Key Takeaways: Compassion Fatigue & Physician Burnout
- Differential Diagnosis: Distinguishes between Burnout (bureaucratic exhaustion), Compassion Fatigue (emotional depletion from empathy), and Moral Injury (violation of ethical values).
- Neurobiology: Explains how the brain’s “mirror neuron” system can lead to secondary trauma in healthcare providers.
- Recovery Protocols: Moves beyond “self-care” to evidence-based therapies like Brainspotting and Somatic Experiencing to discharge stored trauma.
- Systemic Reality: Acknowledges that physician burnout is often a structural issue, not a personal failure of resilience.

The Cost of Caring: A Clinical Guide to Overcoming Compassion Fatigue and Physician Burnout
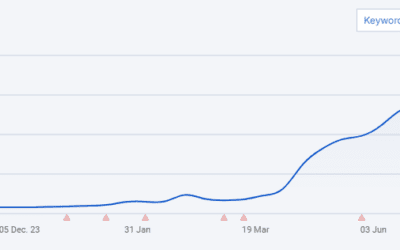
The image of the stoic, tireless healer is a dangerous myth. In the modern healthcare landscape, providers are facing an epidemic that goes far beyond “stress.” Compassion fatigue and secondary trauma are having a profound impact on the well-being and effectiveness of healthcare professionals. When healthcare workers are emotionally depleted and struggling with the weight of their experiences, it affects their ability to provide high-quality patient care and maintain their own sanity.
This guide dives deep into the anatomy of this silent crisis, exploring the difference between burnout and moral injury, the neuroscience of empathy, and practical, depth-psychology-based strategies for recovery.
We Have a Clinician who Treats Physician Burnout at Taproot Therapy Collective – Click Here
Part 1: The Diagnosis – Burnout, Compassion Fatigue, or Moral Injury?
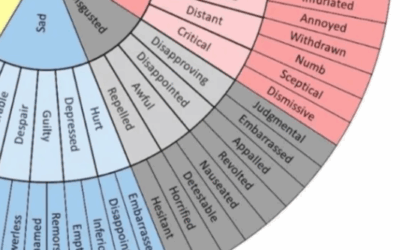
In clinical practice, these terms are often used interchangeably, but they represent distinct phenomena. Understanding which one you are suffering from is the first step toward treatment.
| Condition | Definition | Clinical Presentation |
| Burnout | Exhaustion caused by excessive demands on energy, strength, and resources. Usually driven by bureaucratic stressors (EHRs, insurance denials). | Cynicism, depersonalization, feeling “hollow,” reduced professional efficacy. |
| Compassion Fatigue | The emotional residue or strain of exposure to working with those suffering from the consequences of traumatic events. Often called “Secondary Traumatic Stress.” | Hyper-vigilance, intrusive thoughts about patients, inability to feel empathy (numbness), nightmares. |
| Moral Injury | The psychological distress that results from actions, or the lack of them, which violate one’s moral or ethical code. | Guilt, shame, spiritual crisis, anger at the “system” or administration. Feeling betrayed by leadership. |
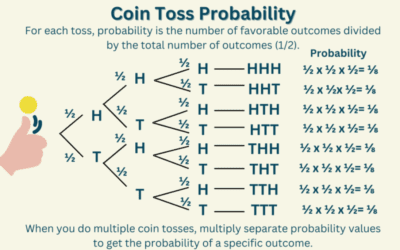
The Neurobiology of Empathy: Why it Hurts
Why does caring hurt? Humans are wired with Mirror Neurons. When you witness a patient in pain, your brain lights up in the same regions as if you were in pain. This is the biological basis of empathy. However, without adequate recovery time, the brain’s “pain matrix” remains activated.
Over time, the brain protects itself by shutting down. This leads to the hallmark symptom of compassion fatigue: Dissociation. The provider becomes detached, cold, or cynical, not because they don’t care, but because their nervous system has blown a fuse to prevent overheating. This relates closely to Allan Schore’s work on interpersonal neurobiology and the limits of emotional regulation.
Part 2: The Consequences of the “Hero” Complex
The medical culture often reinforces the Hero Archetype—the idea that the doctor must be invincible. This persona prevents providers from seeking help.
Impact on Patient Care
Emotionally exhausted healthcare professionals struggle to maintain empathy. They may become more detached, less attentive, and less responsive to patients’ needs. This deterioration leads to:
- Increased Medical Errors: Cognitive load from unprocessed trauma reduces executive function.
- Decreased Patient Safety: Distracted providers are more prone to oversights.
- Loss of Trust: Patients feel the provider’s detachment as rejection.
The Personal Toll
On a personal level, the constant exposure to suffering can lead to symptoms indistinguishable from PTSD. Healthcare workers may struggle with sleep disturbances, changes in appetite, and physical exhaustion. In severe cases, this can lead to the “Death Drive” or passive suicidality, a concept explored in Freud’s Death Drive.
Part 3: Evidence-Based Recovery Protocols
Healing from compassion fatigue requires more than a vacation. It requires a restructuring of how the provider relates to their work and their own nervous system.
1. Somatic Therapies: Discharging the Trauma
Talk therapy is often insufficient because trauma resides in the brainstem, not the prefrontal cortex. Somatic Experiencing helps providers physically “discharge” the freeze response accumulated after traumatic codes or difficult diagnoses. By tracking bodily sensations, the provider can complete the stress cycle.
2. Brainspotting for Visual Trauma
Healthcare providers often carry haunting visual memories (e.g., a traumatic injury in the ER). Brainspotting is a powerful tool that uses eye position to access the subcortical brain, allowing these “stuck” images to be processed and integrated without re-traumatizing the clinician.
3. The “Wounded Healer” and Jungian Analysis
From a Jungian perspective, many doctors are possessed by the archetype of the Healer. Jungian Therapy helps providers integrate their own “Wounded” side. Recognizing one’s own vulnerability is not a weakness; it is the bridge to authentic connection. Dealing with the Shadow—the parts of ourselves we reject (like our exhaustion or resentment)—is crucial to preventing burnout.
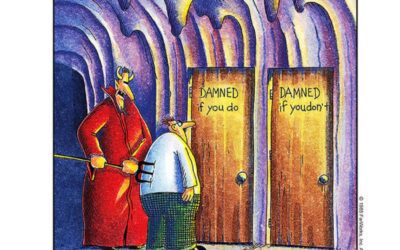
4. Systemic Awareness and Boundaries
Sometimes, the abuse comes from the system itself. Administrators who prioritize profit over patient care can enact a form of institutional abuse. Recognizing that the problem is systemic (Moral Injury) rather than personal (Resilience) shifts the blame off the provider. Setting boundaries becomes a political and therapeutic act.
Part 4: Creating a Culture of Resilience
Addressing the emotional toll of healthcare professions requires a multi-faceted approach that involves both individual and systemic interventions.
- Peer Support Groups: Creating spaces where “dark humor” and grief can be shared without judgment.
- Debriefing Protocols: Moving beyond the medical facts of a case to debrief the emotional impact of a death or error.
- Neurofeedback: Using QEEG Brain Mapping to identify and train the brain out of hyper-arousal states common in high-stress specialties like Surgery or Emergency Medicine.
Conclusion: From Surviving to Thriving
The cost of caring is high, but it should not cost you your soul. By acknowledging the biological reality of compassion fatigue and distinguishing it from systemic moral injury, healthcare providers can stop blaming themselves for their exhaustion.
Whether through mindfulness practices, deep somatic work, or simply allowing oneself to grieve, the path to recovery involves reclaiming the humanity that the medical system often tries to strip away. As you care for others, remember that you, too, are a patient worthy of care.
Explore Depth Psychology for Healers
Taproot Therapy Collective Podcast
Trauma & Somatic Treatments
- Somatic Experiencing: Healing trauma through the body’s natural release mechanisms.
- Brainspotting: Accessing deep brain trauma through eye positioning.
- EMDR: Processing traumatic memories.
- Somatic Trauma Mapping: Locating where stress lives in the body.
- Lifespan Integration: Healing the timeline of trauma.
Psychological Frameworks
- Personality Psychology: Understanding the traits that lead to the medical profession.
- The Hero’s Journey: Navigating the cycle of call, struggle, and return.
- The Shadow: Confronting the hidden costs of being a “helper.”
- Abraham Maslow: Moving toward self-actualization beyond burnout.
Bibliography
- Figley, C. R. (2002). Compassion fatigue: Psychotherapists’ chronic lack of self care. Journal of clinical psychology.
- Shanafelt, T. D., et al. (2012). Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Archives of internal medicine.
- Dean, W., & Talbot, S. G. (2019). Moral injury and burnout in medicine: A year of lessons learned.
- Kluczewska, E., et al. (2020). The Neurobiology of Compassion Fatigue: A Review.
- Van der Kolk, B. A. (2014). The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma. Viking.
Disclaimer: This article is for educational purposes only and does not constitute medical advice or professional supervision. If you are in crisis, please contact a mental health professional or emergency services.
















0 Comments