Do I have Schizophrenia?

Schizophrenia: Dispelling Myths and Understanding the Complex Mental Disorder
What is Schizophrenia?
Schizophrenia is a severe, chronic mental disorder characterized by disturbances in thought, perception, emotions, and behavior 1. It affects approximately 1% of the global population and typically emerges in late adolescence or early adulthood 2. While often misunderstood, schizophrenia is not a “split personality” but rather a complex condition that causes a disconnect from reality.
The exact causes of schizophrenia remain unclear, but research suggests a combination of genetic, environmental, and neurochemical factors 3. Studies have identified numerous risk genes, and individuals with a family history of schizophrenia have a higher likelihood of developing the disorder 4. Environmental factors like prenatal infections, birth complications, and psychosocial stressors may also play a role.
Positive Symptoms
Positive symptoms refer to psychotic behaviors not generally seen in healthy people [2]. These include:
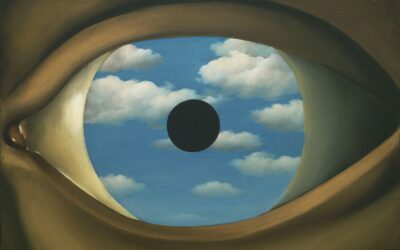
- Hallucinations: Sensations that appear real but are created by the mind, such as hearing voices, seeing things that aren’t there, or feeling phantom sensations. Auditory hallucinations are most common.
- Delusions: False, fixed beliefs not based in reality. For example, thinking others are plotting against you (paranoid delusion) or believing you have extraordinary powers.
- Thought disorders: Dysfunctional ways of thinking, such as loose associations, derailment or tangentiality. Speech may be incoherent or jump rapidly between unrelated topics.
- Movement disorders: Agitated body movements or repetitive motions. The person may appear clumsy or exhibit involuntary movements like grimacing.
Negative Symptoms
Negative symptoms disrupt normal behaviors and emotions [3]. These include:
- Flat affect: Reduced emotional expression or reactions. The person may speak in a monotone, avoid eye contact, or seem unresponsive.
- Anhedonia: Loss of interest or pleasure in daily activities. Things that were once enjoyable no longer bring satisfaction.
- Asociality: Lack of interest in social relationships. The person withdraws, ceasing communication and interaction with friends and family.
- Avolition: Decreased motivation and apathy. Simple tasks like personal hygiene become difficult. Decision-making is impaired.
- Alogia: Poverty of speech. Responses to questions may be brief, empty, or completely absent. Thoughts are not fluidly translated into words.
Cognitive Symptoms
Cognitive symptoms are subtle and often go unrecognized [4]. These include:
- Poor executive functioning: Difficulty understanding information, making decisions, and problem-solving. Abstract thinking and flexibility of thought are impaired.
- Trouble focusing: Problems with concentration, attention and working memory. Conversations and tasks become challenging to follow and complete.
- Impaired memory: Difficulty retaining recently learned verbal or non-verbal information. Both short and long-term memory are affected.
Pharmacotherapy for Schizophrenia
Antipsychotic medications are the cornerstone of schizophrenia treatment. They work by modulating neurotransmitters in the brain, particularly dopamine and serotonin, to reduce psychotic symptoms like hallucinations and delusions [2]. Two main classes exist:
- First-generation (typical) antipsychotics such as chlorpromazine and haloperidol have been used since the 1950s. While effective, they carry a higher risk of neurological side effects like extrapyramidal symptoms (EPS) and tardive dyskinesia [3].
- Second-generation (atypical) antipsychotics like risperidone, olanzapine, and aripiprazole emerged in the 1990s. They pose a lower EPS risk but are associated with metabolic side effects like weight gain, diabetes, and high cholesterol [4].
Clozapine, an atypical antipsychotic, is considered the gold standard for treatment-resistant schizophrenia but requires close monitoring due to the risk of agranulocytosis [5].
Psychosocial Interventions
Medication alone is not enough. Psychotherapy and psychosocial support are essential for developing coping skills, improving functioning, and facilitating recovery [6]. Evidence-based interventions include:
- Cognitive Behavioral Therapy (CBT): Helps identify and change distorted thoughts and perceptions. Useful for managing persistent symptoms and preventing relapse [7].
- Family Psychoeducation: Educates family about the illness, improves communication, and reduces stress within the family unit [8]. Leads to better medication adherence and lower relapse rates.
- Social Skills Training: Teaches communication, assertiveness, and conflict resolution to improve social interactions and vocational success [9].
- Supported Employment: Assists with finding and maintaining competitive employment. Linked to better self-esteem, symptom control, and overall functioning [10].
Coordinated Specialty Care
For those experiencing first-episode psychosis, Coordinated Specialty Care (CSC) offers a comprehensive, team-based approach. CSC integrates medication management, psychotherapy, family education and support, case management, and employment/education services [11]. Research shows CSC leads to better clinical and functional outcomes compared to standard care [12].
Dispelling Common Myths
Despite growing awareness, schizophrenia remains shrouded in myths and misconceptions. Let’s shed light on some of the most pervasive ones:
Myth 1: Schizophrenia means having multiple personalities
Schizophrenia and dissociative identity disorder (formerly known as multiple personality disorder) are distinct conditions 6. Schizophrenia involves a disconnect from reality, not a fragmentation of identity.
Myth 2: People with schizophrenia are dangerous and violent
Research indicates most individuals with schizophrenia are not violent and are more often victims than perpetrators of violence 7. Co-occurring substance abuse and history of childhood trauma can increase risk of violent behavior 8.
Myth 3: Schizophrenia stems from poor parenting
While family environment may influence coping and recovery, parenting styles do not cause schizophrenia 9. The outdated concept of “schizophrenogenic mothers” has been thoroughly debunked 10.
Recognizing Schizophrenia Symptoms
Schizophrenia presents with diverse symptoms, which are typically categorized as follows 11:
Positive symptoms:
Include hallucinations (sensory experiences with no external cause), delusions (firmly held false beliefs), and disorganized speech or behavior. These psychotic symptoms represent an excess or distortion of normal functions.
Negative symptoms:
Reflect a diminishment or loss of typical functions, such as blunted affect (reduced emotional expression), alogia (decreased speech), anhedonia (inability to feel pleasure), and avolition (lack of motivation).
Cognitive symptoms:
Involve difficulties with attention, working memory, executive functions (planning, organizing, decision-making), and social cognition. These deficits often emerge before positive symptoms and can significantly impact daily functioning 12.
Integrated Treatment Approaches
While there is no cure for schizophrenia, recovery is possible with comprehensive, individualized treatment 13. The most effective approaches involve a combination of pharmacological, psychological, and psychosocial interventions:
Antipsychotic medications are the cornerstone of treatment, helping to manage psychotic symptoms by regulating neurotransmitters like dopamine and serotonin. Second-generation or atypical antipsychotics are often preferred due to their lower risk of extrapyramidal side effects 14.
Cognitive-behavioral therapy (CBT) has shown promise in reducing the severity and distress associated with psychotic symptoms, enhancing coping skills, and improving functioning 15. Family psychoeducation and support, social skills training, and vocational rehabilitation are also key components of psychosocial treatment 16.
Coordinated specialty care (CSC) is an evidence-based, recovery-oriented treatment model that integrates pharmacotherapy, psychotherapy, case management, family education and support, and supported employment/education services 17. CSC has been shown to improve clinical and functional outcomes, particularly for individuals experiencing their first episode of psychosis 18.
Despite the availability of effective treatments, many individuals with schizophrenia face significant barriers to care, including stigma, lack of awareness, and limited access to specialized services 19. Overcoming these obstacles requires a multi-pronged approach involving public education, early intervention, and advocacy for accessible, high-quality mental health care.
Challenging the Dominant Paradigm
The medical model of schizophrenia, which emphasizes biological causes and pharmacological treatments, has faced criticism for its reductionistic view of the disorder 20. Some argue that this framework neglects the complex psychosocial factors that contribute to the development and maintenance of schizophrenia 21.
Critics also question the long-term efficacy and safety of antipsychotic medications, citing issues like treatment resistance, cognitive impairment, and metabolic side effects 22. Some advocate for a more holistic, person-centered approach that prioritizes empowerment, social inclusion, and recovery-oriented practices 23.
While these critiques raise important considerations, the biopsychosocial model remains the most empirically supported framework for understanding and treating schizophrenia 24. This integrative approach recognizes the complex interplay of biological, psychological, and social factors in the etiology and treatment of the disorder.
Promoting Hope and Recovery
Schizophrenia is a challenging condition that impacts millions of individuals and families worldwide. By dispelling myths, increasing public awareness, and advocating for accessible, evidence-based care, we can work towards improving outcomes and quality of life for those affected.
Recovery from schizophrenia is a ongoing process that requires a comprehensive, individualized approach addressing both symptoms and functional impairments. With appropriate support, many individuals with schizophrenia can lead fulfilling, productive lives and achieve their personal goals 25.
References
- National Institute of Mental Health. (2020). Schizophrenia. https://www.nimh.nih.gov/health/topics/schizophrenia
- World Health Organization. (2022). Schizophrenia. https://www.who.int/news-room/fact-sheets/detail/schizophrenia
- American Psychiatric Association. (2020). What is Schizophrenia? https://www.psychiatry.org/patients-families/schizophrenia/what-is-schizophrenia
- Giusti-Rodríguez, P., & Sullivan, P. F. (2013). The genomics of schizophrenia: update and implications. The Journal of clinical investigation, 123(11), 4557–4563. https://doi.org/10.1172/JCI66031
- Brown A. S. (2011). The environment and susceptibility to schizophrenia. Progress in neurobiology, 93(1), 23–58. https://doi.org/10.1016/j.pneurobio.2010.09.003
- National Alliance on Mental Illness. (n.d.). Dissociative Disorders. https://www.nami.org/About-Mental-Illness/Mental-Health-Conditions/Dissociative-Disorders
- Fazel, S., Gulati, G., Linsell, L., Geddes, J. R., & Grann, M. (2009). Schizophrenia and violence: systematic review and meta-analysis. PLoS medicine, 6(8), e1000120. https://doi.org/10.1371/journal.pmed.1000120
- Volavka J. (2013). Violence in schizophrenia and bipolar disorder. Psychiatria Danubina, 25(1), 24–33.
- Patel, K. (2021). Can “Bad” Parenting Cause Schizophrenia? Psychology Today. https://www.psychologytoday.com/us/blog/fighting-fear/202109/can-bad-parenting-cause-schizophrenia
- Harrington, A. (2019). Mind Fixers: Psychiatry’s Troubled Search for the Biology of Mental Illness. W. W. Norton & Company.
- American Psychiatric Association. (2020). What are the symptoms of schizophrenia? https://www.psychiatry.org/patients-families/schizophrenia/what-are-the-symptoms-of-schizophrenia
- Reichenberg, A., & Harvey, P. D. (2007). Neuropsychological impairments in schizophrenia: Integration of performance-based and brain imaging findings. Psychological bulletin, 133(5), 833–858. https://doi.org/10.1037/0033-2909.133.5.833
- Novotney, A. (2015). Integrated treatment for schizophrenia. Monitor on Psychology, 46(3). https://www.apa.org/monitor/2015/03/treatment-schizophrenia
- Divac, N., Prostran, M., Jakovcevski, I., & Cerovac, N. (2014). Second-generation antipsychotics and extrapyramidal adverse effects. BioMed research international, 2014, 656370. https://doi.org/10.1155/2014/656370
- Bighelli, I., Salanti, G., Huhn, M., Schneider-Thoma, J., Krause, M., Reitmeir, C., Wallis, S., Schwermann, F., Pitschel-Walz, G., Barbui, C., Furukawa, T. A., & Leucht, S. (2018). Psychological interventions to reduce positive symptoms in schizophrenia: systematic review and network meta-analysis. World psychiatry, 17(3), 316–329. https://doi.org/10.1002/wps.20577
- Bauml, J., Pitschel-Walz, G., Volz, A., Luscher, S., Rentrop, M., Kissling, W., & Jahn, T. (2016). Psychoeducation Improves Compliance and Outcome in Schizophrenia Without an Increase of Adverse Side Effects: A 7-Year Follow-up of the Munich PIP-Study. Schizophrenia Bulletin, 42(suppl_1), S62–S70. https://doi.org/10.1093/schbul/sbw008
- National Institute of Mental Health. (2018). What is Coordinated Specialty Care (CSC)? https://www.nimh.nih.gov/health/topics/schizophrenia/raise/what-is-coordinated-specialty-care-csc
- Kane, J. M., Robinson, D. G., Schooler, N. R., Mueser, K. T., Penn, D. L., Rosenheck, R. A., Addington, J., Brunette, M. F., Correll, C. U., Estroff, S. E., Marcy, P., Robinson, J., Meyer-Kalos, P. S., Gottlieb, J. D., Glynn, S. M., Lynde, D. W., Pipes, R., Kurian, B. T., Miller, A. L., Azrin, S. T., … Heinssen, R. K. (2016). Comprehensive Versus Usual Community Care for First-Episode Psychosis: 2-Year Outcomes From the NIMH RAISE Early Treatment Program. American Journal of Psychiatry, 173(4), 362–372. https://doi.org/10.1176/appi.ajp.2015.15050632
- Thornicroft, G., Brohan, E., Rose, D., Sartorius, N., Leese, M., & INDIGO Study Group (2009). Global pattern of experienced and anticipated discrimination against people with schizophrenia: a cross-sectional survey. Lancet (London, England), 373(9661), 408–415. https://doi.org/10.1016/S0140-6736(08)61817-6
- van Os, J., Kenis, G., & Rutten, B. P. (2010). The environment and schizophrenia. Nature, 468(7321), 203–212. https://doi.org/10.1038/nature09563
- Larsen, J. A. (2013). Integrating clinical and epidemiological research in psychosis: from risk factors to prediction. Psychosis, 5(sup1), 62-71. https://doi.org/10.1080/17522439.2013.827985
- Friedman, J. I., Soleimani, L., McGonigle, D. P., Egol, C., & Silverstein, S. M. (2014). Pharmacological treatments of non-substance-withdrawal delirium: a systematic review of prospective trials. The American Journal of Psychiatry, 171(2), 151–159. https://doi.org/10.1176/appi.ajp.2013.13040458
- Leamy, M., Bird, V., Le Boutillier, C., Williams, J., & Slade, M. (2011). Conceptual framework for personal recovery in mental health: systematic review and narrative synthesis. The British journal of psychiatry : the journal of mental science, 199(6), 445–452. https://doi.org/10.1192/bjp.bp.110.083733
- Patel, K. R., Cherian, J., Gohil, K., & Atkinson, D. (2014). Schizophrenia: Overview and Treatment Options. Pharmacy and Therapeutics, 39(9), 638–645.
- Jääskeläinen, E., Juola, P., Hirvonen, N., McGrath, J. J., Saha, S., Isohanni, M., Veijola, J., & Miettunen, J. (2013). A systematic review and meta-analysis of recovery in schizophrenia.
- Patel, K. R., Cherian, J., Gohil, K., & Atkinson, D. (2014). Schizophrenia: overview and treatment options. P & T: A peer-reviewed journal for formulary management, 39(9), 638–645.
- Stępnicki, P., Kondej, M., & Kaczor, A. A. (2018). Current Concepts and Treatments of Schizophrenia. Molecules (Basel, Switzerland), 23(8), 2087. https://doi.org/10.3390/molecules23082087
- Muench, J., & Hamer, A. M. (2010). Adverse effects of antipsychotic medications. American family physician, 81(5), 617–622.
- Solmi, M., Murru, A., Pacchiarotti, I., Undurraga, J., Veronese, N., Fornaro, M., Stubbs, B., Monaco, F., Vieta, E., Seeman, M. V., Correll, C. U., & Carvalho, A. F. (2017). Safety, tolerability, and risks associated with first- and second-generation antipsychotics: a state-of-the-art clinical review. Therapeutics and clinical risk management, 13, 757–777. https://doi.org/10.2147/TCRM.S117321
- De Berardis, D., Rapini, G., Olivieri, L., Di Nicola, D., Tomasetti, C., Valchera, A., Fornaro, M., Di Fabio, F., Perna, G., Di Nicola, M., Serafini, G., Carano, A., Pompili, M., Vellante, F., Orsolini, L., Martinotti, G., & Di Giannantonio, M. (2018). Safety of antipsychotics for the treatment of schizophrenia: a focus on the adverse effects of clozapine. Therapeutic advances in drug safety, 9(5), 237–256. https://doi.org/10.1177/2042098618756261
- Bighelli, I., Ostuzzi, G., Girlanda, F., Cipriani, A., Becker, T., Koesters, M., & Barbui, C. (2016). Implementation of treatment guidelines for specialist mental health care. The Cochrane database of systematic reviews, 12(12), CD009780. https://doi.org/10.1002/14651858.CD009780.pub3
- Kingdon, D., & Turkington, D. (2005). Cognitive-behavioural therapy of schizophrenia. Guilford Press.
- McFarlane W. R. (2016). Family Interventions for Schizophrenia and the Psychoses: A Review. Family process, 55(3), 460–482. https://doi.org/10.1111/famp.12235
- Turner, D. T., McGlanaghy, E., Cuijpers, P., van der Gaag, M., Karyotaki, E., & MacBeth, A. (2018). A Meta-Analysis of Social Skills Training and Related Interventions for Psychosis. Schizophrenia bulletin, 44(3), 475–491. https://doi.org/10.1093/schbul/sbx146
- Suijkerbuijk, Y., Schaafsma, F. G., van Mechelen, J. C., Ojajärvi, A., Corbière, M., & Anema, J. R. (2017). Interventions for obtaining and maintaining employment in adults with severe mental illness, a network meta-analysis. The Cochrane database of systematic reviews, 9(9), CD011867. https://doi.org/10.1002/14651858.CD011867.pub2
- National Institute of Mental Health. (2018). What is Coordinated Specialty Care (CSC)? https://www.nimh.nih.gov/health/topics/schizophrenia/raise/what-is-coordinated-specialty-care-csc
- Kane, J. M., Robinson, D. G., Schooler, N. R., Mueser, K. T., Penn, D. L., Rosenheck, R. A., Addington, J., Brunette, M. F., Correll, C. U., Estroff, S. E., Marcy, P., Robinson, J., Meyer-Kalos, P. S., Gottlieb, J. D., Glynn, S. M., Lynde, D. W., Pipes, R., Kurian, B. T., Miller, A. L., Azrin, S. T., … Heinssen, R. K. (2016
- Owen, M. J., Sawa, A., & Mortensen, P. B. (2016). Schizophrenia. Lancet (London, England), 388(10039), 86–97. https://doi.org/10.1016/S0140-6736(15)01121-6
- National Institute of Mental Health. (2020). Schizophrenia. https://www.nimh.nih.gov/health/topics/schizophrenia
- American Psychiatric Association. (2013). Schizophrenia spectrum and other psychotic disorders. In Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596.dsm02
- Reichenberg, A., & Harvey, P. D. (2007). Neuropsychological impairments in schizophrenia: Integration of performance-based and brain imaging findings. Psychological bulletin, 133(5), 833–858. https://doi.org/10.1037/0033-2909.133.5.833
Types of Therapy















0 Comments