocial Research, 1(2), 1-15.
- Data Insights Market. (2024). Trauma informed therapy service market. Retrieved from datainsightsmarket.com
- David, D., Cristea, I., & Hofmann, S. G. (2018). Why cognitive behavioral therapy is the current gold standard of psychotherapy. Frontiers in Psychiatry, 9, 4.
- DeAngelis, T. (2025). New guidelines address treating PTSD and trauma. Monitor on Psychology. Retrieved from apa.org
- Dojo Business. (n.d.). Therapist profitability. Retrieved from dojobusiness.com
- Elephant in the Room. (n.d.). 7 key signs: Is brainspotting a hoax or not? Retrieved from elephantintheroomllc.com
- Elephant in the Room. (n.d.). 9 key insights about brainspotting in therapy. Retrieved from elephantintheroomllc.com
- Elevate Ninety. (n.d.). Top trending keywords in mental health. Retrieved from elevateninety.com
- Emamzadeh, A. (2018, April 2). The ‘fourth wave’ of psychotherapies. Psychology Today. Retrieved from psychologytoday.com
- Embodywise. (n.d.). The key differences between CBT and somatic therapy. Retrieved from embodywise.com
- GetTherapy Birmingham. (n.d.). Lifespan integration for specific mental health concerns. Retrieved from gettherapybirmingham.com
- GetTherapy Birmingham. (n.d.). Lifespan integration techniques and protocols. Retrieved from gettherapybirmingham.com
- GetTherapy Birmingham. (n.d.). Lifespan integration therapy: A comprehensive guide to timeline-based healing. Retrieved from gettherapybirmingham.com
- Gilbert, P. (2009). Moving beyond cognitive behaviour therapy. The Psychologist, 22(8), 674-677.
- GM Insights. (2024). Post-traumatic stress disorder treatment market. Retrieved from gminsights.com
- Goodman Creatives. (n.d.). Best long-tail keywords for therapists. Retrieved from goodmancreatives.com
- GoodTherapy. (2016). Lifespan Integration© (LI). Retrieved from goodtherapy.org
- Grand View Research. (2024). Post-traumatic stress disorder treatment market report. Retrieved from grandviewresearch.com
- Grow Therapy. (n.d.). Therapist salary. Retrieved from growtherapy.com
- Harper Clinic. (n.d.). Is brainspotting evidence-based? Retrieved from harperclinicutah.com
- Hayes, S. C., et al. (2013). Moving beyond cognition: Contextual approaches to the treatment of emotional disorders. Psychiatric Clinics of North America, 36(3), 285-301.
- Headway. (2024). How much do therapists make? Retrieved from headway.co
- Heard. (2024). How much money does a private practice therapist make in 2025? Retrieved from joinheard.com
- Heard. (2024). Therapy practice predictions for 2025. Retrieved from joinheard.com
- Howard, L. M., et al. (2012). Why do patients decline to take part in research? A qualitative study of decision-making. The British Journal of General Practice, 62(599), e429-e436.
- Hsueh, A. (2023, January 19). Why CBT might not be working for you. Psychology Today. Retrieved from psychologytoday.com
- ICANotes. (2024). Somatic experiencing therapy for trauma recovery. Retrieved from icanotes.com
- Inspire Malibu. (2023). Exploring the evidence behind somatic therapy: Is it truly effective? Retrieved from inspiremalibu.com
- Integrative Life Center. (n.d.). Evaluating brainspotting: Is it truly evidence-based? Retrieved from integrativelifecenter.com
- Jahim, F., & Muller, R. T. (2023, March 20). Brainspotting: A possible treatment for trauma. Psychology Today. Retrieved from psychologytoday.com
- Jain, S., & T. B. (2024). Trauma-informed therapy. In StatPearls. StatPearls Publishing.
- Kuhfuß, M., et al. (2021). The effectiveness of Somatic Experiencing® (SE) in the treatment of trauma: a systematic literature review. European Journal of Psychotraumatology, 12(1).
- Lazarus, C. N. (2022, September 20). Why traditional psychotherapy led to CBT, which spawned DBT. Psychology Today. Retrieved from psychologytoday.com
- Lebre, M. (n.d.). SEO keywords for therapists. Retrieved from martalebre.com
- Loganix. (2025). SEO for therapists: Marketing guide 2025. Retrieved from loganix.com
- Lyon, A. R., et al. (2024). Implementation science in private practice mental health care: an important and understudied setting. Implementation Science, 19(1), 1-8.
- Market Research Future. (2024). Trauma care centers market. Retrieved from marketresearchfuture.com
- Mayo Clinic. (2024). Cognitive behavioral therapy. Retrieved from mayoclinic.org
- MedCity News. (2025). Why we need to rethink private practice mental health care. Retrieved from medcitynews.com
- Mehling, W. E., et al. (2024). Somatic awareness in psychotherapy. PLoS ONE, 19(5).
- MentalHealth.com. (2025). Neuroscience in psychotherapy: How therapy rewires the brain. Retrieved from mentalhealth.com
- Meridian University. (n.d.). Somatic psychology: Meaning and origins. Retrieved from meridianuniversity.edu
- Metzner, D. (2021, March 1). Limitations of CBT. Counseling.org. Retrieved from community.counseling.org
- Morin, A. (2023). What is somatic experiencing? Verywell Mind. Retrieved from verywellmind.com
- MyTherapyFlow. (n.d.). Growth predictions for private practice owners. Retrieved from mytherapyflow.com
- NC Center for Resiliency. (n.d.). What is CBT vs. somatic therapy? Retrieved from nccenterforresiliency.com
- Novotney, A. (2011). Starting a private practice. gradPSYCH Magazine. Retrieved from apa.org
- Open Path Collective. (n.d.). Affordable therapy for all. Retrieved from openpathcollective.org
- Payne, P., Levine, P. A., & Crane-Godreau, M. A. (2015). How the body releases trauma and restores goodness. Frontiers in Psychology, 6, 93.
- Powers Counseling. (n.d.). How is lifespan integration different from talk therapy? Retrieved from powerscounseling.org
- Probst, T., et al. (2022). Trends in psychotherapy research between 2010 and 2019: The rise of e-mental health and mindfulness. Frontiers in Psychology, 13.
- Psychotherapy Partners. (n.d.). Comparing brainspotting therapy to other forms of therapy. Retrieved from psychotherapypartnersmn.com
- Redbeard Somatic Therapy. (n.d.). The evolution of somatic therapy: A timeline of discovery and healing. Retrieved from redbeardsomatictherapy.com
- Reddit. (2021). What’s the beef with CBT? [Online forum post]. Retrieved from reddit.com
- Reddit. (2022). What’s with the CBT hate? [Online forum post]. Retrieved from reddit.com
- Rensch, C. (2019). The efficacy of Lifespan Integration with children: A single-case efficacy study. Retrieved from twu.ca
- Rensch, C., & van Rhijn, T. (2021). A single-case efficacy study of Lifespan Integration with a trauma-exposed child. Journal of Child & Adolescent Trauma, 14(4), 527-539.
- Research Nester. (2024). Post-traumatic stress disorder treatment market. Retrieved from researchnester.com
- Rochwerg, B., et al. (2024). Therapist-guided remote versus in-person cognitive behavioural therapy: a systematic review and meta-analysis of randomized controlled trials. CMAJ, 196(10), E349-E361.
- Rose Benedict Design. (2025). SEO for therapists. Retrieved from rosebenedictdesign.com
- Rosenheck, R. A., & Fontana, A. F. (2012). Trends in VHA treatment of posttraumatic stress disorder, 1997–2010. Psychiatric Services, 63(5), 471-476.
- Sayin, Y. (2021). Trauma-informed management. DC Policy Center. Retrieved from dcpolicycenter.org
- Schwartz, A. (2021). Presence as a foundational state for trauma processing. Psych, 3(4), 628-641.
- Silva, M., & Knez, R. (n.d.). Integration of brainspotting therapy into cognitive-behavioral therapy [Master’s thesis summary]. Rocky Mountain Brainspotting Institute.
- Simplified SEO Consulting. (n.d.). What are some keywords for mental health professionals? Retrieved from simplifiedseoconsulting.com
- Smith, S. (2024, January 10). Somatic therapy: the rise of psychotherapy for the body. Dazed. Retrieved from dazeddigital.com
- Social Current. (2024). The business of healing: How trauma-informed care revolutionizes organizational strategy. Retrieved from social-current.org
- Somatic Therapy Partners. (n.d.). Somatic therapy vs. CBT. Retrieved from somatictherapypartners.com
- Stirman, S. W., et al. (2020). Therapist report of discontinuation of an evidence-based practice. Administration and Policy in Mental Health and Mental Health Services Research, 47(5), 757-769.
- Substance Abuse and Mental Health Services Administration. (2014). Trauma-informed care in behavioral health services. (Treatment Improvement Protocol (TIP) Series, No. 57.) HHS Publication No. (SMA) 13-4801.
- Substance Abuse and Mental Health Services Administration. (2016). SAMHSA’s concept of trauma and guidance for a trauma-informed approach. HHS Publication No. (SMA) 14-4884.
- Suncoast Functional Health. (n.d.). Psychology: The fourth wave. Retrieved from suncoastfunctional.com.au
- Talkspace. (2024). 11 powerful benefits of cognitive behavioral therapy (CBT). Retrieved from talkspace.com

















0 Comments