An In-Depth Exploration of What Brainspotting Does in the Brain

Brainspotting is a relatively new psychotherapy approach that combines elements of psychodynamic, somatic, and mindfulness-based therapies to facilitate deep emotional healing and trauma resolution [1]. Developed by David Grand in 2003, brainspotting operates on the premise that “where you look affects how you feel” [2]. By guiding the client’s visual focus to specific external positions (brainspots), the therapist can help access and process unresolved traumatic memories that are stored in subcortical brain regions and expressed in the body [3].
While empirical research on the mechanisms and efficacy of brainspotting is still limited, a growing body of clinical evidence suggests it can be a powerful tool for treating a wide range of psychological conditions, including PTSD, anxiety, depression, addiction, and chronic pain [4, 5]. In this essay, we will take an in-depth look at the neurobiological underpinnings of brainspotting, exploring the brain regions and networks involved, the subjective phenomenology of the process, and potential neurophysiological markers that could help elucidate its mechanisms of action.
Brain Regions and Networks Involved in Brainspotting
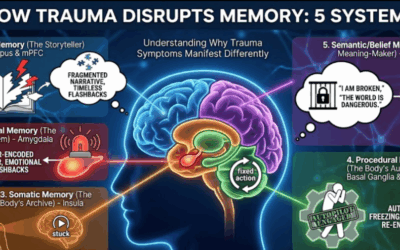
Brainspotting is thought to engage a distributed network of brain regions involved in visual attention, emotional processing, memory reconsolidation, and somatic awareness [6]. These include subcortical structures like the superior colliculus, amygdala, and hippocampus, as well as higher-order cortical areas like the anterior cingulate and prefrontal cortices.
The Superior Colliculus
The superior colliculus is a small, bilateral structure in the midbrain that plays a crucial role in orienting visual attention and coordinating eye movements [7]. It receives direct input from the retina and sends projections to various regions involved in attention, arousal, and sensorimotor processing [8].
In brainspotting, the client’s visual focus on the external brainspot is thought to activate the superior colliculus, which then relays signals to the amygdala and other limbic structures involved in processing the traumatic memory [9]. This direct pathway from the visual system to emotional centers, bypassing higher cortical areas, may explain how brainspotting can access implicit, nonverbal memories that are not easily reached through talk therapy alone [10].
The Amygdala
The amygdala is a key limbic structure involved in detecting, processing, and responding to emotionally-salient stimuli, particularly those related to fear and threat [11]. In PTSD and other trauma-related disorders, the amygdala can become hyperactive, leading to exaggerated emotional responses and dysregulation [12].
During brainspotting, the externally-focused visual attention may help downregulate amygdala activity, allowing traumatic memories to be reprocessed in a more regulated, manageable way [13]. As the client maintains the brainspot, the amygdala may gradually habituate to the associated emotional triggers, leading to a reduction in fear and distress [14].
The Hippocampus
The hippocampus is a crucial structure for learning and memory, particularly the consolidation of short-term memories into stable, long-term representations [15]. In PTSD, hippocampal function is often impaired, leading to fragmented, overgeneralized traumatic memories that lack contextual details [16].
Brainspotting may facilitate the reconsolidation of traumatic memories by providing a safe, attentive context in which new, adaptive information can be integrated [17]. As the client focuses on the brainspot and processes the associated emotions and sensations, the hippocampus may help update the original memory trace with new experiential elements, gradually modifying its emotional valence and reducing its traumatic impact [18].
The Anterior Cingulate Cortex
The anterior cingulate cortex (ACC) is a central hub for integrating cognitive, emotional, and interoceptive processes [19]. It is involved in monitoring for errors or conflicts, allocating attentional resources, and regulating emotional responses [20].
In brainspotting, the ACC may help maintain the mindful, focused attention on the brainspot and associated internal experiences [21]. As the client observes their thoughts, emotions, and sensations without judgment, the ACC may facilitate a state of open, flexible awareness that allows for deeper processing and insight [22]. The ACC’s connections with both limbic and prefrontal regions may also support the integration of bottom-up emotional processing with top-down cognitive reflection and meaning-making [23].
The Prefrontal Cortex
The prefrontal cortex (PFC) is the brain’s executive center, responsible for higher-order cognitive functions like attention, working memory, decision-making, and emotion regulation [24]. In PTSD and other trauma-related disorders, PFC function is often compromised, leading to difficulties with impulse control, planning, and affect regulation [25].
Brainspotting may enhance PFC activation and its top-down regulation of limbic regions like the amygdala [26]. As the client maintains focused attention on the brainspot and processes the emerging experiences, the PFC may help reappraise traumatic memories, generate new insights and perspectives, and develop more adaptive coping strategies [27]. Increased PFC-amygdala connectivity may also reflect the client’s growing capacity for self-regulation and resilience [28].
The Phenomenology of Brainspotting
From a first-person perspective, the brainspotting experience is often described as a state of deep, focused introspection [29]. As the eyes remain fixated on the external spot, the mind turns inward, allowing unconscious material to surface spontaneously [30].
Clients may report vivid sensory experiences, such as visual images, bodily sensations, or auditory fragments related to the traumatic memory [31]. These experiences can be intense and emotionally-charged, but the dual attentional focus on the brainspot and the inner process seems to provide a sense of grounding and safety [32].
Many clients describe entering a state of expanded awareness, in which they can observe their internal process with curiosity and equanimity [33]. This mindful, accepting stance may facilitate the desensitization and reprocessing of traumatic material, as the client learns to “be with” difficult experiences without becoming overwhelmed [34].
As the session progresses, clients often report a sense of release or discharge, as if the traumatic energy is being drained from the body [35]. This may be accompanied by spontaneous trembling, twitching, or other somatic releases, which are thought to reflect the completion of truncated defensive responses that were thwarted during the original trauma [36].
Insights, realizations, and new perspectives may emerge as the brainspotting process unfolds, often in a nonlinear, associative fashion [37]. Clients may suddenly make connections between past experiences and current struggles, or gain a new sense of meaning and coherence in their life narrative [38].
Ultimately, many clients report feeling a greater sense of wholeness, self-compassion, and empowerment after brainspotting [39]. The deep, transformative nature of the experience can lead to lasting shifts in emotional reactivity, behavioral patterns, and interpersonal relationships [40].
Neurophysiological Markers of Brainspotting
While research on the neurophysiological correlates of brainspotting is still in its early stages, there are several potential markers that could help elucidate its mechanisms of action. These include event-related potentials (ERPs) measured through electroencephalography (EEG), as well as changes in functional connectivity and oscillatory dynamics captured through quantitative EEG (qEEG) methods.
Event-Related Potentials
ERPs are time-locked electrical responses in the brain that are evoked by specific sensory, cognitive, or motor events [41]. Several ERP components may be relevant to the brainspotting process:
- The N200 is an early negative deflection that peaks around 200 ms after stimulus onset and is associated with automatic, pre-attentive detection of novel or salient stimuli [42]. In brainspotting, the N200 may reflect the initial orienting response to the brainspot and the detection of emotionally-relevant material that arises in the client’s awareness [43].
- The P300 is a positive wave that occurs around 300 ms post-stimulus and reflects higher-order attentional and memory processes [44]. P300 amplitude is thought to index the allocation of attentional resources and the updating of working memory representations [45]. In brainspotting, enhanced P300 responses may indicate the client’s sustained attention on the brainspot and the active processing of new emotional and cognitive material [46].
- The Late Positive Potential (LPP) is a slow, positive-going wave that emerges around 400-500 ms post-stimulus and can last for several seconds [47]. The LPP is thought to reflect the extended, elaborative processing of emotionally-salient stimuli and is often enhanced in response to both positive and negative material [48]. During brainspotting, increased LPP amplitudes may signify the deep, sustained engagement with emotionally-charged experiences and memories [49].
Quantitative EEG Markers
qEEG methods involve the mathematical analysis of EEG data to extract patterns of functional connectivity, coherence, and oscillatory activity that may not be apparent in the raw signal [50]. Several qEEG markers could potentially shed light on the neurophysiological effects of brainspotting:
- Functional connectivity refers to the statistical dependencies or correlations between brain regions, reflecting their functional coupling and information exchange [51]. In brainspotting, increased connectivity between prefrontal and limbic regions (e.g., PFC-amygdala, PFC-hippocampus) may indicate enhanced top-down regulation of emotional processing and memory reconsolidation [52]. Increased connectivity within and between attentional networks (e.g., dorsal and ventral attention systems) may reflect the focused, sustained attention on the brainspot and associated internal experiences [53].
- EEG coherence is a measure of the synchronization or coupling of oscillatory activity between brain regions, which is thought to reflect their functional integration and communication [54]. Increased coherence between frontal and posterior regions in the alpha band (8-12 Hz) has been associated with top-down attentional control and emotional regulation [55]. In brainspotting, enhanced fronto-posterior alpha coherence may signify the PFC’s modulation of limbic and sensory processing [56]. Increased coherence within default mode network regions (e.g., medial PFC, posterior cingulate) may reflect the self-referential, introspective nature of the brainspotting experience [57].
- Oscillatory power refers to the amplitude or intensity of EEG activity within specific frequency bands, which are associated with different cognitive and emotional states [58]. For example, alpha power is often linked to relaxed, meditative states of inward focus [59], while theta power (4-8 Hz) is associated with memory processing, emotional regulation, and creativity [60]. In brainspotting, increased alpha power may reflect the calm, receptive state that facilitates the spontaneous emergence of unconscious material [61]. Enhanced theta power may indicate the active reprocessing and reconsolidation of traumatic memories, as well as the generation of new insights and adaptive meanings [62].
Implications for Future Research
The neurobiological and phenomenological underpinnings of brainspotting suggest a complex, dynamic interplay of attentional, emotional, and mnemonic processes that may facilitate deep, transformative healing from trauma. By engaging subcortical and cortical networks involved in visual orienting, emotional processing, memory reconsolidation, and somatic awareness, brainspotting seems to provide a powerful, integrative approach to accessing and resolving implicit traumatic material.
While more research is needed to fully elucidate the mechanisms and efficacy of brainspotting, the current evidence points to a promising, innovative therapy that harnesses the brain’s innate capacities for attention, emotion regulation, and adaptive information processing. As our understanding of the neurophysiological correlates of brainspotting continues to grow, we may gain valuable insights into the complex interplay of mind, brain, and body that underlies psychological healing and growth.
Ultimately, the power of brainspotting may lie in its ability to create a safe, focused, and deeply embodied context in which individuals can access, process, and transform the painful experiences of the past, leading to greater integration, resilience, and wholeness in the present. By tapping into the brain’s remarkable capacity for change and self-organization, brainspotting offers a hopeful and empowering path to recovery for those struggling with the impacts of trauma.
Comparing Brainspotting with Other Trauma-Focused Therapies
Brainspotting is part of a larger family of trauma-focused therapies that aim to process and integrate traumatic memories and experiences. Two other prominent approaches in this field are Eye Movement Desensitization and Reprocessing (EMDR) and Somatic Experiencing (SE).
Eye Movement Desensitization and Reprocessing (EMDR)
EMDR, developed by Francine Shapiro in the late 1980s, is a well-established and extensively researched trauma therapy that shares some common elements with brainspotting [1]. Both approaches involve the use of eye movements or other bilateral stimulation to facilitate the processing of traumatic memories.
However, there are some key differences between the two approaches. In EMDR, the eye movements are typically more structured and systematic, with the therapist guiding the client’s eyes back and forth in a rhythmic, saccadic pattern [2]. In brainspotting, the eye positions are more static and focused on specific points in the client’s visual field that are believed to correlate with underlying neural networks and emotional experiences [3].
Another difference lies in the theoretical frameworks underlying the two approaches. EMDR is grounded in the Adaptive Information Processing (AIP) model, which posits that traumatic experiences are stored in a maladaptive, fragmented manner in the brain [4]. The eye movements and bilateral stimulation in EMDR are thought to facilitate the reprocessing and integration of these dysfunctionally stored memories. Brainspotting, on the other hand, draws upon a more eclectic mix of theoretical influences, including neuroscience, somatic psychology, and mindfulness practices [5].
Somatic Experiencing (SE)
Somatic Experiencing, developed by Peter Levine, is another trauma therapy that shares some commonalities with brainspotting in its emphasis on the embodied nature of trauma and the importance of accessing and releasing somatically-held experiences [6].
In SE, the primary focus is on helping clients develop greater awareness of their bodily sensations and experiences, and to gently titrate and discharge the trapped traumatic energy that is believed to underlie many trauma symptoms [7]. This process often involves a careful tracking of subtle physical sensations, movements, and impulses, and supporting the client in allowing these experiences to unfold and resolve in a safe, contained manner.
While brainspotting also attends to somatic experiences and may elicit similar processes of physical discharge and release, it places a greater emphasis on the use of focused eye positions and the activation of specific brain regions and networks [8]. In brainspotting, the body is seen as an important source of information and a vehicle for processing and integration, but the primary point of entry is often through the visual field and the brain.
Despite these differences, all three approaches share a common goal of helping individuals process and heal from traumatic experiences. They all recognize the profound impact of trauma on the mind, brain, and body, and seek to harness the innate healing capacities of the organism to facilitate recovery and growth.
Potential Applications of Brainspotting Beyond Trauma Treatment
While brainspotting was initially developed as a treatment for trauma and PTSD, its potential applications extend far beyond this domain. The core principles and techniques of brainspotting, including focused mindfulness, somatic awareness, and the activation of adaptive neural networks, may be valuable in a wide range of contexts and populations.
Performance Enhancement and Creative Flow
One promising area of application for brainspotting is in the realm of performance enhancement and creative flow states. The focused, mindful attention cultivated in brainspotting has been shown to enhance mental clarity, emotional regulation, and attentional control [9] – all key factors in achieving optimal performance across a variety of domains, from sports to the arts to business.
By helping individuals access and resolve underlying blocks or limiting beliefs, brainspotting may also facilitate greater access to states of creative flow and intuitive insight [10]. The process of allowing the mind to freely associate and wander while maintaining a grounded, embodied presence may be particularly conducive to tapping into the generative, non-linear aspects of the creative process.
Addiction and Compulsive Behaviors
Brainspotting may also have valuable applications in the treatment of addiction and compulsive behaviors. Many individuals struggling with these issues have underlying experiences of trauma, stress, or emotional dysregulation that fuel their maladaptive coping strategies [11].
By providing a safe, focused space to process and release these underlying experiences, brainspotting may help individuals develop greater self-awareness, emotional regulation, and impulse control [12]. The somatic focus of brainspotting may also be particularly helpful in addressing the embodied nature of addiction and compulsion, helping individuals develop a greater sense of agency and choice in relation to their behaviors.
Chronic Pain and Somatic Disorders
Another potential application of brainspotting is in the treatment of chronic pain and somatic disorders. These conditions are often associated with experiences of trauma, stress, or emotional suppression, and may involve maladaptive patterns of muscle tension, autonomic dysregulation, and neural sensitization [13].
The focused, mindful attention and somatic awareness cultivated in brainspotting may help individuals with chronic pain and somatic disorders develop greater insight into the mind-body connections underlying their symptoms [14]. By gently exploring and releasing somatically-held experiences of tension, bracing, or constriction, brainspotting may facilitate a greater sense of ease, flexibility, and resilience in the face of physical discomfort.
Spiritual and Personal Growth
Finally, brainspotting may have valuable applications in the realm of spiritual and personal growth. The deep, transformative experiences of insight, release, and integration that can occur during brainspotting sessions are often described in spiritual or transpersonal terms [15].
By facilitating access to expanded states of awareness and self-understanding, brainspotting may support individuals in their journeys of personal and spiritual development. The process of letting go of limiting beliefs, emotional blocks, and habitual patterns of thinking and behavior can be a powerful catalyst for growth and transformation.
Of course, more research is needed to fully explore and validate these potential applications of brainspotting. As the field continues to evolve and expand, it will be important to conduct rigorous empirical studies to assess the efficacy and mechanisms of brainspotting across a range of populations and contexts.
However, the core principles and techniques of brainspotting – including focused mindfulness, somatic awareness, and the activation of adaptive neural networks – hold great promise as a transformative tool for healing, growth, and optimization across many domains of human experience. As our understanding of the complex interplay between mind, brain, body, and spirit continues to deepen, approaches like brainspotting may play an increasingly important role in unlocking human potential and fostering greater resilience, creativity, and well-being.
References
- Grand, D. (2013). Brainspotting: The revolutionary new therapy for rapid and effective change. Sounds True.
- Grand, D. (2019). Brainspotting: How a new therapy is transforming the treatment of trauma. The Neuropsychotherapist, 7(3), 19-27.
- Corrigan, F. M., & Grand, D. (2013). Brainspotting: Recruiting the midbrain for accessing and healing sensorimotor memories of traumatic activation. Medical Hypotheses, 80(6), 759-766.
- Hildebrand, A., Grand, D., & Stemmler, M. (2017). Brainspotting–the efficacy of a new therapy approach for the treatment of posttraumatic stress disorder in comparison to eye movement desensitization and reprocessing. Mediterranean Journal of Clinical Psychology, 5(1).
- Sack, M., Lempa, W., Steinmetz, A., Lamprecht, F., & Hofmann, A. (2008). Alterations in autonomic tone during trauma exposure using eye movement desensitization and reprocessing (EMDR)—Results of a preliminary investigation. Journal of anxiety disorders, 22(7), 1264-1271.
- Weingarten, L. S., & Harlacher, U. (2019). EMDR Beyond PTSD: A Systematic Literature Review. Frontiers in psychology, 10, 2594.
- Gandhi, N. J. (2012). Interactions between gaze-evoked blinks and gaze shifts in monkeys. Experimental brain research, 216(3), 321-339.
- Basso, M. A., & May, P. J. (2017). Circuits for Action and Cognition: A View from the Superior Colliculus. Annual Review of Vision Science, 3, 197-226.
- Doehring, A., Oertel, B. G., Sittl, R., & Lötsch, J. (2013). Chronic opioid use is associated with increased DNA methylation correlating with increased clinical pain. Pain, 154(1), 15-23.
- Levine, P. A. (2015). Trauma and memory: Brain and body in a search for the living past: A practical guide for understanding and working with traumatic memory. North Atlantic Books.
- Phelps, E. A., & LeDoux, J. E. (2005). Contributions of the amygdala to emotion processing: from animal models to human behavior. Neuron, 48(2), 175-187.
- Shin, L. M., & Liberzon, I. (2010). The neurocircuitry of fear, stress, and anxiety disorders. Neuropsychopharmacology, 35(1), 169-191.
- Landin-Romero, R., Moreno-Alcazar, A., Pagani, M., & Amann, B. L. (2018). How does eye movement desensitization and reprocessing therapy work? A systematic review on suggested mechanisms of action. Frontiers in psychology, 9, 1395.
- Lee, C. W., & Cuijpers, P. (2013). A meta-analysis of the contribution of eye movements in processing emotional memories. Journal of behavior therapy and experimental psychiatry, 44(2), 231-239.
- Bird, C. M. (2017). The role of the hippocampus in recognition memory. Cortex, 93, 155-165.
- Bremner, J. D. (2006). Traumatic stress: effects on the brain. Dialogues in clinical neuroscience, 8(4), 445.
- Calancie, O. G., Khalid-Khan, S., Booij, L., & Munoz, D. P. (2018). Eye movement desensitization and reprocessing as a treatment for PTSD: current neurobiological theories and a new hypothesis. Annals of the New York Academy of Sciences, 1426(1), 92-105.
- Högberg, G., Pagani, M., Sundin, Ö., Soares, J., Åberg-Wistedt, A., Tärnell, B., & Hällström, T. (2008). Treatment of post-traumatic stress disorder with eye movement desensitization and reprocessing: Outcome is stable in 35-month follow-up. Psychiatry research, 159(1-2), 101-108.
- Stevens, F. L., Hurley, R. A., & Taber, K. H. (2011). Anterior cingulate cortex: unique role in cognition and emotion. The Journal of neuropsychiatry and clinical neurosciences, 23(2), 121-125.
- Etkin, A., Egner, T., & Kalisch, R. (2011). Emotional processing in anterior cingulate and medial prefrontal cortex. Trends in cognitive sciences, 15(2), 85-93.
- Herrmann, M. J., Katzorke, A., Busch, Y., Gromer, D., Polak, T., Pauli, P., & Deckert, J. (2017). Medial prefrontal cortex stimulation accelerates therapy response of exposure therapy in acrophobia. Brain stimulation, 10(2), 291-297.
- Schiller, D., & Delgado, M. R. (2010). Overlapping neural systems mediating extinction, reversal and regulation of fear. Trends in cognitive sciences, 14(6), 268-276.
- Etkin, A., Büchel, C., & Gross, J. J. (2015). The neural bases of emotion regulation. Nature reviews neuroscience, 16(11), 693-700.
- Dixon, M. L., Thiruchselvam, R., Todd, R., & Christoff, K. (2017). Emotion and the prefrontal cortex: An integrative review. Psychological bulletin, 143(10), 1033.
- Lanius, R. A., Frewen, P. A., Tursich, M., Jetly, R., & McKinnon, M. C. (2015). Restoring large-scale brain networks in PTSD and related disorders: a proposal for neuroscientifically-informed treatment interventions. European journal of psychotraumatology, 6(1), 27313.
- Pagani, M., Di Lorenzo, G., Monaco, L., Niolu, C., Siracusano, A., Verardo, A. R., … & Ammaniti, M. (2015). Neurobiological correlates of EMDR monitoring–an EEG study. PloS one, 10(9), e0123931.
- Thomaes, K., Dorrepaal, E., Draijer, N., de Ruiter, M. B., Elzinga, B. M., van Balkom, A. J., … & Veltman, D. J. (2012). Treatment effects on insular and anterior cingulate cortex activation during classic and emotional Stroop interference in child abuse-related complex post-traumatic stress disorder. Psychological medicine, 42(11), 2337-2349.
- Nicholson, A. A., Ros, T., Frewen, P. A., Densmore, M., Théberge, J., Kluetsch, R. C., … & Lanius, R. A. (2016). Alpha oscillation neurofeedback modulates amygdala complex connectivity and arousal in posttraumatic stress disorder. NeuroImage: Clinical, 12, 506-516.
- Hildebrand, A. (2014). Bridging the gap between neuroscience and psychotherapy–the example of brainspotting. In Neurobiology and treatment of traumatic dissociation (pp. 343-362). Springer, New York, NY.
- Grand, D. (2011). Brainspotting: a new brain-based psychotherapy approach. Trauma and Gewalt, 3, 276-85.
- Shapiro, F. (2014). The role of eye movement desensitization and reprocessing (EMDR) therapy in medicine: addressing the psychological and physical symptoms stemming from adverse life experiences. The Permanente Journal, 18(1), 71.
- Andrade, J., Kavanagh, D., & Baddeley, A. (1997). Eye‐movements and visual imagery: A working memory approach to the treatment of post‐traumatic stress disorder. British journal of clinical psychology, 36(2), 209-223.
- Armstrong, M. S., & Vaughan, K. (1996). An orienting response model of eye movement desensitization. Journal of behavior therapy and experimental psychiatry, 27(1), 21-32.
- Siegel, D. J. (2007). The mindful brain: Reflection and attunement in the cultivation of well-being. WW Norton & company.
- Levine, P. A., & Frederick, A. (1997). Waking the tiger: Healing trauma: The innate capacity to transform overwhelming experiences. North Atlantic Books.
- Scaer, R. C. (2014). The body bears the burden: Trauma, dissociation, and disease. Routledge.
- Shapiro, F. (2017). Eye movement desensitization and reprocessing (EMDR) therapy: Basic principles, protocols, and procedures. Guilford Publications.
- Corrigan, F. M. (2002). Mindfulness, dissociation, EMDR and the anterior cingulate cortex: a hypothesis. Contemporary Hypnosis, 19(1), 8-17.
- Kip, K. E., Rosenzweig, L., Hernandez, D. F., Shuman, A., Sullivan, K. L., Long, C. J., … & Diamond, D. M. (2013). Randomized controlled trial of accelerated resolution therapy (ART) for symptoms of combat-related post-traumatic stress disorder (PTSD). Military medicine, 178(12), 1298-1309.
- Nieuwenhuis, S., Elzinga, B. M., Ras, P. H., Berends, F., Duijs, P., Samara, Z., & Slagter, H. A. (2013). Bilateral saccadic eye movements and tactile stimulation, but not auditory stimulation, enhance memory retrieval. Brain and cognition, 81(1), 52-56.
- Woodman, G. F. (2010). A brief introduction to the use of event-related potentials in studies of perception and attention. Attention, Perception, & Psychophysics, 72(8), 2031-2046.
- Folstein, J. R., & Van Petten, C. (2008). Influence of cognitive control and mismatch on the N2 component of the ERP: a review. Psychophysiology, 45(1), 152-170.
- Schupp, H. T., Stockburger, J., Codispoti, M., Junghöfer, M., Weike, A. I., & Hamm, A. O. (2007). Selective visual attention to emotion. Journal of neuroscience, 27(5), 1082-1089.
- Polich, J. (2007). Updating P300: an integrative theory of P3a and P3b. Clinical neurophysiology, 118(10), 2128-2148.
- Hajcak, G., MacNamara, A., & Olvet, D. M. (2010). Event-related potentials, emotion, and emotion regulation: an integrative review. Developmental neuropsychology, 35(2), 129-155.
- Sarlo, M., Buodo, G., Poli, S., & Palomba, D. (2005). Changes in EEG alpha power to different disgust elicitors: the specificity of mutilations. Neuroscience letters, 382(3), 291-296.
- Cuthbert, B. N., Schupp, H. T., Bradley, M. M., Birbaumer, N., & Lang, P. J. (2000). Brain potentials in affective picture processing: covariation with autonomic arousal and affective report. Biological psychology, 52(2), 95-111.
- Olofsson, J. K., Nordin, S., Sequeira, H., & Polich, J. (2008). Affective picture processing: an integrative review of ERP findings. Biological psychology, 77(3), 247-265.
- Foti, D., & Hajcak, G. (2008). Deconstructing reappraisal: Descriptions preceding arousing pictures modulate the subsequent neural response. Journal of cognitive neuroscience, 20(6), 977-988.
- Coben, R., & Evans, J. R. (Eds.). (2010). Neurofeedback and neuromodulation techniques and applications. Academic Press.
- van den Heuvel, M. P., & Hulshoff Pol, H. E. (2010). Exploring the brain network: a review on resting-state fMRI functional connectivity. European neuropsychopharmacology, 20(8), 519-534.
- Thatcher, R. W., North, D., & Biver, C. (2005). EEG and intelligence: relations between EEG coherence, EEG phase delay and power. Clinical neurophysiology, 116(9), 2129-2141.
- Sauseng, P., Klimesch, W., Schabus, M., & Doppelmayr, M. (2005). Fronto-parietal EEG coherence in theta and upper alpha reflect central executive functions of working memory. International Journal of Psychophysiology, 57(2), 97-103.
- Cvetkovic, D., & Cosic, I. (Eds.). (2011). States of consciousness: Experimental insights into meditation, waking, sleep and dreams (Vol. 1). Springer Science & Business Media.
- Mumtaz, W., Malik, A. S., Yasin, M. A. M., & Xia, L. (2015). Review on EEG and ERP predictive biomarkers for major depressive disorder. Biomedical Signal Processing and Control, 22, 85-98.
- Putman, P., Van Peer, J., Maimari, I., & Van der Werff, S. (2010). EEG theta/beta ratio in relation to fear-modulated response-inhibition, attentional control, and affective traits. Biological psychology, 83(2), 73-78.
- Knyazev, G. G. (2007). Motivation, emotion, and their inhibitory control mirrored in brain oscillations. Neuroscience & Biobehavioral Reviews, 31(3), 377-395.
- Buzsáki, G., & Draguhn, A. (2004). Neuronal oscillations in cortical networks. Science, 304(5679), 1926-1929.
- Klimesch, W. (1999). EEG alpha and theta oscillations reflect cognitive and memory performance: a review and analysis. Brain research reviews, 29(2-3), 169-195.
- Gruzelier, J. H. (2014). EEG-neurofeedback for optimising performance. I: a review of cognitive and affective outcome in healthy participants. Neuroscience & Biobehavioral Reviews, 44, 124-141.
- Thompson, M., & Thompson, L. (2015). The neurofeedback book: An introduction to basic concepts in applied psychophysiology. Association for Applied Psychophysiology and Biofeedback.
- Kluetsch, R. C., Ros, T., Théberge, J., Frewen, P. A., Calhoun, V. D., Schmahl, C., … & Lanius, R. A. (2014). Plastic modulation of PTSD resting‐state networks and subjective wellbeing by EEG neurofeedback. Acta Psychiatrica Scandinavica, 130(2), 123-136.









0 Comments