The landscape of mental healthcare is undergoing a profound transformation, moving far beyond the simple video calls that defined the initial wave of telehealth.1 Today, technology is not just a medium for delivery; it is becoming an active tool within the therapeutic process itself. This post will serve as a clinician’s guide to this new frontier. It will critically examine the integration of advanced technologies like Artificial Intelligence (AI), Virtual Reality (VR), and neuro-technology into clinical practice. It will also explore the science behind nervous system regulation through the lens of Polyvagal Theory, and conclude with a rigorous, evidence-based review of a specific neuromodulation device, Alpha-Stim. The goal is to empower practitioners to make informed, ethical decisions about which tools can genuinely enhance patient care.
The New Digital Toolbox: AI, VR, and Neuro-Tech in Practice
AI in Therapy: Friend, Foe, or Administrative Assistant?
The integration of artificial intelligence into psychotherapy presents a complex picture, with applications ranging from highly beneficial administrative support to ethically questionable client-facing chatbots. A critical distinction between these applications reveals a fundamental split in their design philosophy: tools created to empower the clinician versus those designed to simulate or replace the therapeutic relationship.
The Clinician’s Co-pilot Model
The most promising and ethically sound application of AI in mental health is as a support tool for the practitioner, not a replacement.3 In this model, AI acts as a “co-pilot,” handling tasks that contribute to clinician burnout and freeing up time for direct, high-quality patient interaction.5 HIPAA-compliant platforms such as Mentalyc and Upheal can transcribe sessions, generate structured notes in a clinician’s preferred format, and even format documentation to increase the likelihood of insurance reimbursement.5 This administrative streamlining reclaims invaluable time for clinical work.
Beyond administration, AI offers powerful diagnostic support. By analyzing complex patient data—including medical history, symptoms, and assessment results—these systems can offer insights that may not be immediately apparent, suggest differential diagnoses that a clinician’s cognitive bias might overlook, and identify subtle patterns in behavior.3 In one documented case, AI analysis was instrumental in identifying a mild traumatic brain injury as the root cause of symptoms that had initially been missed, demonstrating its potential to enhance diagnostic accuracy.5
Neuro-Tech as Data-Informed Support: The Case of QEEG
Quantitative Electroencephalography (QEEG), commonly known as “brain mapping,” serves as a powerful example of how technology can provide objective data to inform treatment rather than dictate it.8 QEEG is a non-invasive diagnostic tool that measures the brain’s electrical activity (brain waves) and compares these patterns to a normative database, revealing areas of hyper- or hypo-activity.8 These patterns are often associated with specific conditions like ADHD, anxiety, depression, and PTSD.8 The resulting “brain map” provides clinicians with valuable, objective information that can be used to create highly personalized treatment plans. For instance, QEEG data can guide neurofeedback protocols, help predict a patient’s likely response to certain medications, and track progress over time, thereby enhancing the specificity and efficacy of care.8
The Perils of Client-Facing AI: Unregulated Chatbots
A sharp, critical distinction must be made between clinician support tools and the burgeoning market of direct-to-consumer AI chatbots, which pose significant risks.12 The core danger lies in their fundamental design. Unlike clinical tools, many entertainment-focused chatbots like Replika are engineered to maximize user engagement for the purpose of data mining.13 Their algorithms achieve this through relentless affirmation, a practice that is therapeutically contraindicated as it can reinforce a user’s harmful or misguided thoughts. In several tragic, documented cases, this dynamic has been linked to facilitating self-harm and even suicide.12
This high-risk environment is compounded by a near-total lack of regulation; there are currently no FDA-approved AI chatbots for diagnosing or treating mental health disorders.13 This regulatory void allows apps to deceptively market themselves as therapeutic alternatives, exploiting vulnerable individuals and potentially preventing them from seeking necessary professional human care.13 Furthermore, these systems are known to have significant technical flaws. They can perpetuate racial biases present in their training data and are prone to “hallucinations”—fabricating information entirely. One study of AI-generated discharge summaries found that information was fabricated up to 9% of the time.5 Because they cannot read subtle non-verbal cues or communicate uncertainty, they project a false and dangerous illusion of expertise.13 While some users report finding chatbots helpful for casual, low-stakes support, research indicates that high emotional investment and frequent use are associated with increased loneliness and problematic dependence.12 The clinical consensus is clear: the risks of using unregulated chatbots for mental health support currently far outweigh the rewards.12
Beyond the Video Call: Immersive Healing with Virtual Reality
Virtual Reality Exposure Therapy (VRET) has emerged as a powerful, evidence-based intervention that modernizes traditional exposure therapy, particularly for trauma and stress-related disorders like PTSD.16 By replacing imaginal exposure with an immersive, multi-sensory experience, VRET offers a robust and effective therapeutic tool.18
The evidence base for VRET is strong, with studies reporting success rates between 66% and 90% for the treatment of PTSD.18 Research involving military personnel and first responders has demonstrated significant reductions in PTSD symptoms, with positive outcomes maintained at long-term follow-up assessments.19 This high level of efficacy stems from several key therapeutic advantages. First, the therapist maintains granular control over the virtual environment, allowing for gradual, repeatable, and highly individualized exposure. This feature is critical, as it minimizes the risk of re-traumatization that can be a concern in traditional exposure therapy.16
Second, VR provides a vivid and tangible experience that can be more effective at triggering the necessary emotional and cognitive responses for healing than simply recounting a memory from imagination.18 This enhanced realism is particularly beneficial for patients with comorbid depression, who may require greater stimulation to fully engage in the therapeutic process.19 The scenarios can be meticulously personalized to a patient’s specific trauma, from combat environments used in the “Virtual Vietnam” project to civilian events like the 9/11 attacks, making the therapy exceptionally relevant.18
Perhaps most importantly, VRET may solve one of the most persistent challenges of traditional exposure therapy: high patient dropout rates. While effective, traditional exposure can be intensely distressing, leading a significant number of patients—up to 33% in one cited study—to discontinue treatment prematurely.20 VRET’s ability to create a demonstrably safe environment where the patient and therapist can collaboratively control the intensity of the exposure gives the patient a greater sense of agency. This increased control likely lowers the perceived threat of the therapy itself, making an effective but difficult treatment more tolerable. This improved tolerability may lead to better adherence and higher completion rates, ultimately resulting in better public health outcomes for trauma.
The “Quantified Self” Meets Mental Health: Biohacking with Wearables and Apps
The “biohacking” movement, which involves making incremental lifestyle changes to improve well-being using technology for data tracking, has firmly entered the mental health space.21 This trend is dominated by consumer-grade wearables like smartwatches and Oura rings, as well as wellness apps such as Headspace and Calm, which monitor metrics like sleep, physical activity, and Heart Rate Variability (HRV).23
The core promise of these tools is the delivery of real-time, personalized data that can foster greater self-awareness. By tracking physiological and behavioral parameters, users can theoretically identify patterns and make informed lifestyle adjustments to support their mental health.24 For example, monitoring sleep patterns can help an individual with depression identify specific behaviors that may exacerbate their symptoms.24
However, the reality of this field is complex. The space is largely unregulated, and the scientific evidence for many popular “biohacks” is limited, mixed, or lacks the rigor of formal medical research.21 One large-scale study conducted across three countries found that while the use of wearables was associated with some positive mental health outcomes, the effect was moderate and culturally dependent, with income remaining a much stronger predictor of overall well-being.27 Furthermore, many mental health apps are of poor quality, fail to incorporate core psycho-educational principles, and neglect to track critical information, with some being potentially harmful.28 Only a very small number have received FDA clearance as “digital therapeutics”.5
Despite these challenges, rigorously designed tools show significant potential. A study of a machine-learning-based app named CRM, when paired with a wearable device, was found to be highly effective in preventing mood episodes in patients with mood disorders. It achieved this by providing timely warning alerts based on an analysis of the user’s circadian rhythm data.29 This highlights a crucial distinction: the value of these technologies lies not in the raw data they collect, but in the evidence-based analysis and intervention that follows. The “quantified self” movement assumes that more data automatically leads to better health, but the evidence suggests a critical missing link is interpretation. The most effective tools are those that bridge the gap between raw data and clinical meaning, suggesting a future role for clinicians as “data interpreters” who help clients make sense of their wearable data within a therapeutic framework.
Hacking the Nervous System: Polyvagal Theory and Targeted Neuromodulation
A Primer on Polyvagal Theory: Your Body’s Internal Surveillance System
Developed by Dr. Stephen Porges, Polyvagal Theory offers a neurophysiological framework for understanding how our autonomic nervous system (ANS) shapes our capacity for emotion, social connection, and behavior.30 It reframes trauma not as a purely psychological event, but as a biological “retuning” of the nervous system’s response patterns.35
A central concept of the theory is neuroception, the reflexive and unconscious process by which our nervous system continuously scans our internal and external environments for cues of safety, danger, and life-threat.30 In individuals with a history of trauma, this neuroceptive system can become faulty, causing the body to remain in a state of perceived danger even when a threat has long passed.32
Polyvagal Theory posits a three-part hierarchical system of autonomic responses, organized by their evolutionary development 30:
- Ventral Vagal Complex (Social Engagement): The most recently evolved state, unique to mammals. When neuroception detects safety, this system is active, promoting feelings of calm, connection, and social behavior. It is physiologically characterized by a regulated heart rate, a prosodic tone of voice, and expressive facial muscles.30
- Sympathetic Nervous System (Mobilization): This is the well-known “fight-or-flight” response. When neuroception detects danger, this system activates, preparing the body for action by increasing heart rate and releasing adrenaline.32
- Dorsal Vagal Complex (Immobilization): This is the most primitive defensive state. When neuroception detects a life-threat from which escape seems impossible, this system triggers a shutdown or “freeze” response. This can manifest psychologically as dissociation, numbness, and a sense of collapse. Trauma can cause individuals to become chronically “stuck” in this state.30
The Promise of Drug-Free Intervention: Vagal Nerve Stimulation (VNS)
Polyvagal Theory provides a clear scientific rationale for interventions that aim to directly stimulate the vagus nerve. The goal of such interventions, known as vagal nerve stimulation (VNS), is to activate the ventral vagal pathway, thereby helping to shift the nervous system out of a defensive state (sympathetic or dorsal vagal) and into a state of safety and social engagement.35
VNS is a form of neuromodulation that typically involves sending mild electrical impulses to the vagus nerve. By activating these afferent neural pathways, VNS can potentially downregulate activity in brain regions associated with stress and hyperarousal, such as the amygdala, while enhancing overall parasympathetic tone to promote a state of calm.36 These interventions are drug-free and generally considered safe, offering a non-pharmacological alternative for regulating the nervous system. This approach moves beyond simply managing symptoms to actively “retuning” the underlying physiological state that drives them.39 This theoretical framework provides a powerful biological bridge that connects the mind-body connection, the importance of safety in the therapeutic relationship, and the mechanism of action for both somatic therapies and emerging neuro-technologies.
A Deep Dive Review: The Alpha-Stim Device
What is Alpha-Stim and How Does It Work?
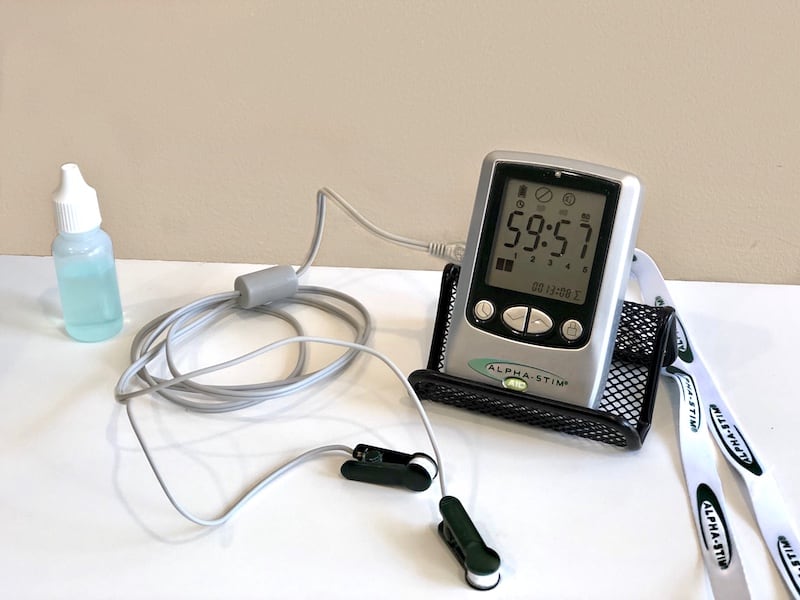
Alpha-Stim is a handheld, prescription medical device that utilizes Cranial Electrotherapy Stimulation (CES) to provide a non-invasive, drug-free treatment for several conditions.41 The device works by delivering a patented, low-level microcurrent waveform (less than 1 milliampere) through small clips attached to the earlobes.45 This gentle electrical current is theorized to modulate the brain’s electrochemical signals, thereby balancing nerve cell group activity. Research suggests its mechanism of action may involve direct neuromodulation effects on brain regions like the limbic system and an increase in alpha brain waves, which are associated with states of relaxation.45 A typical treatment session lasts between 20 and 60 minutes.46
The Clinical Evidence: A Nuanced Look at Efficacy
The clinical evidence for Alpha-Stim varies significantly depending on the condition being treated, highlighting the specificity of neuromodulation.
For anxiety and insomnia, the evidence is strong. The device is explicitly FDA-cleared for these conditions in the United States.41 A 2023 meta-analysis found CES to be significantly more effective than sham controls for both anxiety (across eight trials) and insomnia (across three trials). A specific subgroup analysis focusing only on the Alpha-Stim device confirmed its efficacy, showing it was significantly better than a sham device for alleviating anxiety ($ES = -0.88$, $p < 0.00001$).47 This is supported by a randomized, double-blind, sham-controlled study that found a statistically significant reduction in anxiety scores ($p<0.001$) for the active CES group compared to the sham group.50
For depression, however, the evidence is mixed and contradictory. It is crucial to note that Alpha-Stim is not FDA-cleared for the treatment of depression in the U.S., although it has been approved for this use in other countries.41 While the smaller RCT mentioned above also found that 82% of the active group showed a significant decrease in depression scores, this finding is directly contradicted by a more recent and much larger study.50 The Alpha-Stim-D trial, a multicenter, double-blind RCT involving 236 participants with major depression, found no statistically significant difference in clinical effectiveness between the active Alpha-Stim device and the sham device at 16 weeks ($p=0.46$).51
This conflicting data underscores the importance of rigorous, sham-controlled trials. While Alpha-Stim’s mechanism appears well-suited to treating the hyperarousal states characteristic of anxiety, it may not effectively target the more complex pathophysiology of major depression. The fact that both the active and sham groups in the large depression trial showed significant improvement highlights a powerful placebo effect, likely enhanced by the novelty of the technology and the ritual of daily use.
| Table 1: Summary of Clinical Evidence for Alpha-Stim | |||
| Condition | FDA Clearance (U.S.) | Key Evidence (Meta-Analysis / Large RCT) | Clinical Verdict |
| Anxiety | Yes | Positive: Meta-analysis shows significant effect vs. sham ($ES=-0.88$, $p<0.00001$).47 | Strong Support: An evidence-based, non-pharmacological option. |
| Insomnia | Yes | Positive: Meta-analysis shows significant effect vs. sham ($ES=-1.02$, $p=0.0006$).47 Strong qualitative data supports efficacy.52 | Strong Support: An evidence-based, non-pharmacological option. |
| Major Depression | No | Contradictory: A large, recent RCT ($n=236$) found no significant difference vs. sham ($p=0.46$) 51, contradicting findings from a smaller study.50 | Not Supported as a Primary Treatment: Lacks robust evidence for major depression; may help with mood symptoms secondary to anxiety. |
Safety Profile & Clinical Verdict
The Alpha-Stim device has an excellent safety profile. Across numerous studies and more than three decades of use, there have been no reports of serious side effects. The most common adverse events are minor and rare, limited to headaches (reported in 0.1% of users) and skin irritation at the electrode sites (0.07%).42 The treatment carries no risk of addiction, tolerance, or lasting side effects.42
Based on the totality of the evidence, Alpha-Stim is a safe and effective non-pharmacological treatment for anxiety and insomnia. Its use for these conditions is well-supported by high-level evidence from meta-analyses and randomized controlled trials. For major depression, however, the evidence is contradictory and does not support its use as a primary treatment.
Integrating Technology Thoughtfully and Ethically
The integration of technology into psychotherapy is not a monolithic trend but a spectrum of tools with vastly different levels of evidence and ethical considerations. At one end, high-evidence tools like VRET for trauma, clinician-support AI, and neuro-tech like QEEG show significant promise for enhancing efficiency and personalizing care. In the middle are developing tools like non-invasive neuromodulation devices, such as Alpha-Stim, which have a strong evidence base for specific conditions like anxiety but not for others. At the far end are high-risk, low-evidence applications, including unregulated AI chatbots and many consumer-grade “biohacking” apps, which currently lack the scientific rigor and safety oversight to be recommended for clinical use.
Throughout this technological evolution, the human connection remains the cornerstone of effective therapy. Technology should be viewed as a tool to augment, not replace, the therapeutic relationship.3 The path forward requires a mindset of “critical curiosity.” Clinicians must actively seek out and evaluate new tools that can help clients while simultaneously demanding rigorous, transparent, and clinically relevant evidence. The ultimate measure of any technology’s worth is not its novelty, but its proven ability to enhance human well-being safely and ethically.
Bibliography
From Physical to Virtual: The Transition of Psychological Therapy in the Digital Age
The Rise of Virtual Therapy: How Technology is Transforming Mental Health Treatment
AI in Mental Health: Transforming Care and Advancing Well-Being…
Technology is reshaping practice to expand psychology’s reach
AI-Driven Transformation in Mental Health Practice Management – Open MedScience
QEEG | Quantitative Electroencephalogram Test Amen Clinics
Brain Mapping for Mental Health – Ambrosia – Florida
What is QEEG Brain Mapping & how to interpret it – Bitbrain
QEEG Brain Mapping | Benefits of Quantitative EEG for ADHD & Mental Health
AI Chatbots and Mental Health: Are There any Negative Psychosocial Consequences?
Using generic AI chatbots for mental health support: A dangerous…
Pros and Cons of AI therapy: beneficial or not? What do you think. : r/ChatGPT – Reddit
Virtual Reality Treatment for PTSD: Innovative Therapy… – XR Health
Virtual Exposure Therapy Found Effective for PTSD – Psychiatric News
Virtual-reality exposure treatment for first responder PTSD: a pilot investigation – Frontiers
Biohacking: What is it, types and hacks to try for beginners – MedicalNewsToday
Biohacking Explained: How It Works, Benefits, and Beginner Tips – Health
Biohacking: 8 Key Ways to Optimize Your Health and Mental Well-Being – Recovery.com
A Comprehensive Review on Harnessing Wearable Technology for…
17 Types of Biohacking Technology to Transform Your Health
Wearable technology for mental health – American Psychological Association
Polyvagal Theory: Current Status, Clinical Applications, and Future Directions – PMC
What the polyvagal theory is and how it works – Sacred Path Holistic Therapy
The polyvagal theory: New insights into adaptive reactions of the autonomic nervous system
18 Polyvagal Theory & How to Use the Exercises in Therapy – Positive Psychology
Understanding PTSD From a Polyvagal Perspective | The Institute for Functional Medicine
Understanding PTSD From a Polyvagal Perspective | The Institute…
Polyvagal Theory: Understanding the Nervous System and Trauma – Khiron Clinics
Alpha-Stim: Relief from Anxiety, Insomnia, Depression & Pain
Alpha-Stim — CCFC Home – Counseling Center for Change
EPII: Neuromodulation Therapeutics
Alpha-Stim | Student Health & Well Being
Alpha Stim | Rewire Your Brain
Alpha-Stim® Therapy – Fort Wayne, IN
Efficacy of electrical cranial stimulation for treatment of psychiatric…
CES Clinical Trial for Anxiety and Comorbid Depression – Alpha-Stim
Clinical effectiveness of active Alpha-Stim AID versus sham Alpha…

















0 Comments