The Limits of the Biomedical Model in Mental Health
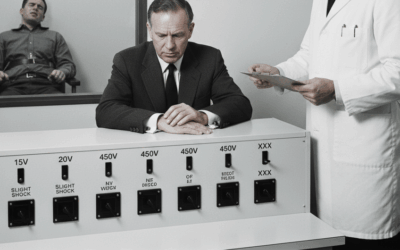
The biomedical model has dominated mental health treatment for decades, offering a structured framework for categorizing psychological symptoms into discrete disorders. While this approach has provided valuable standardization for diagnosis and treatment, emerging neuroscience research reveals its fundamental limitations in capturing the true complexity of human consciousness and psychological experience.
The biomedical model operates on a necessary but inherently reductive principle: grouping observable symptoms into diagnostic categories. However, these categories represent artificial constructs that often mask the underlying neurobiological diversity of mental health conditions. As we’ll explore, what appears uniform on the surface—conditions that check the same diagnostic boxes and respond to similar medications—may actually represent vastly different neurological processes.
The Hidden Heterogeneity of Mental Health Conditions: The ADHD Example
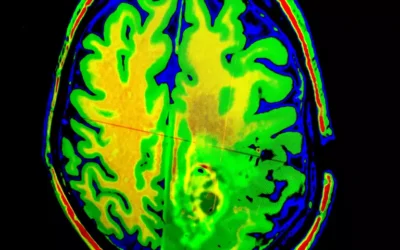
Perhaps no condition better illustrates the limitations of symptom-based categorization than Attention Deficit Hyperactivity Disorder (ADHD). While the DSM groups ADHD into three subtypes based on behavioral presentations (combined, inattentive, and hyperactive-impulsive), quantitative electroencephalogram (qEEG) brain mapping reveals that ADHD actually represents multiple distinct neurological patterns that can be measured through brain wave activity.
The Six Major qEEG Patterns in ADHD
Research has identified at least six distinct neurological profiles that can present as ADHD, each with unique brain wave signatures:
1. The Classic Elevated Theta/Beta Ratio Pattern
The most widely studied pattern shows elevated theta waves (4-8 Hz) and reduced beta waves (13.5-30 Hz), particularly at the Cz location (central midline of the scalp). This pattern has been found to discriminate ADHD patients from controls with sensitivity of 86% to 90% and specificity from 94% to 98%. However, this excessive theta/beta ratio cannot be considered a reliable diagnostic measure for all ADHD cases, as it represents only a substantial sub-group of ADHD patients.
2. Elevated Delta Power with Reduced Theta
Some ADHD patients show elevated delta power (1-4 Hz) with less theta activity. This pattern suggests deeper levels of brain wave slowing and may indicate more severe forms of inattention or brain dysfunction. Delta waves are typically associated with deep sleep states, so their presence during waking hours indicates significant underarousal.
3. Elevated Slow Alpha Pattern
Another subtype shows elevated slow alpha relative power (8-10 Hz). This pattern is particularly interesting because the increase in theta/beta ratio in some boys with ADHD is actually mediated by slow alpha peak frequency rather than true theta elevation. This finding suggests that what appears as elevated theta in some studies may actually be slowed alpha waves, representing a different neurological mechanism entirely.
4. Elevated Theta with Alpha/Beta Deficiencies
This pattern shows elevated theta combined with deficiencies in both alpha and beta relative power. This profile has been found primarily in children with the combined type of ADHD and is associated with hypoarousal. These individuals show excessive slow wave activity across multiple frequency bands.
5. Frontal Theta Pattern (Maturational Lag)
Research has identified increased frontal slow-wave EEG as a biological link to brain immaturity in hyperactive individuals, with ADHD demonstrating a developmental lag of up to 5 years for frontal cortical thickness. This maturational lag has been associated with elevated slow wave activity and deficiencies of fast wave, particularly in frontal regions.
6. High Beta/Hyperarousal Pattern
While less common, some ADHD patients show excess beta activity, which has been tentatively interpreted as hyperarousal. This pattern challenges the traditional view of ADHD as purely a disorder of underarousal and may represent a distinct neurological subtype requiring different treatment approaches.
Age and Development Factors
The neurological patterns in ADHD are not static but change with development:
- The theta/beta ratio did not differ significantly by ADHD status for youth but was significantly lower in adults with ADHD compared with controls
- Theta power and age share a negative correlation, demonstrating that age is a significant confounding factor in EEG abnormality in adult ADHD
- The brain’s functional architecture shows prominent maturational lag in ADHD, particularly in connections between the Default Mode Network and Frontoparietal Network
Comorbidity and Subtype Complications
The picture becomes even more complex when considering psychiatric comorbidities:
- ADHD subtype and psychiatric comorbidities such as disruptive behavior disorders and depression have opposing and significant mediating effects on the theta/beta ratio
- Different qEEG profiles may relate to specific neuropsychological profiles, suggesting a relationship between brain patterns and cognitive functioning
Clinical Implications of qEEG Heterogeneity
Understanding these distinct patterns has profound implications for treatment:
- Personalized Treatment Protocols: Based on brain map analysis, neurofeedback protocols can be developed that target specific symptoms linked to the functional networks shown to be abnormal or dysregulated
- Medication Response Prediction: Patients with a peak at 11.7 Hz might be responders to therapy with atomoxetine, while increased power in the beta band coupled with increased alpha seems to be related to non-responders
- Treatment Monitoring: The qEEG could be used for choosing and monitoring pharmacological treatments, with recommendations to discontinue atomoxetine if there is an increase of theta with treatment
Despite these neurological differences, all six patterns may:
- Meet the same DSM diagnostic criteria
- Present with similar behavioral symptoms
- Initially respond to the same stimulant medications
This finding reveals the fundamental limitation of the biomedical model: it groups together neurologically distinct conditions based on surface symptoms rather than underlying brain mechanisms. The technology shows that what we call “ADHD” is not a single condition but a collection of different brain network dysfunctions that manifest similarly on the behavioral level.
Understanding Psychology as Biodynamic Forces
Leading neuroscientists are revolutionizing our understanding of mental processes by viewing them not as static conditions but as dynamic interactions between brain networks, bodily states, and environmental factors.
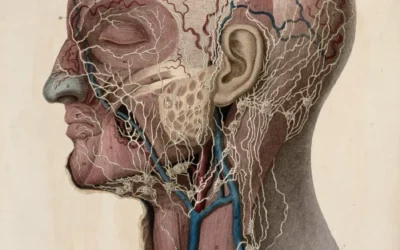
Antonio Damasio: The Embodied Mind
Antonio Damasio‘s groundbreaking research demonstrates that feelings are “mental experiences of body states,” arising as the brain interprets emotions, which are themselves physical states emerging from the body’s responses to external stimuli. His work challenges the traditional separation of mind and body, showing that:
- Emotions are essential for rational decision-making, not obstacles to it
- Homeostasis—the body’s drive to maintain balance and thrive—serves as “the monitors and arbiters of cultural invention”
- Consciousness emerges from the continuous interaction between the nervous system and the body
Damasio’s somatic marker hypothesis reveals that our bodies generate emotional signals that guide decision-making before conscious reasoning occurs. This understanding suggests that effective therapy must address both cognitive and somatic experiences.
Michael Gazzaniga: The Interpreter and Multiple Selves
Michael Gazzaniga’s split-brain research revealed that the left and right hemispheres of the brain have distinct information-processing capabilities. His work identified the “left hemisphere interpreter”—a system that constantly creates coherent narratives from our experiences, even when those experiences arise from disconnected brain processes.
This research demonstrates that:
- We are not singular, unified selves but collections of semi-independent processing systems
- Consciousness can be split, suggesting that what we experience as a unified self is actually constructed from multiple neural processes
- The brain actively creates meaning and coherence, sometimes generating explanations for behaviors whose true causes are unconscious
Joseph LeDoux: Survival Circuits vs. Emotional Experience
Joseph LeDoux’s research on the amygdala and fear circuits provides crucial insights into how we process threats and emotions. His work shows that the amygdala may trigger physical responses to threats, but the conscious experience of fear involves higher-order brain circuits in the prefrontal cortex.
LeDoux distinguishes between:
- Survival circuits that produce automatic defensive responses
- The subjective, conscious experience of emotions
- Different brain systems for threat detection versus the feeling of being afraid
This two-system view has profound implications for treating anxiety and trauma, suggesting that effective therapy must address both automatic threat responses and conscious emotional processing.
Brain Networks: The Dynamic Architecture of Mind
Modern neuroscience reveals that the brain operates through dynamic networks that can colonize different structures depending on the task at hand. Rather than fixed locations for specific functions, we see flexible systems that adapt and reorganize.
Key insights about brain networks include:
- Networks for attention, executive function, memory, and emotion communicate continuously
- Functional connections between brain regions are key for optimal brain functioning
- Disruptions in network connectivity often underlie psychological symptoms
- The same symptoms can arise from different network dysfunctions
Understanding these networks allows therapists to conceptualize mental health issues as problems of integration and communication rather than localized deficits.
The Indirect Pathway: When Filtering Fails
The basal ganglia’s indirect pathway serves as a crucial filtering mechanism in the brain. This pathway involves GABAergic neurons that help filter out unnecessary information and regulate responses. When this filtering system is too “wide open,” it can lead to conditions characterized by sensory overload or unusual perceptual experiences.
Research shows that dysfunction within basal ganglia circuits may contribute to stereotyped movements, reduced attentional control, and altered social processing in conditions like autism spectrum disorder. In schizophrenia, patients show markedly decreased activation in the basal ganglia across task domains, suggesting broad dysfunction in this filtering system.
However, this “dysfunction” isn’t always negative. A wider indirect pathway may also confer:
- Enhanced pattern recognition abilities
- Greater sensitivity to environmental stimuli
- Access to information typically filtered out by others
- Creative insights arising from unusual connections
Symptoms as Biodynamic Expressions
Understanding symptoms as expressions of underlying biodynamic forces rather than simply problems to eliminate opens new therapeutic possibilities. Depression, for instance, might serve adaptive functions:
- Forcing analytical thinking about complex problems
- Promoting social withdrawal to conserve energy
- Signaling the need for life changes
- Teaching us about emotions we typically avoid
As Damasio notes, basic feelings like pain and pleasure are fundamental to life regulation and cannot be separated from our cognitive processes. Sometimes, going “all the way through” difficult emotions provides insights that medication alone cannot offer.
Toward a New Model of Psychotherapy
A revised model of psychotherapy must acknowledge several key principles:
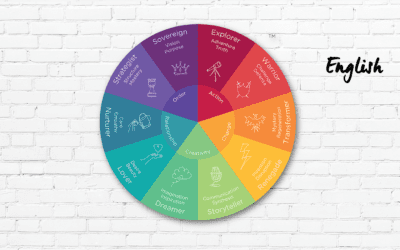
1. Embrace Neurological Diversity
Recognize that similar symptoms can arise from different neural patterns. Treatment should be tailored to underlying network dysfunctions, not just surface presentations.
2. Integrate Multiple Levels of Experience
Effective therapy addresses:
- Cognitive patterns (thoughts and beliefs)
- Somatic experiences (bodily sensations and emotions)
- Network dynamics (how different brain systems communicate)
- Meaning-making processes (the interpreter function)
3. Respect Adaptive Functions
Many “symptoms” represent adaptive responses that serve protective or regulatory functions. Understanding these functions is crucial before attempting to eliminate them.
4. Work with Brain Networks
Therapists can learn to recognize network patterns without expensive brain imaging:
- Attention difficulties may signal default mode network issues
- Emotional dysregulation often involves limbic-cortical disconnection
- Sensory sensitivities might indicate filtering differences
5. Honor Individual Neurodiversity
What’s pathological in one context may be advantageous in another. A wider indirect pathway might create challenges in a noisy classroom but advantages in pattern recognition or creative fields.
Clinical Implications: Practical Applications
Assessment Beyond Categories
Instead of simply checking diagnostic criteria, clinicians should explore:
- How symptoms manifest across different contexts
- The client’s unique sensory and processing profile
- Network-based patterns (attention, emotion regulation, executive function)
- Somatic experiences and body-based patterns
Treatment Matching
Different network dysfunctions require different approaches:
- Attention network issues might benefit from mindfulness or neurofeedback
- Emotional processing differences could respond to somatic therapies
- Executive function challenges might improve with cognitive training
- Integration difficulties often require body-based or expressive therapies
Therapeutic Stance
Adopt a curious, exploratory approach that:
- Views symptoms as information about underlying processes
- Collaborates with clients to understand their unique neurology
- Respects neurodiversity while addressing genuine suffering
- Integrates multiple therapeutic modalities based on network needs
The Future of Mental Health Treatment
As our understanding of brain networks and consciousness evolves, psychotherapy must evolve as well. The biomedical model served an important purpose in standardizing diagnosis and treatment, but we now know that:
- Mental health conditions are heterogeneous at the neurological level
- Consciousness emerges from complex interactions between brain, body, and environment
- Symptoms often serve adaptive functions that deserve respect
- Effective treatment must address multiple levels of organization
By embracing this complexity, we can develop more nuanced, effective approaches that honor both the universal patterns and individual uniqueness of human psychological experience. The future of psychotherapy lies not in more precise diagnostic categories but in understanding the dynamic, interconnected nature of consciousness itself.
As we continue to uncover the intricate relationships between neural networks, bodily experience, and conscious awareness, one thing becomes clear: the mind cannot be reduced to a collection of symptoms or a set of diagnostic criteria. It is a living, dynamic system that requires equally dynamic and integrative approaches to healing.
Bibliography
Andrews, P. W., & Thomson Jr, J. A. (2009). The bright side of being blue: depression as an adaptation for analyzing complex problems. Psychological Review, 116(3), 620-654.
Aron, A. R., & Poldrack, R. A. (2006). Cortical and subcortical contributions to stop signal response inhibition: role of the subthalamic nucleus. Journal of Neuroscience, 26(9), 2424-2433.
Barry, R. J., Clarke, A. R., & Johnstone, S. J. (2003). A review of electrophysiology in attention-deficit/hyperactivity disorder: I. Qualitative and quantitative electroencephalography. Clinical Neurophysiology, 114(2), 171-183.
Bechara, A., Damasio, H., Tranel, D., & Damasio, A. R. (1997). Deciding advantageously before knowing the advantageous strategy. Science, 275(5304), 1293-1295.
Bernard, J. A., Russell, C. E., Newberry, R. E., Goen, J. R., & Mittal, V. A. (2017). Patients with schizophrenia show aberrant patterns of basal ganglia activation: Evidence from ALE meta-analysis. NeuroImage: Clinical, 14, 450-463.
Damasio, A. (1994). Descartes’ Error: Emotion, Reason, and the Human Brain. New York: Putnam.
Damasio, A. (1999). The Feeling of What Happens: Body and Emotion in the Making of Consciousness. New York: Harcourt.
Damasio, A. (2003). Looking for Spinoza: Joy, Sorrow, and the Feeling Brain. New York: Harcourt.
Damasio, A. (2010). Self Comes to Mind: Constructing the Conscious Brain. New York: Pantheon.
Damasio, A. (2018). The Strange Order of Things: Life, Feeling, and the Making of Cultures. New York: Pantheon.
Damasio, A., & Carvalho, G. B. (2013). The nature of feelings: evolutionary and neurobiological origins. Nature Reviews Neuroscience, 14(2), 143-152.
Damasio, A., & Meyer, K. (2009). Consciousness: An overview of the phenomenon and of its possible neural basis. In S. Laureys & G. Tononi (Eds.), The Neurology of Consciousness (pp. 3-14). Academic Press.
Gazzaniga, M. S. (1985). The Social Brain: Discovering the Networks of the Mind. New York: Basic Books.
Gazzaniga, M. S. (2000). Cerebral specialization and interhemispheric communication: Does the corpus callosum enable the human condition? Brain, 123(7), 1293-1326.
Gazzaniga, M. S. (2005). Forty-five years of split-brain research and still going strong. Nature Reviews Neuroscience, 6(8), 653-659.
Gazzaniga, M. S. (2011). Who’s in Charge?: Free Will and the Science of the Brain. New York: Ecco.
Gazzaniga, M. S. (2018). The Consciousness Instinct: Unraveling the Mystery of How the Brain Makes Mind. New York: Farrar, Straus and Giroux.
Gazzaniga, M. S., & LeDoux, J. E. (1978). The Integrated Mind. New York: Plenum Press.
Gazzaniga, M. S., Bogen, J. E., & Sperry, R. W. (1962). Some functional effects of sectioning the cerebral commissures in man. Proceedings of the National Academy of Sciences, 48(10), 1765-1769.
Gerfen, C. R. (1992). The neostriatal mosaic: multiple levels of compartmental organization in the basal ganglia. Annual Review of Neuroscience, 15(1), 285-320.
Hughes, J. R., & John, E. R. (1999). Conventional and quantitative electroencephalography in psychiatry. The Journal of Neuropsychiatry and Clinical Neurosciences, 11(2), 190-208.
Hutcheson, N. L., Clark, D. G., Bolding, M. S., White, D. M., & Lahti, A. C. (2014). Basal ganglia volume in unmedicated patients with schizophrenia is associated with treatment response to antipsychotic medication. Psychiatry Research: Neuroimaging, 221(1), 6-12.
LeDoux, J. E. (1996). The Emotional Brain: The Mysterious Underpinnings of Emotional Life. New York: Simon and Schuster.
LeDoux, J. E. (2000). Emotion circuits in the brain. Annual Review of Neuroscience, 23(1), 155-184.
LeDoux, J. E. (2003). The emotional brain, fear, and the amygdala. Cellular and Molecular Neurobiology, 23(4-5), 727-738.
LeDoux, J. E. (2012). Rethinking the emotional brain. Neuron, 73(4), 653-676.
LeDoux, J. E. (2015). Anxious: Using the Brain to Understand and Treat Fear and Anxiety. New York: Viking.
LeDoux, J. E. (2019). The Deep History of Ourselves: The Four-Billion-Year Story of How We Got Conscious Brains. New York: Viking.
LeDoux, J. E., & Pine, D. S. (2016). Using neuroscience to help understand fear and anxiety: a two-system framework. American Journal of Psychiatry, 173(11), 1083-1093.
Loo, S. K., & Makeig, S. (2012). Clinical utility of EEG in attention-deficit/hyperactivity disorder: a research update. Neurotherapeutics, 9(3), 569-587.
Lubar, J. F. (1991). Discourse on the development of EEG diagnostics and biofeedback for attention-deficit/hyperactivity disorders. Biofeedback and Self-regulation, 16(3), 201-225.
Macpherson, T., & Hikida, T. (2019). Role of basal ganglia neurocircuitry in the pathology of psychiatric disorders. Psychiatry and Clinical Neurosciences, 73(6), 289-301.
Nambu, A., Tokuno, H., & Takada, M. (2002). Functional significance of the cortico–subthalamo–pallidal ‘hyperdirect’ pathway. Neuroscience Research, 43(2), 111-117.
Oertel-Knöchel, V., Knöchel, C., Matura, S., Rotarska-Jagiela, A., Magerkurth, J., Prvulovic, D., … & Linden, D. E. (2012). Cortical-basal ganglia imbalance in schizophrenia patients and unaffected first-degree relatives. Schizophrenia Research, 138(2-3), 120-127.
Parent, A., & Hazrati, L. N. (1995). Functional anatomy of the basal ganglia. I. The cortico-basal ganglia-thalamo-cortical loop. Brain Research Reviews, 20(1), 91-127.
Perez-Costas, E., Melendez-Ferro, M., & Roberts, R. C. (2010). Basal ganglia pathology in schizophrenia: dopamine connections and anomalies. Journal of Neurochemistry, 113(2), 287-302.
Phelps, E. A., & LeDoux, J. E. (2005). Contributions of the amygdala to emotion processing: from animal models to human behavior. Neuron, 48(2), 175-187.
Roiz-Santiáñez, R., Ayesa-Arriola, R., Tordesillas-Gutiérrez, D., Ortiz-García de la Foz, V., Pérez-Iglesias, R., Pazos, A., … & Crespo-Facorro, B. (2013). Three-year longitudinal population-based volumetric MRI study in first-episode schizophrenia spectrum patients. Psychological Medicine, 44(8), 1591-1604.
Scheepers, F. E., Gispen de Wied, C. C., Hulshoff Pol, H. E., van de Flier, W., van der Linden, J. A., & Kahn, R. S. (2001). The effect of clozapine on caudate nucleus volume in schizophrenic patients previously treated with typical antipsychotics. Neuropsychopharmacology, 24(1), 47-54.
Shen, H. H. (2015). Core concepts: resting-state connectivity. Proceedings of the National Academy of Sciences, 112(46), 14115-14116.
Sperry, R. W. (1961). Cerebral organization and behavior. Science, 133(3466), 1749-1757.
Tanimura, Y., King, M. A., Williams, D. K., & Lewis, M. H. (2011). Development of repetitive behavior in a mouse model: roles of indirect and striosomal basal ganglia pathways. International Journal of Developmental Neuroscience, 29(4), 461-467.
van der Kolk, B. (2014). The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma. New York: Viking.
Walther, S., Federspiel, A., Horn, H., Razavi, N., Wiest, R., Dierks, T., … & Müller, T. J. (2011). Resting state cerebral blood flow and objective motor activity reveal basal ganglia dysfunction in schizophrenia. Psychiatry Research: Neuroimaging, 192(2), 117-124.
Tags
psychotherapy revision, biomedical model limitations, qEEG brain mapping, ADHD neurological subtypes, Antonio Damasio consciousness, neural networks psychology, indirect pathway brain, basal ganglia function, neurodiversity mental health, brain network dynamics, embodied cognition therapy, Michael Gazzaniga split-brain, Joseph LeDoux emotion, integrative psychotherapy approaches, neuroplasticity mental health














0 Comments