How Therapists Can Prepare For Insurance in 2025
As we move into 2025, Alabama’s mental health landscape stands at a critical juncture. With Blue Cross Blue Shield of Alabama (BCBSAL) proposing innovative healthcare models, ongoing antitrust settlements, and evolving parity requirements, therapists across our state must stay informed and prepared. This comprehensive guide will help you understand these changes and their potential impact on your practice.
The ALLHealth Initiative: A New Chapter in Alabama Healthcare
At the forefront of change is BCBSAL’s ALLHealth initiative—a groundbreaking public-private partnership that represents Alabama’s unique approach to addressing the coverage gap. Unlike traditional Medicaid expansion adopted by many states, ALLHealth proposes to use federal Medicaid expansion dollars to fund private insurance coverage through BCBSAL.
This initiative aims to cover individuals earning up to 138% of the Federal Poverty Level, potentially bringing insurance to 113,000 uninsured Alabamians initially, with projections suggesting this number could rise to 260,000-330,000 with additional premium assistance. For mental health providers, this represents a significant expansion of the potential client base, though it comes with important considerations.
The program’s structure reflects Alabama’s political landscape, where traditional Medicaid expansion has faced resistance. By channeling federal funds through private insurance rather than expanding government programs directly, ALLHealth offers a more politically palatable solution to our state’s coverage gap. County commissions across Alabama, including Albany County, are being actively courted for support, signaling the serious momentum behind this initiative.
Understanding the Provider Landscape Post-Antitrust Settlement
The recent $2.8 billion antitrust settlement against BCBSAL marks a watershed moment for healthcare providers in Alabama. This settlement, addressing allegations of anticompetitive practices, includes provisions for increased transparency and accountability that could fundamentally alter the relationship between insurers and providers.
For therapists, the settlement’s most immediate impact lies in the claims process. Providers have until July 29, 2025, to submit claims for damages related to alleged anticompetitive practices. This represents a unique opportunity to address past grievances and potentially recover lost revenue. The settlement also mandates new transparency measures that should provide unprecedented insight into BCBSAL’s pricing structures and denial rates.
Currently, BCBSAL reimburses approximately $136 for a 90837 session (60-minute psychotherapy), which is comparable to other carriers. However, the minimal rate increase of just 8 cents at the start of 2022 highlights the ongoing challenges therapists face with reimbursement stagnation. The transparency requirements emerging from the antitrust settlement may provide leverage for future rate negotiations.
Mental Health Parity: Federal Pressure Meets State Reality
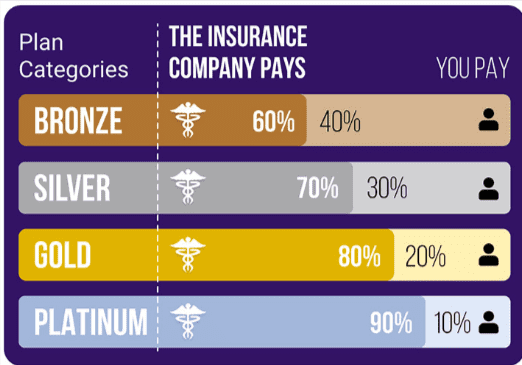
Perhaps no issue is more critical to mental health providers than the ongoing struggle for true parity between mental health and physical health coverage. Alabama’s benchmark BCBS plan currently includes quantitative limits on mental health and substance use services—restrictions that potentially violate federal parity laws.
The Mental Health Parity and Addiction Equity Act (MHPAEA) requires insurers to provide mental health benefits on par with medical benefits. Yet in practice, Alabama therapists continue to face higher copays for clients, increased denial rates, and narrower networks compared to medical providers. These disparities not only affect provider revenues but also create barriers to care for vulnerable populations.
Federal enforcement of parity requirements is intensifying, and Alabama’s benchmark plans are increasingly under scrutiny. This pressure could lead to significant changes in how mental health services are covered and reimbursed. Therapists should prepare for potential shifts in benefit structures, prior authorization requirements, and network adequacy standards.
Preparing Your Practice for 2025 and Beyond
As these policy changes unfold, Alabama therapists must take proactive steps to position their practices for success. Here are essential strategies for navigating this evolving landscape:
1. Network Participation and Credentialing
With ALLHealth potentially introducing new plan types, staying current with credentialing requirements is crucial. Review your current BCBSAL contracts and ensure all credentialing information is up to date. Consider whether expanding your network participation makes sense as new plans emerge. The influx of newly insured individuals through ALLHealth could significantly increase demand for mental health services, making network participation more valuable than ever.
2. Documentation and Compliance
The increased scrutiny on mental health parity means documentation standards will likely become more stringent. Ensure your clinical documentation clearly demonstrates medical necessity and aligns with parity requirements. Invest in training for your staff on proper coding and documentation practices to minimize denials and maximize reimbursement.
3. Financial Planning and Diversification
While the expansion of coverage through ALLHealth presents opportunities, relying too heavily on any single payer remains risky. BCBSAL’s 86% market share in Alabama creates a concerning level of dependence for many practices. Consider diversifying your revenue streams through:
- Developing cash-pay services for specialized treatments
- Exploring telehealth opportunities that may expand your geographic reach
- Building relationships with employer-sponsored wellness programs
- Considering collaborative care models that integrate with primary care practices
4. Advocacy and Professional Development
The policy landscape is still being shaped, and therapist voices matter. Engage with professional associations like the Alabama Counseling Association or the Alabama Psychological Association to stay informed and contribute to advocacy efforts. Attend workshops and continuing education focused on healthcare policy and practice management to stay ahead of changes.
5. Technology and Infrastructure
As transparency requirements increase and new plans emerge, having robust practice management systems becomes essential. Invest in technology that can:
- Track reimbursement rates across different plans and procedures
- Monitor denial patterns and appeal success rates
- Automate eligibility verification and prior authorization processes
- Generate reports that help you negotiate with payers
Looking Ahead: Opportunities Amidst Challenges
While the changes coming to Alabama’s healthcare landscape present challenges, they also offer significant opportunities for forward-thinking therapists. The potential influx of newly insured clients through ALLHealth could dramatically increase demand for mental health services. The antitrust settlement’s transparency requirements may provide leverage for improved reimbursement rates. And increased federal focus on parity enforcement could lead to more equitable treatment of mental health services.
Success in this new environment will require adaptability, strategic planning, and a commitment to staying informed. Therapists who proactively prepare for these changes—by updating their business practices, strengthening their documentation, diversifying their revenue streams, and engaging in advocacy—will be best positioned to thrive.












0 Comments