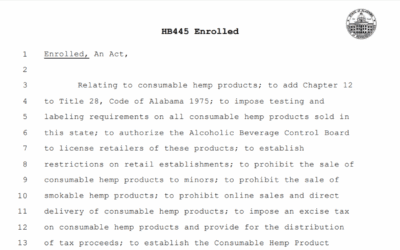
Alabama’s New Mental Health Consent Law: Understanding SB 101’s Full Scope
CRITICAL UPDATE: Alabama’s Senate Bill 101, which became law in May 2025 and takes effect October 1, 2025, represents a comprehensive overhaul of medical and mental health consent requirements for minors across ALL healthcare settings – not just schools.
SCOPE CLARIFICATION: Who SB 101 Actually Affects
✅ WHO IS AFFECTED BY SB 101:
- ALL healthcare providers (medical, dental, mental health)
- Private practice therapists and counselors
- Community mental health centers
- Hospital-based mental health professionals
- School counselors and school-based mental health providers
- Public school K-12 mental health services
- Agencies contracted to provide mental health services
- Any provider offering medical, dental, or mental health services to minors
❌ EXCEPTIONS – Services that maintain existing consent frameworks:
- Pregnancy prevention and treatment services
- Sexually transmitted infection services
- Alcohol and drug dependency treatment
Key Point: Unlike the original scope described in earlier interpretations, SB 101 affects the ENTIRE healthcare landscape in Alabama, fundamentally changing consent requirements for all mental health services provided to minors under 16 years of age.
Understanding SB 101: The Comprehensive Medical Consent Reform
Alabama’s Senate Bill 101 raises the age of medical consent from 14 to 16 years old for all medical, dental, and mental health services, while establishing new parental rights and notification requirements across all healthcare settings.
What the Law Requires
New Age of Consent: Minors must now be at least 16 years old (increased from 14) to independently consent to medical, dental, and mental health services.
Universal Parental Consent: All healthcare providers must now obtain parental consent for minors under 16, except in specific circumstances outlined below.
Parental Access Rights: Parents have the fundamental right to access their minor child’s health information and make healthcare decisions.
School-Specific Requirements:
- Annual written parental consent for school-based mental health services
- Local school boards must adopt policies for annual parental notification
- Distinction between individual counseling (requires consent) and group educational activities
Who Can Consent Independently
The following individuals may consent to their own healthcare without parental permission:
- Individuals 18 years of age or older
- Minors who have graduated from high school
- Minors who are married or divorced
- Pregnant minors
- Emancipated minors
- Independent minors who are:
- Not dependent on parents for support
- Living apart from parents
- Managing their own financial affairs
Exceptions to Parental Consent Requirements
Emergency Mental Health Services may be provided without parental consent when there is:
- Imminent threat to the health of the student or others
- Suspected abuse, neglect, or exploitation of the minor
- Immediate necessity for grief counseling
Services Maintaining Previous Consent Framework:
- Pregnancy prevention and treatment services
- Sexually transmitted infection testing and treatment
- Alcohol and drug dependency services
Parental Information Access Rights
Healthcare providers and governmental entities MUST provide parents access to their minor child’s health information EXCEPT when:
- Access is prohibited by court order
- The parent is under investigation for a crime against the child and law enforcement has requested information not be released
Implementation Timeline and Requirements
Effective Date: October 1, 2025
Healthcare Provider Requirements:
- Update consent policies and procedures
- Implement new age verification processes
- Establish clear protocols for emergency exceptions
- Train staff on new consent requirements
- Modify record-keeping and information sharing practices
School-Specific Requirements:
- Develop and adopt annual parental notification policies
- Create consent forms for mental health services
- Establish emergency intervention protocols
- Train all school counseling staff
Practical Implementation Guide for ALL Mental Health Providers
📋 Daily Practice Checklist
Before Providing Services to Any Minor:
- Verify minor’s age and eligibility for independent consent
- Check if minor meets exception criteria (married, pregnant, emancipated, independent)
- Obtain parental consent if minor is under 16 and doesn’t meet exceptions
- Document consent status in client records
- Verify emergency circumstances if providing services without parental consent
For Emergency Situations:
- Assess if situation meets emergency criteria
- Provide necessary immediate services
- Document emergency circumstances thoroughly
- Follow appropriate notification and reporting protocols
🤔 Decision Tree for ALL Providers
Is the client under 16 years old?
- No → Client may consent independently
- Yes → Does client meet exception criteria?
- Graduated high school → May consent independently
- Married/divorced → May consent independently
- Pregnant → May consent independently
- Emancipated → May consent independently
- Living independently → May consent independently
- None of the above → Parental consent required
Is this an emergency situation?
- Imminent threat to safety → Provide services, document emergency
- Suspected abuse/neglect → Provide services, follow reporting protocols
- Immediate grief counseling need → Provide services, document circumstances
💡 Service Categories Under SB 101
| Service Type | Consent Required | Notes |
|---|---|---|
| Individual therapy (under 16) | Yes (unless emergency or exception applies) | All individual therapeutic services |
| Group therapy (under 16) | Yes | Therapeutic group sessions |
| Crisis intervention | Emergency exception may apply | When client/others at imminent risk |
| Psychological testing (under 16) | Yes | Unless emergency circumstances |
| Family therapy (with minor under 16) | Yes | When minor is identified client |
| Medication management (under 16) | Yes | Psychiatric medications |
| School counseling (under 16) | Yes (annual written consent) | Individual counseling sessions |
| Classroom mental health education | No specific consent required | General educational presentations |
| Pregnancy/STI services | No (maintains previous framework) | Specific exception in law |
| Substance abuse treatment | No (maintains previous framework) | Specific exception in law |
Administrative Requirements for All Healthcare Settings
Policy Development Requirements
Consent Documentation Policies:
- Create standardized consent procedures for minors under 16
- Establish age verification protocols
- Design emergency services documentation systems
- Update confidentiality and information sharing policies
Parental Rights Policies:
- Develop procedures for parental access to minor’s health information
- Create systems for managing court orders and investigation exceptions
- Establish clear communication protocols with parents
Staff Training Requirements:
- Train all clinical staff on new consent requirements
- Update emergency intervention protocols
- Provide guidance on documentation requirements
- Review legal and ethical obligations
🔄 Sample Consent Scenarios for All Settings
Scenario 1: 15-year-old seeks therapy for depression at community mental health center
- Action: Verify no exception criteria met; obtain parental consent before providing services
- Documentation: Record parental consent and minor’s presenting concerns
Scenario 2: 16-year-old requests counseling at private practice
- Action: Minor may consent independently (meets age requirement)
- Documentation: Record minor’s independent consent
Scenario 3: 15-year-old in crisis at hospital emergency room
- Action: Assess as imminent threat; emergency exception applies
- Follow-up: Provide immediate stabilization; notify parents as clinically appropriate
Scenario 4: 15-year-old married minor seeks therapy
- Action: Married minor may consent independently
- Documentation: Verify marital status; record independent consent
Impact on Different Practice Settings
Private Practice Mental Health Providers
Immediate Actions Required:
- Update intake forms and consent documents
- Revise office policies and procedures
- Implement age verification processes
- Train staff on new requirements
- Update confidentiality agreements
- Establish parental communication protocols
Community Mental Health Centers
System-Wide Changes:
- Update electronic health record systems
- Revise clinic-wide consent procedures
- Implement staff training programs
- Establish emergency protocols
- Update crisis intervention policies
- Coordinate with child protective services protocols
Hospital-Based Mental Health Services
Integration Requirements:
- Align with hospital consent policies
- Update emergency department protocols
- Coordinate with medical teams on consent requirements
- Establish clear documentation standards
- Implement family notification procedures
School-Based Mental Health Services
Educational Setting Specific Requirements:
- Develop annual notification letters to parents
- Create opt-in consent forms for mental health services
- Establish clear boundaries between educational and therapeutic services
- Train school personnel on emergency exceptions
- Coordinate with community mental health providers for referrals
Legal and Ethical Considerations
Documentation Requirements
Universal Documentation Standards:
- Maintain detailed consent records for all minors
- Document emergency circumstances when providing services without consent
- Record specific exception criteria when minors consent independently
- Ensure compliance with HIPAA and state confidentiality laws
Emergency Services Documentation:
- Document specific emergency circumstances
- Record services provided and clinical rationale
- Note follow-up actions and notifications
- Maintain compliance with mandatory reporting requirements
Professional Boundaries and Scope
Clinical Practice Considerations:
- Understand interaction with existing professional ethics codes
- Recognize when external referrals are necessary
- Maintain appropriate therapeutic boundaries
- Navigate conflicts between parental rights and clinical judgment
Risk Management:
- Consult with legal counsel on implementation
- Review professional liability insurance coverage
- Establish supervision and consultation protocols
- Create quality assurance procedures
Communication Strategies
Parent Education and Engagement
Building Therapeutic Alliances:
- Explain the therapeutic value of mental health services
- Address concerns about confidentiality and treatment
- Provide education about adolescent mental health needs
- Offer opportunities for family involvement in treatment
Managing Resistance:
- Acknowledge parental concerns and values
- Provide evidence-based information about treatment effectiveness
- Explore alternative support options when consent is declined
- Maintain respectful communication channels
Minor Client Communication
Age-Appropriate Discussions:
- Explain consent requirements to adolescent clients
- Help minors understand their rights and limitations
- Encourage family communication about mental health needs
- Provide information about alternative resources
Navigating Confidentiality:
- Clarify what information will be shared with parents
- Establish clear boundaries for therapeutic confidentiality
- Help minors understand mandatory reporting requirements
- Support healthy family communication when clinically appropriate
Supporting Clients Without Parental Consent
Alternative Resources and Referrals
Community Resources:
- Maintain updated lists of services available to minors
- Establish relationships with providers offering excepted services
- Connect families with educational and support programs
- Provide information about crisis resources
Safety Planning:
- Develop safety protocols for at-risk minors
- Establish relationships with crisis intervention services
- Create procedures for emergency situations
- Maintain coordination with child protective services
Resources and Support for Providers
Professional Development
Training Opportunities:
- Alabama professional association workshops
- Legal compliance training programs
- Ethics and best practices seminars
- Crisis intervention certification programs
Ongoing Support:
- Peer consultation networks
- Professional supervision resources
- Legal guidance and consultation
- Professional liability guidance
External Partnerships
Community Collaboration:
- Develop referral networks with other providers
- Establish crisis intervention partnerships
- Create resource sharing agreements
- Coordinate care across service systems
Key Takeaways and Action Steps
Alabama’s SB 101 represents the most comprehensive change to minor consent laws in decades, affecting ALL healthcare providers serving minors. Success in implementation requires:
Immediate Action Items (Before October 1, 2025):
- Review and update all consent policies and procedures
- Train all clinical and administrative staff
- Modify intake forms and documentation systems
- Establish emergency intervention protocols
- Create parental communication procedures
- Update professional liability coverage as needed
- Establish legal consultation relationships
Long-term Success Factors:
- Comprehensive staff training and ongoing education
- Clear, consistent policy implementation
- Effective parent and family engagement strategies
- Strong community partnerships and referral networks
- Robust documentation and quality assurance procedures
- Regular policy review and updates
Bottom Line:
SB 101 fundamentally changes healthcare consent in Alabama by:
- Raising the age of independent medical consent from 14 to 16
- Requiring parental consent for ALL healthcare services to minors under 16
- Establishing comprehensive parental rights to healthcare information
- Maintaining specific exceptions for emergencies and certain services
- Affecting ALL healthcare providers, not just schools
Every healthcare provider serving minors in Alabama must update policies, procedures, and practices to comply with these new requirements by October 1, 2025.
This document is for informational purposes only and does not constitute legal advice. Healthcare providers should consult with legal counsel and professional associations for specific guidance on policy implementation and compliance with SB 101.












0 Comments