Current Evidence and Dietary Considerations for sperger’s Syndrome
Asperger’s syndrome, now classified as part of autism spectrum disorder (ASD) in the DSM-5, is characterized by challenges in social interaction and communication, alongside restricted and repetitive patterns of behavior and interests. While conventional treatments focus on behavioral, educational, and psychosocial interventions, growing interest has emerged in the potential role of nutritional approaches in managing symptoms and supporting overall well-being. This comprehensive review examines the current evidence for various nutritional interventions and dietary strategies that may benefit individuals with Asperger’s syndrome.
Understanding Asperger’s Syndrome and Nutrition’s Potential Role
Asperger’s syndrome represents a form of autism spectrum disorder typically without significant language or cognitive delays. Individuals with Asperger’s often demonstrate average to above-average intelligence, but experience challenges with social interaction, nonverbal communication, and sometimes exhibit intense interests in specific topics.
Emerging research suggests that various physiological mechanisms in ASD may be influenced by nutritional status. Key biological factors in Asperger’s syndrome that intersect with nutrition include:
- Gastrointestinal dysfunction: Higher rates of digestive issues and altered gut microbiome composition
- Immune system irregularities: Increased inflammatory markers and immune dysregulation
- Oxidative stress: Higher levels of oxidative damage markers and lower antioxidant capacity
- Mitochondrial dysfunction: Impaired cellular energy production in some individuals
- Neurotransmitter imbalances: Alterations in systems involving serotonin, dopamine, and GABA
These mechanisms provide multiple potential targets for nutritional interventions. While nutrition alone cannot treat Asperger’s syndrome, evidence suggests specific nutrients and dietary approaches may help modulate these systems and potentially improve certain symptoms and quality of life.
Omega-3 Fatty Acids: Building Blocks for Brain Function
Omega-3 fatty acids, particularly docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA), are essential fats critical for brain development and function. These fatty acids are structural components of neural cell membranes and influence numerous aspects of brain function relevant to ASD.
Mechanisms of Action
Omega-3 fatty acids may benefit those with Asperger’s syndrome through several pathways:
- Anti-inflammatory effects: Reducing neuroinflammation potentially associated with ASD
- Neurotransmitter regulation: Influencing dopamine and serotonin function
- Cell membrane fluidity: Improving neuronal signaling and receptor function
- Neuroprotection: Supporting healthy brain development and function
Research Evidence
Research on omega-3 supplementation for ASD shows mixed but promising results:
Several systematic reviews and meta-analyses have examined omega-3 fatty acid supplementation in ASD. While results are mixed, some studies show improvements in certain behavioral measures, particularly hyperactivity, lethargy, and stereotypy. A 2017 meta-analysis found small but significant effects for specific ASD symptoms.
For individuals with Asperger’s specifically, who typically have fewer cognitive challenges but significant social difficulties, omega-3s may provide modest benefits for irritability and hyperactivity, though effects on core social symptoms appear less consistent.
The research indicates that response to omega-3 supplementation varies considerably between individuals, suggesting personalized approaches based on baseline omega-3 status might be necessary.
Clinical Applications
For those considering omega-3 supplementation:
- Dosage: Most studies used 1-1.5 grams daily of combined EPA and DHA
- EPA
ratio: Higher EPA formulations may provide better behavioral benefits
- Duration: At least 12 weeks of consistent use to assess effectiveness
- Quality: Purified supplements tested for contaminants and oxidation
- Food sources: Fatty fish (salmon, sardines, mackerel), though supplementation is typically needed to reach therapeutic doses
Vitamin D: The Sunshine Nutrient
Vitamin D has numerous functions beyond bone health, including roles in brain development, immune regulation, and gene expression. A growing body of research has identified associations between vitamin D status and ASD.
Mechanisms and Evidence
Vitamin D may influence ASD through several pathways:
- Neurodevelopment: Critical for proper brain development during prenatal and early childhood periods
- Immune regulation: Modulating immune function and inflammation
- Gene expression: Influencing the expression of numerous genes involved in brain function
- Neuroprotection: Supporting healthy neural growth and function
Research consistently shows associations between vitamin D deficiency and ASD. Multiple studies have found lower vitamin D levels in children with ASD compared to typically developing peers. Some research suggests correlations between vitamin D status and symptom severity.
Supplementation studies show preliminary promise. Small clinical trials of vitamin D supplementation in children with ASD have reported improvements in certain behavioral measures, though research specific to Asperger’s syndrome is limited.
Clinical Applications
For vitamin D considerations in Asperger’s syndrome:
- Testing: Measuring 25-hydroxyvitamin D levels to assess deficiency (levels below 30 ng/mL)
- Dosage: Typically 1,000-2,000 IU daily for children and 2,000-4,000 IU for adults, depending on baseline levels
- Monitoring: Periodic retesting to ensure optimal blood levels (typically 30-50 ng/mL)
- Sources: While sunlight exposure is the natural method, supplementation is often necessary, especially in northern latitudes or for those with limited sun exposure
B Vitamins: Supporting Methylation and Energy
B vitamins play crucial roles in methylation processes, energy production, and neurotransmitter synthesis. Several B vitamins have been studied in the context of ASD:
Folate (Vitamin B9)
Folate is essential for one-carbon metabolism, DNA synthesis, and gene expression regulation. Abnormalities in folate metabolism have been identified in some individuals with ASD:
- Research shows associations between maternal folate status during pregnancy and ASD risk
- Some individuals with ASD may have genetic variations affecting folate metabolism (e.g., MTHFR polymorphisms)
- Cerebral folate deficiency, a condition involving reduced folate transport to the brain, occurs in some individuals with ASD
For those with identified folate-related issues, supplementation with the bioactive form methylfolate may be more beneficial than folic acid, particularly for individuals with MTHFR mutations.
Vitamin B6 and Magnesium
The combination of vitamin B6 (typically as pyridoxine or the active form pyridoxal-5-phosphate) and magnesium has been studied for ASD:
- Several older studies reported improvements in behavior, speech, and social interaction
- More recent research shows mixed results, with some small trials showing modest benefits
- The combination may influence neurotransmitter production and function
While evidence is not strong enough for broad recommendations, some practitioners consider a trial of B6 and magnesium in cases where other approaches haven’t been sufficient.
Vitamin B12
Vitamin B12 is critical for methylation processes, nerve function, and energy metabolism:
- Some children with ASD show markers suggesting functional B12 deficiency
- Methyl B12 (methylcobalamin) administered via injection has shown positive results in small studies
- Improvements were noted in glutathione levels, oxidative stress markers, and certain behaviors
For individuals with Asperger’s syndrome specifically, research is limited, but those with indicators of methylation issues or oxidative stress might be candidates for assessment of B12 status.
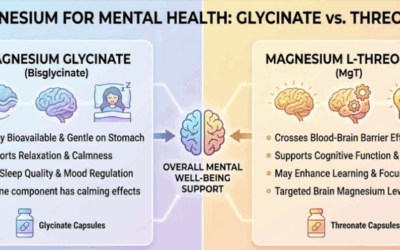
Magnesium: The Calming Mineral
Magnesium is involved in over 300 enzymatic reactions in the body and plays crucial roles in neurotransmitter function, energy production, and stress response. Some evidence suggests magnesium status may be relevant in ASD:
Mechanisms and Evidence
Magnesium may support those with Asperger’s syndrome by:
- GABA enhancement: Supporting the function of this calming neurotransmitter
- Glutamate regulation: Modulating excitatory neurotransmission
- Stress response modulation: Helping regulate the physiological stress response
- Energy metabolism: Supporting cellular energy production
Some studies have found lower magnesium levels in children with ASD compared to controls, though results are inconsistent. The combined supplementation of magnesium with vitamin B6 has shown modest benefits in small studies, potentially improving attention, communication, and reducing irritability in some children with ASD.
For individuals with Asperger’s who experience anxiety, sleep difficulties, or sensory sensitivities, magnesium supplementation might offer supportive benefits, though more research is needed.
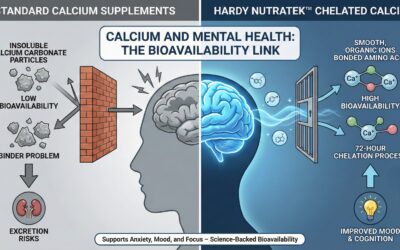
Clinical Applications
For magnesium in the context of Asperger’s syndrome:
- Dosage: Typically 3-5 mg/kg/day for children or 200-400 mg daily for adults
- Form: Magnesium glycinate or magnesium threonate may have better tolerability and brain bioavailability
- Monitoring: Watch for digestive side effects, which can indicate need for dose adjustment or form change
- Food sources: Green leafy vegetables, nuts, seeds, legumes, and whole grains
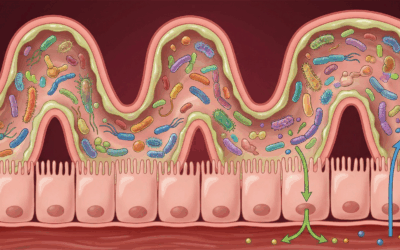
Probiotics and Gut Health
The gut-brain axis—the bidirectional communication between the digestive system and the brain—has emerged as an area of significant interest in ASD research. Many individuals with ASD, including those with Asperger’s syndrome, report gastrointestinal symptoms, and research suggests alterations in gut microbiome composition.
Mechanisms and Evidence
Probiotics and gut health approaches may benefit those with Asperger’s syndrome through:
- Microbiome modulation: Supporting a balanced intestinal microbial ecosystem
- Reducing inflammation: Addressing potential gut-derived inflammatory signals
- Improving barrier function: Enhancing intestinal barrier integrity
- Neurotransmitter production: Supporting production of serotonin and other neuroactive compounds produced in the gut
Research in this area is still emerging. Some studies have found differences in gut bacterial composition in individuals with ASD compared to controls. Small clinical trials of probiotic supplementation have shown modest benefits in reducing certain gastrointestinal symptoms and, in some cases, improvements in behavioral measures.
For individuals with Asperger’s syndrome who experience comorbid digestive issues such as constipation, diarrhea, or abdominal pain, addressing gut health might provide both digestive and potentially behavioral benefits.
Clinical Applications
For gut health approaches in Asperger’s syndrome:
- Probiotics: Multi-strain formulations containing Lactobacillus and Bifidobacterium species at doses of at least 10-20 billion CFUs
- Prebiotic foods: Fiber-rich foods that feed beneficial bacteria (e.g., fruits, vegetables, legumes)
- Fermented foods: Yogurt, kefir, sauerkraut, and other traditionally fermented foods
- Individualization: Responses to specific probiotics vary considerably between individuals
Specialized Dietary Approaches
Several specialized dietary approaches have been proposed for ASD, including Asperger’s syndrome. These range from elimination diets to specific therapeutic protocols:
Gluten-Free, Casein-Free (GFCF) Diet
The GFCF diet eliminates all sources of gluten (a protein found in wheat, barley, and rye) and casein (a protein found in dairy):
- Based on the theory that some individuals with ASD may have increased intestinal permeability and abnormal metabolism of gluten and casein peptides
- Some peptides derived from these proteins may have opioid-like activity that could potentially influence brain function
Research on the GFCF diet shows mixed results. Some studies report improvements in certain behavioral and gastrointestinal symptoms in subsets of children, while others find no significant effects. One challenge in interpreting research is identifying which individuals might respond to the diet, as it’s unlikely to benefit all with ASD.
For individuals with Asperger’s syndrome specifically, the GFCF diet might be considered particularly if there is:
- History of gastrointestinal symptoms that worsen with gluten or dairy consumption
- Family history of celiac disease or non-celiac gluten sensitivity
- Evidence of IgG antibodies to gluten or casein (though the clinical significance remains debated)
Low FODMAPs Diet
The low FODMAPs diet restricts certain types of fermentable carbohydrates that can trigger digestive symptoms in sensitive individuals:
- FODMAPs (Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols) include certain fruits, vegetables, grains, and dairy products
- This diet was developed for irritable bowel syndrome but may help some with ASD who have significant digestive symptoms
While not extensively studied in ASD, clinical experience suggests this approach may help reduce digestive discomfort in some individuals with Asperger’s syndrome who experience bloating, abdominal pain, or irregular bowel habits.
Ketogenic Diet
The ketogenic diet is a high-fat, adequate-protein, very low-carbohydrate diet that shifts metabolism toward ketone production:
- Originally developed for epilepsy treatment, which is more common in ASD
- Some small studies suggest potential benefits for certain behaviors in ASD
- Proposed mechanisms include effects on mitochondrial function, inflammation, and neurotransmitter systems
Research on the ketogenic diet for ASD is preliminary, with most studies being small case series or open-label trials. While some individuals show notable improvements, the diet is restrictive and requires careful medical supervision.
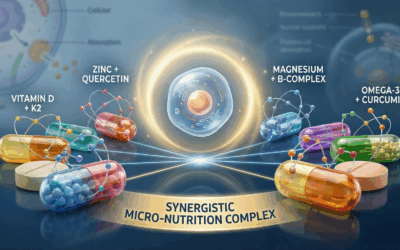
Anti-inflammatory Approaches
Emerging evidence suggests neuroinflammation may play a role in ASD. Several nutrients and food components with anti-inflammatory properties have been studied:
Curcumin
Curcumin, the active compound in turmeric, has potent anti-inflammatory and antioxidant properties:
- Small studies suggest potential benefits for irritability and certain behaviors in ASD
- Well-studied for its general neuroprotective properties
- Poor bioavailability requires special formulations (e.g., combined with piperine or in liposomal form)
Antioxidants
Various antioxidant compounds may help address oxidative stress found in some individuals with ASD:
- Vitamin C and E: Work synergistically to combat oxidative damage
- Coenzyme Q10: Supports mitochondrial function and provides antioxidant protection
- N-acetylcysteine (NAC): Precursor to glutathione, the body’s master antioxidant
Small clinical trials of NAC have shown promising results for irritability and repetitive behaviors in ASD, though larger studies are needed to confirm these effects.
Nutrient Deficiencies and Testing
Some individuals with Asperger’s syndrome may have specific nutrient deficiencies or metabolic differences that could benefit from targeted nutritional intervention:
Common Nutritional Assessments
- Vitamin D status: 25-hydroxyvitamin D blood levels
- Iron status: Complete iron panel including ferritin
- Zinc and copper levels: Particularly the zinc-to-copper ratio
- Omega-3 fatty acid profile: Measuring EPA and DHA levels
- Methylation markers: Homocysteine, folate, and B12 status
- Oxidative stress markers: Glutathione and oxidative damage indicators
Individualized Approach
Nutritional assessment should be tailored to:
- Specific symptoms and presentation
- Dietary intake and restrictions
- Family history
- Medication use that may affect nutrient status
Working with healthcare providers knowledgeable about both ASD and nutrition allows for targeted assessment and intervention based on individual needs.
Practical Implementation Strategies
Implementing dietary changes with individuals with Asperger’s syndrome requires consideration of several factors:
Sensory Considerations
Many individuals with Asperger’s syndrome have sensory sensitivities that affect food acceptance:
- Texture: Preferences for certain textures and aversions to others
- Taste: Often heightened taste perception, particularly for bitter flavors
- Smell: Sensitivity to food aromas
- Visual presentation: Preferences regarding how food looks or is arranged
Strategies might include gradual introduction of new foods, involvement in food preparation, and respecting sensory preferences while gently expanding options.
Routine and Predictability
Individuals with Asperger’s syndrome often prefer routine and predictability:
- Scheduled mealtimes: Maintaining consistent meal schedules
- Gradual changes: Introducing dietary modifications slowly
- Visual supports: Using visual schedules or recipes
- Preparation: Providing advance notice about dietary changes
Focus on Nutrient Density
Given potential dietary restrictions and selective eating:
- Emphasize nutrient-dense foods that provide maximum nutritional value
- Ensure adequate protein intake for neurotransmitter production
- Include sources of healthy fats, particularly omega-3s when accepted
- Consider appropriate supplementation for identified deficiencies
Family Involvement
Dietary approaches work best with family support:
- Education about nutritional needs and rationale for changes
- Involving all family members in dietary modifications when possible
- Creating a supportive food environment at home
- Developing strategies for social eating situations and school
Integrating Nutritional Approaches with Conventional Care
Nutritional approaches should complement, not replace, evidence-based treatments for Asperger’s syndrome:
Communication with Healthcare Team
- Inform all healthcare providers about nutritional supplements and dietary approaches
- Discuss potential interactions with medications
- Create a coordinated care plan incorporating nutritional strategies
Monitoring and Assessment
- Track behaviors, symptoms, and quality of life measures when implementing dietary changes
- Document any adverse effects or challenges
- Periodically reassess nutritional status and adjust approaches as needed
Individualized Integration
- Combine nutritional strategies with behavioral, educational, and social interventions
- Recognize that nutritional needs change throughout development
- Adapt approaches based on individual response and changing circumstances
Research Limitations and Future Directions
Current evidence for nutritional approaches in Asperger’s syndrome has several limitations:
Research Challenges
- Small sample sizes in many studies
- Heterogeneity in ASD presentation
- Limited studies focused specifically on Asperger’s syndrome
- Variability in outcome measures and intervention protocols
- Publication bias favoring positive results
Future Research Needs
- Larger, well-designed randomized controlled trials
- Identification of biomarkers to predict responders to specific interventions
- Long-term studies on safety and efficacy
- Research on combinations of nutritional interventions
- Studies specifically focusing on adults with Asperger’s syndrome
The evidence supporting nutritional approaches for Asperger’s syndrome is growing but remains preliminary for many interventions. Omega-3 fatty acids, vitamin D, probiotics, and certain specialized diets show the most promising evidence, though individual responses vary considerably.
While nutrition alone cannot address all aspects of Asperger’s syndrome, addressing the biological foundations of the condition through evidence-based nutritional strategies may help improve quality of life and potentially reduce certain challenging symptoms. The unique characteristics of Asperger’s syndrome—including average to above-average cognitive abilities, intense interests, and often strong logical thinking—may actually facilitate engagement with nutritional approaches when the rationale is clearly explained.
For individuals with Asperger’s syndrome and their families, working with healthcare providers knowledgeable about both ASD and nutrition offers the best opportunity for developing personalized nutritional strategies that complement conventional care. With appropriate guidance and monitoring, nutritional approaches can become valuable components of a comprehensive strategy for supporting individuals with Asperger’s syndrome throughout life.
For more information on supplemens for mental health consult our comprehensive guide for micronutrient and supplement therapy and how it can treat specific issues and enhance certain modalities of therapy.
If you’re interested in exploring micronutrient therapy as part of your anxiety treatment plan, Hardy Nutritionals offers a range of products to fit your specific needs. Their Daily Essential Nutrients clinical strength formula provides comprehensive, research-backed dosages in convenient capsule or powder form.
For 15% off in savings, use the offer code “Taproot” at checkout on the Hardy Nutritionals website to receive 15% off your order. @ GetHardy.com
It’s important to remember that while micronutrient therapy can be a powerful tool for managing anxiety, it is not a replacement for professional mental health care. Always consult with a qualified healthcare provider before starting any new supplement regimen, particularly if you have pre-existing health conditions or are taking medications.
Disclaimer: These statements have not been evaluated by the Food and Drug Administration. These products are not intended to diagnose, treat, cure, or prevent any disease. Please consult with a qualified healthcare professional before beginning any supplement regimen, particularly if you are pregnant, nursing, have a medical condition, or are taking medications. The information on this website doesnot constitute medical advice. We recieve a small commision on sales with Hardy Nutritionals through our offer code. Our affiliation does not effect treatment or recomendations made by Taproot authors, therapists or other staff.
Bibliography
- Adams, J. B., Audhya, T., McDonough-Means, S., Rubin, R. A., Quig, D., Geis, E., … & Lee, W. (2011). Nutritional and metabolic status of children with autism vs. neurotypical children, and the association with autism severity. Nutrition & Metabolism, 8(1), 34.
- Bölte, S., Girdler, S., & Marschik, P. B. (2019). The contribution of environmental exposure to the etiology of autism spectrum disorder. Cellular and Molecular Life Sciences, 76(7), 1275-1297.
- Cryan, J. F., O’Riordan, K. J., Cowan, C. S., Sandhu, K. V., Bastiaanssen, T. F., Boehme, M., … & Dinan, T. G. (2019). The microbiota-gut-brain axis. Physiological Reviews, 99(4), 1877-2013.
- Doenyas, C. (2018). Dietary interventions for autism spectrum disorder: New perspectives from the gut–brain axis. Physiology & Behavior, 194, 577-582.
- El-Ansary, A., Bjørklund, G., Chirumbolo, S., & Alnakhli, O. M. (2017). Predictive value of selected biomarkers related to metabolism and oxidative stress in children with autism spectrum disorder. Metabolic Brain Disease, 32(4), 1209-1221.
- Frye, R. E., & Rossignol, D. A. (2014). Treatments for biomedical abnormalities associated with autism spectrum disorder. Frontiers in Pediatrics, 2, 66.
- Frye, R. E., Slattery, J., Delhey, L., Furgerson, B., Strickland, T., Tippett, M., … & Quadros, E. V. (2018). Folinic acid improves verbal communication in children with autism and language impairment: a randomized double-blind placebo-controlled trial. Molecular Psychiatry, 23(2), 247-256.
- Geraghty, M. E., Bates-Wall, J., Ratliff-Schaub, K., & Lane, A. E. (2010). Nutritional interventions and therapies in autism: A spectrum of what we know: Part 2. ICAN: Infant, Child, & Adolescent Nutrition, 2(2), 120-133.
- Ghalichi, F., Ghaemmaghami, J., Malek, A., & Ostadrahimi, A. (2016). Effect of gluten free diet on gastrointestinal and behavioral indices for children with autism spectrum disorders: a randomized clinical trial. World Journal of Pediatrics, 12(4), 436-442.
- Grimaldi, R., Gibson, G. R., Vulevic, J., Giallourou, N., Castro-Mejía, J. L., Hansen, L. H., … & Costabile, A. (2018). A prebiotic intervention study in children with autism spectrum disorders (ASDs). Microbiome, 6(1), 133.
- Hyman, S. L., Stewart, P. A., Schmidt, B., Cain, U., Lemcke, N., Foley, J. T., … & Ng, P. K. (2012). Nutrient intake from food in children with autism. Pediatrics, 130(Supplement 2), S145-S153.
- Levy, S. E., & Hyman, S. L. (2015). Complementary and alternative medicine treatments for children with autism spectrum disorders. Child and Adolescent Psychiatric Clinics, 24(1), 117-143.
- Li, Q., & Zhou, J. M. (2016). The microbiota–gut–brain axis and its potential therapeutic role in autism spectrum disorder. Neuroscience, 324, 131-139.
- Liu, H., Zimmerman, A. W., & Singh, K. (2021). Antioxidant approaches for the treatment of autism spectrum disorder: What clinicians should know. Seminars in Pediatric Neurology, 38, 100898.
- Mazahery, H., Stonehouse, W., Delshad, M., Kruger, M. C., Conlon, C. A., Beck, K. L., & von Hurst, P. R. (2017). Relationship between long chain n-3 polyunsaturated fatty acids and autism spectrum disorder: systematic review and meta-analysis of case-control and randomised controlled trials. Nutrients, 9(2), 155.
- Müller, E., Schuler, A., & Yates, G. B. (2008). Social challenges and supports from the perspective of individuals with Asperger syndrome and other autism spectrum disabilities. Autism, 12(2), 173-190.
- Sathe, N., Andrews, J. C., McPheeters, M. L., & Warren, Z. E. (2017). Nutritional and dietary interventions for autism spectrum disorder: a systematic review. Pediatrics, 139(6), e20170346.
- Sanctuary, M. R., Kain, J. N., Angkustsiri, K., & German, J. B. (2018). Dietary considerations in autism spectrum disorders: the potential role of protein digestion and microbial putrefaction in the gut-brain axis. Frontiers in Nutrition, 5, 40.
- Whiteley, P., Shattock, P., Knivsberg, A. M., Seim, A., Reichelt, K. L., Todd, L., … & Hooper, M. (2013). Gluten-and casein-free dietary intervention for autism spectrum conditions. Frontiers in Human Neuroscience, 6, 344.
- Woo, C. C., & Leon, M. (2013). Environmental enrichment as an effective treatment for autism: a randomized controlled trial. Behavioral Neuroscience, 127(4), 487.


















0 Comments