The Hidden Pattern in Healthcare Policy
For mental health practitioners, insurance policy changes often feel like unpredictable storms that disrupt practice operations, threaten revenue streams, and create administrative chaos. Yet beneath this apparent randomness lies a remarkably consistent pattern: what Medicaid does today, private insurance will likely do tomorrow. Understanding this cascade effect—from CMS (Centers for Medicare & Medicaid Services) to Federal BCBS to state-level plans—transforms reactive scrambling into proactive planning.
This essay explores how therapists can leverage Medicaid’s role as healthcare’s “policy laboratory” to predict insurance trends years in advance, allowing them to build practices that thrive amid constant change rather than merely survive it.
The Policy Cascade: Understanding the Flow of Change
The CMS Foundation
At the apex of healthcare policy sits CMS, the federal agency that oversees both Medicare and Medicaid. CMS functions as the primary innovation engine for American healthcare, testing new reimbursement models, coverage frameworks, and care delivery approaches through its massive programs. When CMS implements a change—whether it’s recognizing audio-only telehealth sessions or funding collaborative care models—it creates a template that reverberates throughout the entire healthcare system.
This influence stems from both practical and regulatory factors. Practically, CMS establishes billing codes, documentation standards, and coverage criteria that become the lingua franca of healthcare administration. Regulatory pressure, particularly around mental health parity enforcement, ensures that private insurers cannot stray too far from CMS standards without risking compliance violations.
The Federal BCBS Bridge
The Federal Employee Program (FEP) administered by Blue Cross Blue Shield serves as the critical bridge between government policy and commercial insurance. Covering approximately 5.5 million federal employees and their families, FEP operates with unique agility—more nimble than state Medicaid programs yet influential enough to set commercial precedents.
When FEP adopts a CMS innovation, it effectively translates government policy into commercial practice. This translation typically occurs within 6-12 months of major CMS changes, providing therapists with a clear signal of what’s coming to their state and regional markets.
State-Level Implementation
State BCBS plans and other commercial insurers represent the final stage of policy cascade. These organizations typically lag 12-18 months behind Federal BCBS, waiting to see utilization data, financial impacts, and provider feedback before implementing changes. This delay, while frustrating for providers eager for expanded coverage, actually provides a valuable window for preparation.
Reading the Tea Leaves: Key Indicators to Monitor
Medicaid Pilot Programs
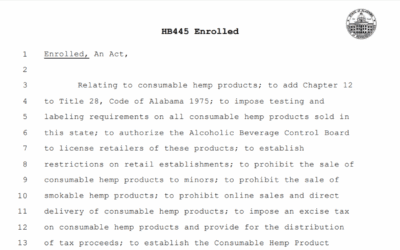
Medicaid pilot programs serve as healthcare’s research and development department. When CMS launches pilots for Certified Community Behavioral Health Clinics (CCBHCs), integrated care models, or novel reimbursement structures, savvy therapists should take note. These pilots, even when geographically limited, often preview nationwide policy shifts within 2-3 years.
Medicare Fee Schedule Updates
Annual Medicare physician fee schedule updates provide concrete signals about reimbursement trends. When Medicare adds new CPT codes for behavioral health services or adjusts relative value units (RVUs) for existing codes, private insurers invariably follow suit. The time lag varies, but the direction remains consistent.
Parity Enforcement Actions
Mental health parity enforcement actions by CMS create ripple effects throughout the insurance industry. When CMS flags specific documentation requirements, network adequacy standards, or reimbursement disparities, all insurers—public and private—scramble to align their policies. These enforcement actions often preview industry-wide compliance standards 12-24 months before full implementation.
Practical Strategies for Proactive Practice Management
Building Your Early Warning System
Creating an effective early warning system doesn’t require sophisticated technology—just consistent attention to the right sources. Therapists should:
- Subscribe to CMS bulletins: The Medicare Learning Network and Medicaid.gov provide free email updates on policy changes.
- Monitor Federal BCBS communications: FEP provider bulletins often preview changes 6-12 months before state implementation.
- Join professional associations: Organizations like the American Psychological Association and National Association of Social Workers maintain policy tracking teams that distill complex changes into practitioner-friendly summaries.
- Engage with billing services: Professional billing companies often spot trends across multiple practices and insurers, providing valuable pattern recognition.
Strategic Practice Positioning
Understanding the policy cascade enables strategic positioning that transforms challenges into opportunities:
Early Technology Adoption: When Medicaid pilots telehealth expansions, forward-thinking practices should invest in HIPAA-compliant platforms and train staff on virtual care delivery. By the time commercial insurers adopt these changes, early adopters have refined their processes and captured market share.
Documentation Systems: As CMS tightens documentation requirements for medical necessity or treatment planning, practices that proactively upgrade their clinical documentation systems avoid the last-minute scramble that catches their competitors off-guard.
Service Line Development: Watching Medicaid coverage expansions reveals emerging service opportunities. When CMS begins covering intensive outpatient programs (IOPs) or specific evidence-based treatments, practices can develop these capabilities before commercial reimbursement arrives.
Financial Sustainability Through Diversification
The policy cascade model argues strongly for practice diversification. Relying heavily on any single insurer or service line creates vulnerability to policy shifts. Instead, sustainable practices maintain:
- Payer diversity: Balancing commercial insurance, self-pay, and government programs
- Service diversity: Offering various levels of care and treatment modalities
- Revenue stream diversity: Combining traditional therapy with groups, assessments, and consultation
This diversification provides buffers against policy changes while positioning practices to capitalize on new opportunities as they emerge.
Case Studies: Learning from Recent History
The Telehealth Revolution
The COVID-19 pandemic accelerated a policy cascade that might have taken a decade under normal circumstances. CMS emergency waivers in March 2020 allowed audio-only therapy sessions and relaxed geographic restrictions. Federal BCBS followed within weeks, and by summer 2020, most state plans had adopted similar policies.
Practices that recognized this wasn’t merely a temporary emergency measure—but rather an acceleration of existing telehealth trends—invested in permanent virtual care infrastructure. When some insurers attempted to roll back telehealth coverage in 2022-2023, these practices successfully advocated for continued coverage, armed with utilization data and patient satisfaction metrics.
Collaborative Care Model Adoption
The CMS collaborative care model (CoCM) demonstration projects of 2017-2019 preview an ongoing transformation in behavioral health delivery. Early Medicaid pilots showed improved outcomes and cost-effectiveness for integrated behavioral health in primary care settings. Federal BCBS began covering CoCM codes in 2021, and state plans are now following suit.
Therapists who tracked these pilots recognized an opportunity to partner with primary care practices, positioning themselves as behavioral health consultants rather than traditional fee-for-service providers. These early movers now enjoy stable referral streams and enhanced reimbursement rates.
Building Your Sustainable Practice: A Five-Year Framework
Year 1: Foundation Building
- Establish monitoring systems for CMS, Federal BCBS, and state insurer communications
- Assess current practice vulnerabilities to likely policy changes
- Begin diversification planning
Year 2: Early Adoption
- Pilot new service lines based on Medicaid demonstrations
- Invest in technology and training for emerging care models
- Build relationships with other providers for potential partnerships
Year 3: Refinement
- Analyze early adoption results and refine processes
- Expand successful pilots as Federal BCBS adoption begins
- Develop outcome metrics to support future advocacy
Year 4: Market Leadership
- Position practice as expert in emerging care models
- Train other providers, generating additional revenue streams
- Advocate with state insurers for appropriate reimbursement
Year 5: Sustainable Operations
- Fully diversified practice with multiple revenue streams
- Established reputation for innovation and quality
- Prepared for next wave of policy changes
The Policy Implications: Aligning Stakeholder Interests
This predictable cascade reveals a profound truth often overlooked in healthcare policy debates: what benefits Medicaid ultimately benefits BCBS providers and patients. When CMS tests innovations through Medicaid—whether expanded telehealth access, integrated care models, or streamlined documentation—these changes eventually improve care delivery across all insurance types. This alignment suggests we should reconsider how we approach healthcare policy.
Rather than viewing Medicaid as a separate, budget-constrained program for low-income populations, policymakers should recognize it as the testing ground for improvements that will enhance healthcare for all Americans. Investments in Medicaid innovation aren’t just social safety net expenses—they’re research and development for the entire healthcare system. When Medicaid pilots succeed, they create templates for better care delivery that benefit patients with commercial insurance months or years later.
This perspective shift has practical implications for advocacy. Therapists and professional associations should support robust Medicaid funding and innovation not just for altruistic reasons, but because today’s Medicaid pilot is tomorrow’s BCBS standard benefit. Supporting Medicaid expansion and enhancement is, in a very real sense, investing in the future of private practice sustainability.
Conclusion: From Reactive to Proactive
The cascade from Medicaid to Federal BCBS to state insurers isn’t just a pattern—it’s a roadmap for practice sustainability. By monitoring CMS initiatives, therapists gain 2-3 years of preparation time for major industry shifts. This lead time transforms insurance changes from practice-threatening disruptions into strategic opportunities.
The most successful mental health practices of the next decade won’t be those that resist change or scramble to catch up. They’ll be the ones that watch Medicaid carefully, prepare thoughtfully, and position themselves at the forefront of each new wave. Understanding that Medicaid improvements ultimately benefit all providers and patients should inspire greater engagement with policy development at all levels.
In an industry where change is the only constant, the ability to see around corners isn’t just valuable—it’s essential for survival and success. For therapists willing to invest time in understanding and tracking the policy cascade, Medicaid truly becomes a crystal ball, revealing not just what’s possible in behavioral healthcare, but what’s inevitable. The only question remaining is whether you’ll be ready when the future arrives at your doorstep—and whether you’ll advocate for the Medicaid innovations that will shape your practice’s future.















0 Comments