
The Ultimate Guide to Nutritional Psychiatry: Supplements, Gut Health, and the Brain
In the evolving landscape of mental health treatment, the focus is shifting from a purely neurochemical model to a holistic view that integrates nutrition, gut health, and systemic physiology. This guide explores the “Skyscraper” concept of nutritional psychiatry—building a robust foundation of health through micronutrients and the microbiome to support higher cognitive functions and emotional stability.
Part 1: The Micronutrient Encyclopedia for Mental Health
The brain is the most metabolically active organ in the body. While it represents only 2% of body weight, it consumes 20% of the body’s energy. This energy demand requires a constant supply of micronutrients to synthesize neurotransmitters, protect against oxidative stress, and maintain neuroplasticity.
Below is a comprehensive breakdown of essential nutrients and their specific roles in psychiatric health.
Essential Vitamins
The B-Complex: The Energy & Methylation Engines
B-vitamins are critical for the Methylation Cycle, a biochemical process that regulates neurotransmitters and DNA repair. Breaks in this cycle can lead to treatment-resistant depression.
Minerals and Trace Elements
Advanced Compounds and Adaptogens
- N-Acetyl-L-Cysteine (NAC): Modulates glutamate (the excitatory neurotransmitter). Shown to reduce intrusive thoughts in OCD and cravings in addiction.
- Acetyl-L-Carnitine: Increases mitochondrial energy output in the brain; acts as a rapid-onset antidepressant in some studies.
- Inositol: Involved in signal transduction; often used for panic disorder and PCOS-related mood issues.
- Shilajit: Rich in fulvic acid, supporting nutrient transport across the blood-brain barrier.
- Alpha-Lipoic Acid: A fatty acid that increases insulin sensitivity in the brain, combating “Type 3 Diabetes” (Alzheimer’s).
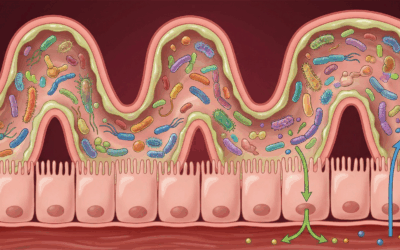
Part 2: The Gut-Brain Axis – The Second Brain
The gut-brain axis is a bidirectional communication highway linking the emotional and cognitive centers of the brain with peripheral intestinal functions. This connection explains why we feel “butterflies” when nervous and why digestive issues often accompany anxiety.
How the Gut Talks to the Brain
The communication occurs through three main channels:
- The Vagus Nerve: A physical nerve connecting the brainstem to the colon. 90% of fibers carry information from the gut to the brain.
- Neurotransmitters: Gut bacteria produce GABA, serotonin, dopamine, and short-chain fatty acids (SCFAs) like butyrate, which cross the blood-brain barrier to regulate inflammation and mood.
- The Immune System: A “leaky gut” (intestinal permeability) allows endotoxins into the bloodstream, triggering systemic inflammation (cytokines) that travels to the brain, causing neuroinflammation and depression.
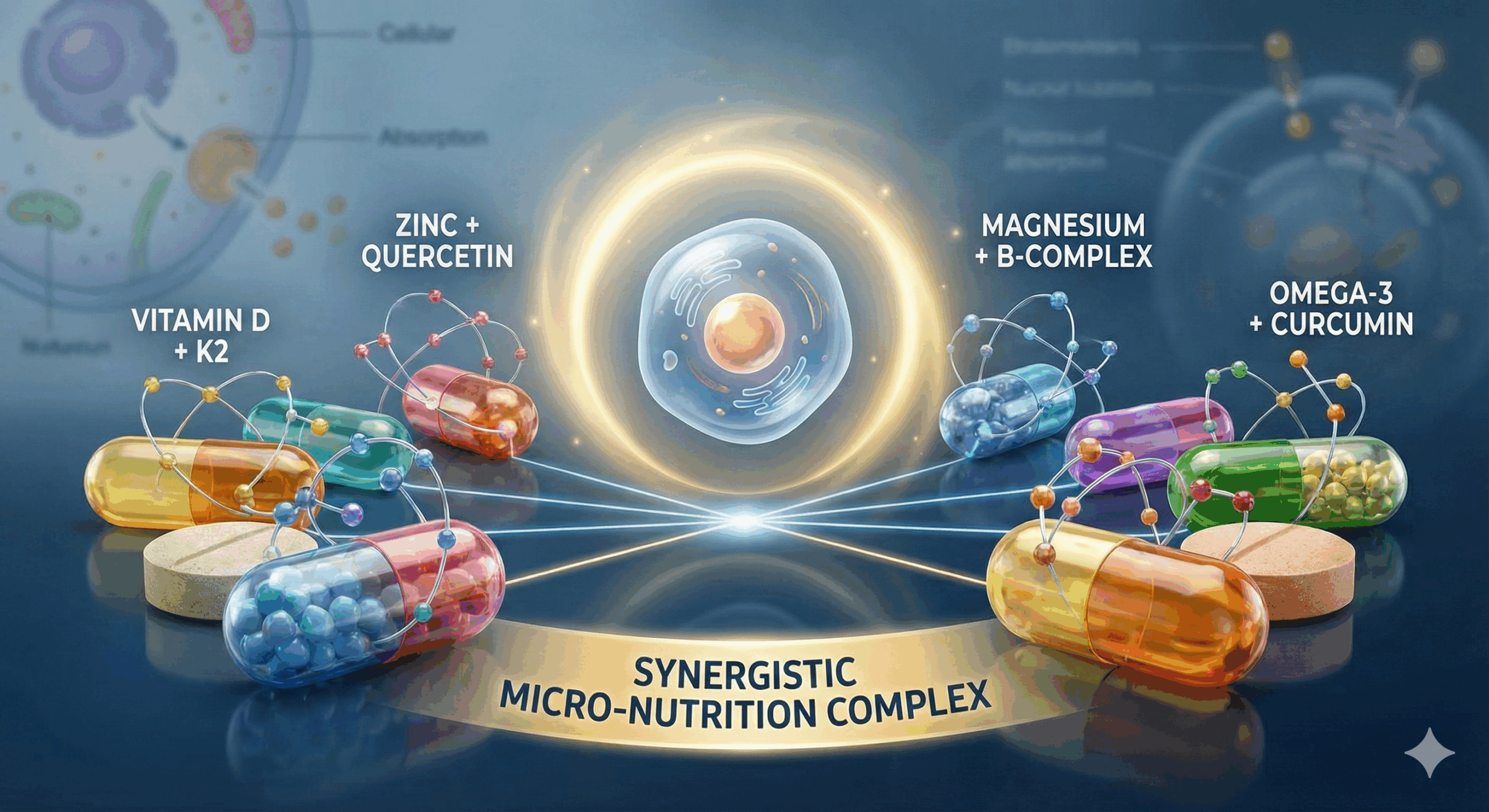
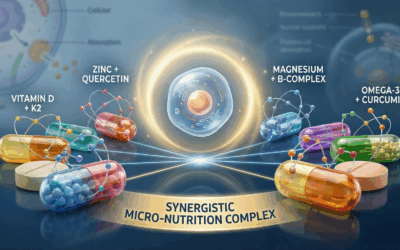
Synergistic Nutrition
Nutrients do not work in isolation. Synergistic nutrition recognizes that the bioavailability of one nutrient often depends on another.
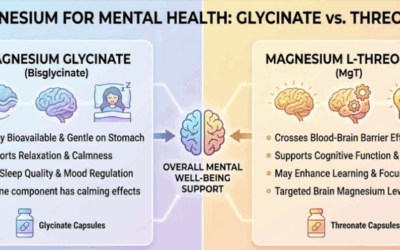
- Magnesium + Vitamin D: Magnesium is required to activate Vitamin D. Taking D without Magnesium can deplete magnesium stores.
- Iron + Vitamin C: Vitamin C significantly enhances the absorption of non-heme iron.
- Zinc + B6: Both are required to synthesize serotonin from tryptophan.
Part 3: Nutritional Protocols for Specific Conditions
Note: These protocols should be discussed with a healthcare provider.
Depression
Inflammation and methylation defects are common drivers.
Key Nutrients: Omega-3s (EPA > DHA), Methylated B-Complex (Folate/B12), Vitamin D3, Zinc, Magnesium.
Dietary Focus: Mediterranean Diet (Anti-inflammatory).
Anxiety & Panic
Often linked to GABA dysfunction or glutamate excess.
Key Nutrients: Magnesium Glycinate, Inositol, L-Theanine, Probiotics (Psychobiotics like Lactobacillus rhamnosus).
Dietary Focus: Blood sugar stabilization (protein at every meal) to prevent cortisol spikes.
ADHD & Executive Function
Linked to dopamine regulation and frontal lobe perfusion.
Key Nutrients: Iron (ferritin levels must be checked), Zinc, Omega-3s (high DHA), Protein-rich breakfast.
Dietary Focus: Elimination of artificial dyes and excessive sugar.
Bipolar Disorder
Requires mitochondrial support and neuroprotection.
Key Nutrients: Lithium Orotate (low dose), NAC, Omega-3s, Choline.
Dietary Focus: Ketogenic metabolic therapy is currently being researched for mood stabilization.
Bibliography of Current Research
The following references link to the National Library of Medicine (PubMed) and academic databases for verification.
- Almeida, O. P., et al. (2015). B vitamins to enhance treatment response to antidepressants in middle-aged and older adults.
- Anglin, R. E., et al. (2013). Vitamin D deficiency and depression in adults: systematic review and meta-analysis.
- Berk, M., et al. (2007). Vitamin D deficiency may play a role in depression. Medical Hypotheses.
- Berk, M., et al. (2013). The promise of N-acetylcysteine in neuropsychiatry. Trends in Pharmacological Sciences.
- Bottiglieri, T. (2005). Homocysteine and folate metabolism in depression.
- Brody, S. (2002). High-dose ascorbic acid increases intercourse frequency and improves mood. Biological Psychiatry.
- Coppen, A., & Bolander-Gouaille, C. (2005). Treatment of depression: time to consider folic acid and vitamin B12.
- Eyles, D. W., et al. (2013). Vitamin D, effects on brain development and links between low levels and neuropsychiatric disease.
- Fava, M., & Mischoulon, D. (2009). Folate in depression: efficacy, safety, and clinical issues.
- Fernandes, B. S., et al. (2016). N-Acetylcysteine in depressive symptoms and functionality: a systematic review.
- Gilbody, S., et al. (2007). MTHFR genetic polymorphisms and psychiatric disorders: a HuGE review.
- Haskell, C. F., et al. (2010). Effects of a multi-vitamin/mineral supplement on cognitive function.
- Kaplan, B. J., et al. (2015). The emerging field of nutritional mental health: inflammation, microbiome, and mitochondrial function.
- Kennedy, D. O. (2016). B vitamins and the brain: mechanisms, dose and efficacy.
- Kidd, P. M. (2007). Omega-3 DHA and EPA for cognition, behavior, and mood: clinical findings.
- Lakhan, S. E., & Vieira, K. F. (2008). Nutritional therapies for mental disorders. Nutrition Journal.
- Marx, W., et al. (2017). Nutritional psychiatry: the present state of the evidence.
- Nowak, G., et al. (2005). Effect of zinc supplementation on antidepressant therapy in unipolar depression.
- Rao, T. S., et al. (2008). Understanding nutrition, depression and mental illnesses.
- Rucklidge, J. J., & Kaplan, B. J. (2013). Broad-spectrum micronutrient formulas for psychiatric symptoms.
- Sarris, J., et al. (2015). Nutritional medicine as mainstream in psychiatry. The Lancet Psychiatry.
- Stough, C., et al. (2011). The effect of 90 day administration of a high dose vitamin B-complex on work stress.
- Weston, P. (2020). Nutritional Psychiatry: The Gut-Brain Connection. Psychiatric Times.
Legal Disclaimer
The information provided in this article is for educational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Do not discontinue psychiatric medication without supervision.
Read More Depth Psychology & Integrative Health:
Taproot Therapy Collective Podcast
QEEG Brain Mapping
Somatic Experiencing









0 Comments