Executive Summary: The Neurobiology of Nutrition
The Core Question: Can diet cure depression? While “cure” is a strong word, clinical trials (like the SMILES trial) confirm that diet is a foundational treatment for major depressive disorder. Food is not just fuel; it is information for the brain.
Key Biological Mechanisms:
- The Psychobiotic Revolution: The gut microbiome produces 95% of the body’s serotonin. Dysbiosis (bacterial imbalance) leads to a deficit in mood-regulating chemicals.
- The Vagus Nerve: This cranial nerve acts as a bidirectional “fiber optic cable,” transmitting inflammatory signals from a “Leaky Gut” directly to the brain, causing “Sickness Behavior” (lethargy, anhedonia).
- Inflammation Theory: Modern psychiatry increasingly views depression as an inflammatory disease. An anti-inflammatory diet can downregulate the cytokines responsible for depressive symptoms.
Key Studies Cited: The SMILES Trial (Jacka et al.); Cryan & Dinan on Psychobiotics; Felice Jacka on Nutritional Psychiatry.
Can Diet Cure Depression? The Gut-Brain Axis and the Inflammation Theory of Mental Health

For decades, psychiatry treated the head as if it were detached from the body. If you were depressed, it was a “chemical imbalance” in the brain. Today, the frontier of mental health has moved south—to the gut.
The Gut-Brain Axis is the biochemical superhighway connecting your digestive tract and your central nervous system (CNS). Emerging research in Nutritional Psychiatry suggests that what we eat dictates how we feel, not just because of blood sugar, but because our microbiome essentially “programs” our neurotransmitters. This article explores the hard science behind why a salad might be as important as an antidepressant.
Part I: Anatomy of the Connection
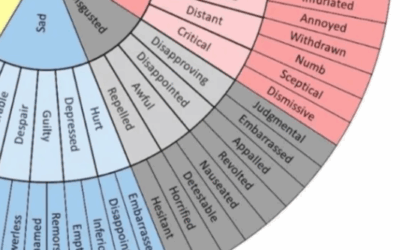
The connection between your stomach and your mood is mediated by three primary pathways: the Nervous System, the Immune System, and the Endocrine System.
1. The Vagus Nerve: The Neural Superhighway
The Vagus Nerve (Cranial Nerve X) is the longest nerve in the autonomic nervous system. It wanders from the brainstem down to the colon. Crucially, 80-90% of its fibers are afferent—meaning they carry signals from the gut to the brain, not the other way around.
When the gut is inflamed, the Vagus nerve detects this danger and sends an “alarm” signal to the brainstem, triggering anxiety and hypervigilance. Therapies like Somatic Experiencing and Brainspotting often work by toning this nerve to shut down the stress response.
2. The Enteric Nervous System (The “Second Brain”)
Your gut lining contains 500 million neurons—more than in the spinal cord. This is the Enteric Nervous System (ENS). It operates independently of the brain (you digest food even in a coma). The ENS produces a vast array of neurotransmitters, including Dopamine, GABA, and Serotonin. If the ENS is irritated by processed food, it sends “panic” signals to the primary brain.
Part II: The Microbiome and “Psychobiotics”
You are not a single organism; you are a colony. The human gut hosts trillions of bacteria, weighing about 4 pounds (the same weight as the brain). This microbiome is an active organ that metabolizes food into psychoactive chemicals.
The Serotonin Factory
Approximately 95% of the body’s Serotonin is produced in the gut, not the brain. Gut bacteria (like Candida, Streptococcus, Escherichia, and Enterococcus) manufacture this “happiness molecule” from the amino acid Tryptophan.
If you have Dysbiosis (an imbalance of bad bacteria vs. good bacteria), serotonin production plummets. This is why SSRIs (antidepressants) often cause digestive side effects—the receptors they target are mostly in your intestines.
The GABA Producers
Certain strains of bacteria, specifically Lactobacillus and Bifidobacterium (found in yogurt and fermented foods), secrete GABA—the brain’s primary inhibitory (calming) neurotransmitter. A deficit in these bacteria is directly linked to Generalized Anxiety Disorder.
Part III: The Inflammation Theory of Depression
The most compelling evidence for diet curing depression comes from the Cytokine Model of Depression.
Leaky Gut = Leaky Brain
A diet high in sugar and processed fats damages the intestinal lining (epithelium). This creates “Leaky Gut” (Intestinal Permeability), allowing toxins (lipopolysaccharides) to leak into the bloodstream.
The immune system attacks these toxins, releasing inflammatory markers called Cytokines. These Cytokines can cross the Blood-Brain Barrier. Once in the brain, they attack the neurons in the amygdala and hippocampus, causing neuro-inflammation.
“Sickness Behavior” vs. Depression
When you have the flu, you feel tired, antisocial, achy, and sad. This is “Sickness Behavior,” an evolutionary mechanism to keep you still so you can heal.
Key Insight: Chronic inflammation from a poor diet tricks the brain into a permanent state of “Sickness Behavior.” We diagnose this as **Major Depression**. The symptoms are identical: lethargy, brain fog, and withdrawal.
Part IV: The Evidence – The SMILES Trial
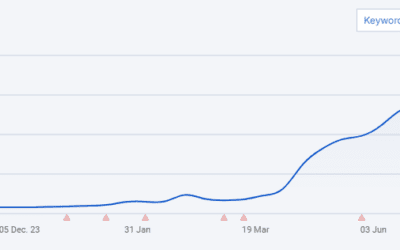
Is this just theory? No. In 2017, the SMILES Trial (Jacka et al.) provided the first randomized controlled clinical trial data.
Researchers took patients with moderate-to-severe depression and put half of them on a “Modified Mediterranean Diet” (high in veggies, fruits, whole grains, oily fish, extra virgin olive oil).
The Result: After 12 weeks, 32% of the diet group achieved full remission from depression, compared to only 8% of the social support control group. The better they ate, the more their depression lifted.
Part V: Brain-Based Medicine & Integrative Therapies
At Taproot Therapy Collective, we integrate nutritional psychology with neurobiological interventions.
1. QEEG Brain Mapping & Neurofeedback
We can see the effects of inflammation in a QEEG Brain Map. Inflamed brains often show excessive “Delta” or “Theta” waves (brain fog) or high “High Beta” (anxiety). Neurofeedback trains the brain to regulate these states, but diet provides the raw materials for the repair.
2. Vagus Nerve Stimulation
Since the Vagus nerve connects the gut and brain, stimulating it can reduce inflammation. Techniques used in Somatic Experiencing and deep diaphragmatic breathing manually activate the Vagus nerve, telling the gut to turn off the inflammatory response.
3. Ancestral Trauma & Epigenetics
Sometimes gut issues are inherited. Epigenetic studies show that stress in parents can alter the microbiome of their offspring. Therapies like Lifespan Integration help resolve the trauma timeline, reducing the stress signals that perpetuate gut dysfunction.
Conclusion: Food as Medicine
Can diet cure depression? For many, diet is the missing link that allows therapy and medication to finally work. You cannot medicate your way out of a bad diet, just as you cannot talk your way out of systemic inflammation.
By treating the gut, we treat the brain. By feeding the microbiome, we feed the mind.
Explore Integrative Treatments
Taproot Therapy Collective Podcast
Somatic & Brain Therapies
QEEG Brain Mapping: See Your Inflammation
Neurofeedback: Training the Inflamed Brain
Somatic Experiencing: The Vagus Nerve
ETT: Light Therapy for Regulation
Trauma & The Body
Lifespan Integration: Healing the Timeline
Scientific Bibliography
- Jacka, F. N., et al. (2017). A randomised controlled trial of dietary improvement for adults with major depression (the ‘SMILES’ trial). BMC Medicine.
- Dinan, T. G., & Cryan, J. F. (2013). Psychobiotics: A Novel Class of Psychotropic. Biological Psychiatry.
- Maes, M. (1995). Evidence for an Immune Response in Major Depression. Progress in Neuro-Psychopharmacology.
- Porges, S. W. (2011). The Polyvagal Theory: Neurophysiological Foundations of Emotions, Attachment, Communication, and Self-regulation. Norton.

















0 Comments