Therapists across all modalities have observed a puzzling phenomenon that challenges our understanding of therapeutic progress: given similar presentations, symptom severity, and treatment approaches, some clients demonstrate remarkable improvement while others remain stuck or progress marginally. This differential response to therapy cannot be fully explained by diagnostic categories, therapeutic alliance quality, or even treatment compliance. Instead, researchers are increasingly recognizing resilience as a distinct neurobiological and psychological phenomenon that fundamentally influences therapeutic outcomes.
Resilience represents far more than simple “bouncing back” from adversity. It encompasses a complex interplay of neurobiological systems, epigenetic factors, developmental experiences, and behavioral patterns that create what researchers now understand as a phenotype, a observable set of characteristics arising from the interaction between genes and environment. When therapists describe certain clients as having “something different” about them that enables progress, they’re often observing the manifestations of resilience without necessarily recognizing its biological underpinnings.
The clinical implications are profound. Two clients with identical trauma histories and PTSD diagnoses might respond entirely differently to evidence-based treatments, not because of therapeutic factors but because of fundamental differences in their resilience architecture. Understanding these mechanisms transforms how we conceptualize treatment resistance, therapeutic progress, and the very nature of psychological healing.
The Neurobiological Architecture of Resilience
At the cellular level, resilience begins with the stress response system, particularly the hypothalamic-pituitary-adrenal (HPA) axis. Research by McEwen and colleagues at Rockefeller University has demonstrated that resilient individuals show distinct patterns of cortisol release and recovery. While all humans release cortisol in response to stressors, resilient individuals demonstrate what researchers term “appropriate responsivity”: their cortisol levels spike appropriately during stress but return to baseline more quickly. This rapid recovery prevents the toxic effects of chronic cortisol exposure on hippocampal neurons, preserving memory function and emotional regulation capacity.
Neuroimaging studies have revealed structural and functional brain differences associated with resilience. The prefrontal cortex, particularly the anterior cingulate cortex (ACC) and dorsolateral prefrontal cortex (dlPFC), shows increased gray matter density and activation in resilient individuals. Research published in Biological Psychiatry using fMRI technology found that resilient individuals demonstrate stronger connectivity between the prefrontal cortex and amygdala, allowing for better top-down regulation of fear responses. This enhanced connectivity appears to be both a cause and consequence of resilience, creating a positive feedback loop where successful stress management strengthens these neural pathways.
The hippocampus, crucial for memory consolidation and stress regulation, shows remarkable differences in resilient individuals. Studies of adult neurogenesis, the birth of new neurons in the adult brain, reveal that resilient individuals maintain higher rates of hippocampal neurogenesis even under stress. Brain-derived neurotrophic factor (BDNF), often called “Miracle Gro for the brain,” is produced at higher levels in resilient individuals. Research from Yale University found that BDNF gene polymorphisms significantly predict resilience to stress-related psychopathology, with certain variants conferring up to 40% reduction in PTSD risk following trauma exposure.
Neurotransmitter systems also display distinct patterns in resilient individuals. The serotonergic system, targeted by SSRI antidepressants, shows more efficient synthesis and receptor sensitivity in resilient populations. Perhaps more intriguingly, research on neuropeptide Y (NPY), a neurotransmitter involved in anxiety regulation, reveals that Special Forces soldiers with high NPY levels show remarkable stress resilience compared to regular troops. This finding has led to investigations into NPY as both a biomarker for resilience and a potential therapeutic target.
The dopaminergic reward system functions differently in resilient individuals, maintaining what researchers call “reward responsiveness” even under chronic stress. While depression typically involves anhedonia linked to dopamine dysfunction, resilient individuals preserve their ability to experience pleasure and motivation despite adversity. Neuroimaging studies show maintained ventral striatum activation to rewards in resilient individuals exposed to early life stress, whereas non-resilient individuals show blunted reward responses.
Epigenetic Mechanisms and Intergenerational Transmission
The field of epigenetics has revolutionized our understanding of resilience by revealing how environmental experiences alter gene expression without changing DNA sequences. The landmark studies of Michael Meaney at McGill University demonstrated that maternal behavior in rats literally reprograms stress response genes in offspring through methylation changes. High-licking and grooming mothers produce pups with enhanced glucocorticoid receptor expression in the hippocampus, creating lifelong stress resilience. Human studies have found parallel effects, with sensitive early caregiving associated with epigenetic changes that promote resilience.
The glucocorticoid receptor (GR) gene, NR3C1, has emerged as a critical site of epigenetic modification influencing resilience. Research published in Nature Neuroscience found that childhood abuse leads to hypermethylation of the GR gene promoter, reducing receptor expression and creating vulnerability to psychopathology. However, individuals with resilient outcomes despite childhood abuse show different methylation patterns, suggesting that other factors can modify or compensate for adverse epigenetic programming.
FKBP5, a gene regulating glucocorticoid receptor sensitivity, demonstrates how genetic variants interact with environmental stress to influence resilience. Certain FKBP5 polymorphisms combined with childhood trauma create epigenetic changes that persist into adulthood, affecting stress hormone regulation. However, research from the Max Planck Institute of Psychiatry found that these same “risk” variants can confer advantage in supportive environments, illustrating the complex, context-dependent nature of genetic contributions to resilience.
Telomeres, protective caps on chromosomes, provide a biological marker of stress exposure and resilience. While chronic stress typically accelerates telomere shortening, associated with cellular aging and disease vulnerability, resilient individuals maintain longer telomeres despite stress exposure. Elizabeth Blackburn’s Nobel Prize-winning research revealed that telomerase, the enzyme that rebuilds telomeres, shows higher activity in individuals practicing stress-reduction techniques, suggesting resilience can be cultivated at the cellular level.
Intergenerational transmission of resilience occurs through both epigenetic inheritance and behavioral transmission. Studies of Holocaust survivors and their descendants reveal complex patterns where trauma-related epigenetic changes are passed to offspring, but resilience factors can also be transmitted. Research from Mount Sinai found that while children of Holocaust survivors show epigenetic changes in stress response genes, those whose parents developed post-traumatic growth show different patterns suggesting inherited resilience capacity.
Developmental Factors and Critical Periods
The development of resilience follows specific temporal patterns, with critical periods where certain capacities must develop for optimal stress resistance. The first three years of life represent a crucial window for establishing stress response system regulation. During this period, the developing brain is extraordinarily plastic, with synapse formation occurring at rates never again matched. Secure attachment during this period creates what researchers term “neurobiological expectation of safety,” fundamentally shaping how the nervous system responds to future stressors.
The concept of “biological embedding” explains how early experiences become literally incorporated into developing biological systems. Research from the Center on the Developing Child at Harvard shows that serve-and-return interactions between infants and caregivers shape the architecture of the developing brain. These reciprocal interactions tune the stress response system, with consistent, sensitive caregiving creating more adaptive stress response patterns that persist throughout life.
Adolescence represents another critical period for resilience development, particularly for prefrontal cortex maturation and integration with limbic structures. The teenage brain undergoes extensive remodeling, with synaptic pruning eliminating unused connections while myelination increases processing speed in frequently used circuits. Research published in Developmental Science found that adolescents who successfully navigate moderate stressors during this period show enhanced resilience in adulthood, supporting the concept of “stress inoculation.”
The timing of adverse experiences profoundly influences their impact on resilience. Early life stress during critical periods can derail normal development, but the concept of “differential susceptibility” suggests that the same plasticity that creates vulnerability also enables remarkable adaptation given appropriate intervention. Studies of Romanian orphans adopted into nurturing families demonstrate that while early severe deprivation causes lasting effects, children adopted before age two show remarkable recovery, highlighting windows of opportunity for resilience building.
Cognitive development interacts with resilience in complex ways. The development of executive functions, particularly cognitive flexibility and working memory, provides tools for emotional regulation and stress management. Research from the University of Minnesota’s longitudinal studies found that children who develop strong executive functions by age five show better stress resilience throughout childhood and adolescence, even when facing adversity. These cognitive skills appear to buffer against stress by enabling better problem-solving and emotional regulation strategies.
The Immune System and Inflammatory Processes
The relationship between resilience and immune function has emerged as a crucial area of research, with inflammation increasingly recognized as a common pathway linking stress to both physical and mental illness. Resilient individuals show distinct inflammatory profiles, with lower baseline levels of pro-inflammatory cytokines like interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α). Research from UCLA found that people with high psychological resilience show reduced inflammatory responses to laboratory stressors, with their immune systems mounting appropriate but not excessive responses.
The concept of “inflammatory resilience” describes the ability to maintain immune homeostasis despite stress exposure. Studies of caregivers for family members with dementia, a population under chronic stress, reveal that resilient caregivers maintain healthier inflammatory profiles despite their challenging circumstances. This protection appears mediated by both behavioral factors like maintained social connections and biological factors like preserved vagal tone.
The gut-brain axis represents another frontier in resilience research. The microbiome, consisting of trillions of bacteria in the digestive system, profoundly influences brain function through production of neurotransmitters, regulation of inflammation, and direct neural communication via the vagus nerve. Research published in Biological Psychiatry found that resilient individuals harbor different bacterial compositions, with higher diversity and abundance of bacteria that produce short-chain fatty acids with anti-inflammatory properties.
Studies of germ-free mice, raised without any bacteria, demonstrate increased stress vulnerability and altered brain development, particularly in regions crucial for stress regulation. When colonized with bacteria from resilient versus vulnerable animals, these mice adopt the behavioral phenotype of their bacterial donors, suggesting the microbiome directly influences resilience. Human studies show parallel findings, with probiotic interventions improving stress resilience and emotional regulation.
The blood-brain barrier (BBB), traditionally viewed as a static anatomical structure, shows dynamic changes related to resilience. Chronic stress increases BBB permeability, allowing inflammatory molecules to enter the brain and trigger neuroinflammation. However, resilient individuals maintain BBB integrity even under stress. Research using advanced imaging techniques reveals that exercise, social support, and certain dietary factors that promote resilience also strengthen BBB function, suggesting multiple pathways to biological resilience.
Behavioral Patterns and Cognitive Frameworks
While biology provides the foundation, behavioral patterns and cognitive frameworks significantly influence resilience expression. Cognitive flexibility, the ability to adapt thinking patterns to changing circumstances, emerges consistently as a resilience marker. Research using neuropsychological testing shows that resilient individuals demonstrate superior performance on set-shifting tasks, reflecting their ability to abandon ineffective strategies and adopt new approaches. This flexibility extends beyond laboratory tasks to real-world problem-solving and emotional regulation.
The concept of “cognitive reappraisal,” reframing situations to alter their emotional impact, shows distinct neural signatures in resilient individuals. fMRI studies reveal that during reappraisal tasks, resilient individuals show stronger prefrontal activation and more effective down-regulation of amygdala activity. This enhanced neural efficiency during reappraisal correlates with better real-world stress management and reduced psychopathology risk.
Meaning-making represents a crucial cognitive process in resilience. Research on post-traumatic growth reveals that individuals who construct coherent narratives about their adversity, finding meaning or purpose in their struggles, show better psychological and physical health outcomes. This isn’t simply “positive thinking” but involves complex cognitive processing that integrates experiences into existing schemas while accommodating new information. Studies of written disclosure interventions demonstrate that the process of creating coherent narratives about stressful experiences produces measurable improvements in immune function and psychological wellbeing.
Active coping strategies distinguish resilient from vulnerable individuals. Rather than passive avoidance or rumination, resilient individuals engage in problem-focused coping when situations are controllable and emotion-focused coping when they’re not. This flexible coping repertoire appears linked to anterior cingulate cortex function, with this brain region essentially serving as a “conflict monitor” that guides strategy selection based on situational demands.
The phenomenon of “psychological flexibility,” central to Acceptance and Commitment Therapy, encompasses multiple resilience-promoting processes. This includes present-moment awareness, acceptance of difficult emotions, clarity about personal values, and committed action despite discomfort. Research shows that psychological flexibility mediates the relationship between adverse experiences and psychopathology, with flexible individuals showing better outcomes despite equivalent stress exposure.
Social Factors and Interpersonal Neurobiology
Human resilience cannot be understood outside the context of relationships. The field of interpersonal neurobiology reveals that our nervous systems are fundamentally designed for co-regulation with others. The polyvagal theory, developed by Stephen Porges, explains how our social engagement system, mediated by the ventral vagus nerve, provides a neural platform for resilience through connection with others.
Research on social baseline theory demonstrates that the presence of supportive others literally changes how the brain processes threats. fMRI studies show that holding a loved one’s hand during threat of electric shock reduces both subjective distress and neural activation in pain and threat-processing regions. This “load-sharing” effect appears stronger in individuals with secure attachment histories, suggesting early relationships shape lifelong capacity for co-regulation.
The quality of social relationships matters more than quantity for resilience. Research from the Harvard Study of Adult Development, spanning over 80 years, reveals that relationship quality predicts resilience to life stressors better than any other factor measured. At the biological level, supportive relationships buffer cortisol responses, reduce inflammation, and even influence gene expression. Studies show that perceived social support correlates with reduced inflammatory gene expression, mediated by reduced sympathetic nervous system activation.
Mirror neuron systems, neural networks that activate both when performing actions and observing others perform them, contribute to resilience through enabling empathy and social learning. Research reveals that individuals with more active mirror neuron systems show better social functioning and emotional resilience. These systems allow us to learn coping strategies through observation and internalize others’ calm states, essentially “borrowing” resilience from our social environment.
Cultural factors profoundly influence resilience expression and development. Collectivist cultures that emphasize interdependence show different resilience patterns than individualist cultures. Research comparing Japanese and American responses to stress found that Japanese individuals show greater resilience when using interdependent coping strategies, while Americans benefit more from independent strategies. This cultural shaping extends to neural level, with cultural background influencing brain activation patterns during stress and recovery.
The Role of Exercise and Physical Factors
Physical exercise emerges as one of the most powerful resilience-promoting interventions, with effects spanning from molecular to behavioral levels. Aerobic exercise stimulates production of BDNF, promoting neuroplasticity and protecting against stress-induced neural damage. Research from the Karolinska Institute found that exercise literally changes how muscles process kynurenine, a stress-induced metabolite linked to depression, preventing it from crossing the blood-brain barrier and affecting mood.
The concept of “exercise-induced resilience” encompasses multiple mechanisms. Regular physical activity enhances mitochondrial function, improving cellular energy production and stress resistance. It promotes adult neurogenesis in the hippocampus, with new neurons showing enhanced plasticity and stress resilience. Exercise also optimizes the HPA axis, creating more adaptive cortisol rhythms and faster recovery from stressors.
Resistance training shows unique resilience benefits beyond aerobic exercise. Studies of older adults found that strength training not only preserves muscle mass but enhances executive function and emotional regulation. The mechanism appears to involve myokines, muscle-derived factors that cross the blood-brain barrier and influence brain function. Irisin, a myokine increased by exercise, promotes BDNF expression and shows antidepressant effects in animal models.
Sleep represents another critical physical factor in resilience. During sleep, the glymphatic system clears metabolic waste from the brain, including proteins associated with neurodegeneration. REM sleep particularly contributes to emotional resilience by processing emotional memories and reducing their affective charge. Research shows that individuals with better sleep quality before trauma exposure show reduced PTSD risk, suggesting sleep builds prospective resilience.
Circadian rhythm regulation influences resilience through multiple pathways. The suprachiasmatic nucleus, our biological clock, coordinates numerous physiological processes relevant to stress response. Disrupted circadian rhythms, common in modern life, impair resilience by dysregulating cortisol rhythms, inflammatory processes, and neurotransmitter systems. Research on shift workers reveals increased vulnerability to stress-related disorders, while interventions that stabilize circadian rhythms enhance resilience.
Nutritional and Metabolic Factors
Emerging research reveals profound connections between nutrition, metabolism, and resilience. The brain’s high metabolic demands make it particularly vulnerable to nutritional insufficiencies that compromise stress resilience. Omega-3 fatty acids, particularly DHA and EPA, incorporate into neural membranes and influence neurotransmitter function, inflammation, and neuroplasticity. Randomized controlled trials show that omega-3 supplementation reduces cortisol responses to stress and improves emotional regulation.
The concept of “metabolic resilience” describes the body’s ability to maintain energy homeostasis under stress. Insulin sensitivity emerges as a crucial factor, with insulin resistance associated with increased vulnerability to stress-related disorders. Research reveals bidirectional relationships: stress promotes insulin resistance through cortisol-mediated mechanisms, while insulin resistance impairs brain function and stress regulation. Interventions improving metabolic health, such as intermittent fasting or ketogenic diets, show promise for enhancing psychological resilience.
Micronutrients play often-overlooked roles in resilience. Magnesium, involved in over 300 enzymatic reactions, modulates the stress response by regulating NMDA receptors and HPA axis function. Studies show that magnesium deficiency increases stress vulnerability, while supplementation reduces cortisol and improves stress resilience. Zinc, crucial for hippocampal function and neurogenesis, shows similar patterns, with deficiency associated with increased depression and anxiety risk.
The gut-brain axis’s nutritional dimensions extend beyond the microbiome to include intestinal permeability and nutrient absorption. Chronic stress increases intestinal permeability, allowing bacterial endotoxins to enter circulation and trigger inflammation. This “leaky gut” phenomenon creates a vicious cycle where stress impairs nutrient absorption, compromising the resources needed for stress resilience. Interventions targeting gut health, including prebiotics, probiotics, and dietary modifications, show promise for enhancing resilience.
B vitamins, particularly folate, B6, and B12, influence resilience through their roles in neurotransmitter synthesis and methylation processes. These vitamins are cofactors in producing serotonin, dopamine, and GABA, neurotransmitters crucial for mood regulation. They also participate in methylation reactions that regulate gene expression, including genes involved in stress response. Research shows that B vitamin supplementation can enhance antidepressant response and improve stress resilience, particularly in individuals with genetic variants affecting vitamin metabolism.
Mindfulness and Contemplative Practices
Mindfulness meditation has emerged from ancient contemplative traditions to become a scientifically validated resilience intervention. Neuroimaging studies reveal that mindfulness practice induces both structural and functional brain changes associated with enhanced resilience. Regular meditators show increased gray matter density in the hippocampus, crucial for stress regulation, and decreased amygdala volume, associated with reduced emotional reactivity.
The concept of “mindfulness-based resilience” involves multiple mechanisms. At the neural level, mindfulness strengthens prefrontal regulation of limbic structures, enhancing emotional regulation. It also alters default mode network activity, reducing rumination and self-referential processing associated with depression and anxiety. Research from Harvard Medical School found that eight weeks of mindfulness practice produces measurable changes in brain regions associated with learning, memory, emotional regulation, and perspective-taking.
Contemplative practices influence resilience at the molecular level. Research on experienced meditators reveals altered gene expression patterns, with downregulation of inflammatory pathways and upregulation of genes involved in cellular stress resistance. Studies of intensive meditation retreats show changes in telomerase activity, suggesting mindfulness might slow cellular aging. These molecular changes occur remarkably quickly, with some studies showing altered gene expression after single meditation sessions.
Different contemplative practices offer distinct resilience benefits. Loving-kindness meditation specifically enhances social connection and reduces implicit bias, strengthening social resources for resilience. Body scan practices improve interoception, the awareness of internal bodily signals crucial for emotional regulation. Movement-based practices like tai chi or qigong combine physical exercise benefits with mindfulness, showing particular efficacy for stress-related physical symptoms.
The therapeutic application of mindfulness for resilience extends beyond formal meditation. Mindfulness-Based Stress Reduction (MBSR) and Mindfulness-Based Cognitive Therapy (MBCT) integrate contemplative practices with psychoeducation and cognitive techniques. Meta-analyses show these interventions reduce relapse rates in recurrent depression, enhance emotional regulation, and improve stress resilience. The mechanisms appear to involve both direct effects on stress physiology and indirect effects through improved self-awareness and coping strategies.
Implications for Therapeutic Practice
Understanding resilience’s multifaceted nature transforms therapeutic approaches. Rather than focusing solely on symptom reduction, resilience-informed therapy aims to strengthen the biological and psychological systems that enable adaptation and growth. This might involve interventions targeting specific resilience mechanisms: exercise prescriptions to enhance neuroplasticity, sleep hygiene to optimize glymphatic clearance, or nutritional interventions to support neurotransmitter synthesis.
The timing of interventions matters given critical periods and neuroplasticity windows. Early intervention during developmental critical periods can prevent resilience deficits, while understanding adult neuroplasticity informs when and how to implement resilience-building interventions. For instance, the enhanced neuroplasticity following ketamine treatment might represent an optimal window for psychological interventions, combining biological and psychological approaches for synergistic effects.
Assessment of resilience factors should extend beyond psychological measures to include biological markers when possible. Heart rate variability, cortisol awakening response, inflammatory markers, and even genetic testing for resilience-relevant polymorphisms could inform personalized treatment planning. This precision medicine approach recognizes that different individuals might require different pathways to resilience based on their unique biological and psychological profiles.
The therapeutic relationship itself becomes a vehicle for resilience development through interpersonal neurobiology mechanisms. The therapist’s regulated nervous system provides co-regulation opportunities, while the therapeutic relationship offers a secure base for exploring new coping strategies. Understanding attachment neuroscience informs how to titrate interventions based on clients’ capacity for regulation and connection.
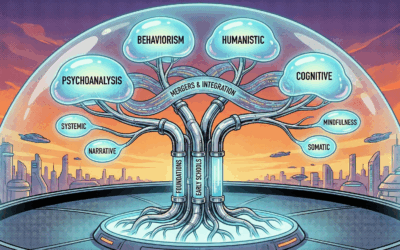
Integration of bottom-up and top-down approaches optimizes resilience building. Bottom-up interventions target the body and brainstem through approaches like somatic experiencing, EMDR, or vagus nerve stimulation. Top-down approaches engage prefrontal regions through cognitive restructuring, mindfulness, or meaning-making. Combining these approaches addresses resilience at multiple levels simultaneously.
Future Directions and Emerging Interventions
The future of resilience intervention lies in personalized, multimodal approaches informed by individual biological and psychological profiles. Pharmacological interventions targeting specific resilience mechanisms are under development, including NPY analogs for anxiety resilience, ketamine for rapid neuroplasticity enhancement, and even psychedelics for promoting psychological flexibility and post-traumatic growth.
Digital interventions offer scalable resilience building. Apps delivering ecological momentary interventions can provide real-time support during stress, while virtual reality enables controlled exposure to stressors for building stress inoculation. Biofeedback devices allow individuals to train stress response systems directly, making the invisible visible and controllable.
The concept of “preventive resilience” involves identifying at-risk individuals before stress exposure and providing targeted interventions. Genetic screening might identify individuals with resilience-compromising variants, enabling early intervention. Pre-deployment resilience training for military personnel and first responders demonstrates this approach’s potential, with studies showing reduced PTSD rates following trauma exposure.
Community-level interventions recognize resilience as not just individual but collective phenomenon. Programs building social capital, cultural connection, and community resources create environments that foster resilience. Research on community resilience following disasters reveals that communities with strong social networks and cultural practices show better recovery, suggesting resilience interventions should extend beyond individual therapy to community development.
Resilience represents a complex phenotype emerging from the dynamic interaction of neurobiological systems, developmental experiences, behavioral patterns, and social contexts. The therapist observing that ineffable quality enabling some clients to thrive is witnessing the culmination of countless biological and psychological processes operating from molecular to social levels. Understanding these mechanisms transforms resilience from mysterious clinical observation to targetable therapeutic outcome.
This multisystem understanding explains why simplistic interventions often fail and why some individuals seem naturally resilient while others struggle despite their best efforts. It’s not about strength of character or willpower but about the complex interplay of genetics, epigenetics, neurodevelopment, and experience creating different capacities for adaptation. This knowledge should inspire both humility about resilience’s complexity and optimism about intervention possibilities.
As we continue uncovering resilience mechanisms, the therapeutic landscape will increasingly shift from treating pathology to building capacity. This doesn’t minimize the reality of mental illness or the need for symptom-focused treatment but recognizes that sustainable healing involves strengthening the systems that enable ongoing adaptation and growth. The future of mental health treatment lies not just in eliminating dysfunction but in cultivating the remarkable human capacity for resilience that allows not just survival but transformation through adversity.













0 Comments