A War Within Your Own Mind?
For many, the mind is a sanctuary. But for some, it becomes a battlefield. Imagine being trapped in a relentless, internal war against your own thoughts—thoughts that feel alien, dangerous, and deeply shameful. These are not fleeting worries; they are intrusive, recurring images, urges, or ideas that scream in direct opposition to who you are and what you value. This is the isolating and often terrifying experience for individuals grappling with a form of Obsessive-Compulsive Disorder (OCD) colloquially known as “Pure O”.1
Many people find this term when searching for answers, desperately trying to name the experience of having intense, disturbing obsessions without the visible, external compulsions—like hand-washing or checking—that are commonly associated with OCD.1 They feel they are “purely obsessional.” However, this report will establish a critical and ultimately more hopeful framework: “Pure O” is a deeply misleading term. The struggle is not merely one of obsessions. It is a full presentation of OCD where the compulsions are simply hidden from view, executed as covert rituals within the mind.3 Understanding this distinction is the first and most crucial step toward effective treatment and reclaiming one’s life from this unseen struggle.
What is “Pure O”? Debunking a Common and Painful Myth
Defining “Purely Obsessional” OCD
“Pure O,” or Purely Obsessional OCD, is a widely used term to describe a form of OCD where an individual experiences intrusive, distressing thoughts, images, or urges (obsessions) and engages primarily in mental, rather than visible, compulsions to manage the resulting anxiety.1 It is essential to clarify that “Pure O” is not a formal clinical diagnosis recognized in the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5), the standard classification used by mental health professionals.3 Instead, it is a descriptive label that captures the subjective experience of those whose compulsions are internal and hidden.
The Critical Flaw in the “Pure O” Label
The term “Pure O” persists because it resonates so strongly with the sufferer’s internal reality: a feeling of being tormented by thoughts alone. This makes the term a common gateway, allowing individuals to find information and a community that understands their invisible battle.7 However, this same term can become a significant barrier to recovery. The core misconception is that these individuals have obsessions without compulsions. Multiple research studies have demonstrated that this is almost never the case. When clinicians conduct careful assessments, they find that individuals who appear to have only obsessions are, in fact, performing a variety of covert mental compulsions and subtle reassurance-seeking behaviors.3
This makes the “Pure O” label not only inaccurate but also “misleading and unhelpful,” as it may prevent individuals—and sometimes even untrained clinicians—from identifying the very compulsions that must be addressed for treatment to be effective.3 Recovery from OCD hinges on targeting and stopping compulsions; if they are not recognized, the path to healing remains obscured.
The OCD Cycle in Pure O: An Internal Loop
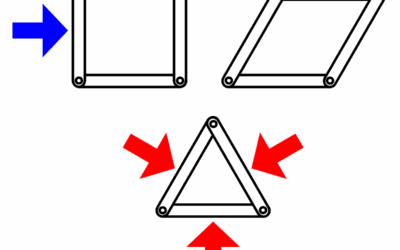
All forms of OCD are driven by the same vicious cycle: an obsession triggers intense anxiety, which leads to a compulsion, resulting in temporary relief.5 This cycle is identical in the so-called “Pure O” presentation, but the compulsive and relief-seeking steps happen almost entirely within the mind.5
- Obsession: An unwanted, intrusive thought, image, or urge enters the mind (e.g., “What if I swerve my car into oncoming traffic?”).
- Anxiety/Distress: The obsession causes a spike in anxiety, fear, guilt, or disgust because it feels so real and threatening.
- Mental Compulsion: To neutralize the anxiety, the individual performs a covert mental ritual (e.g., mentally reviewing their driving history to “prove” they are a safe driver, silently repeating a “safe” phrase, or mentally “undoing” the bad thought with a good one).
- Temporary Relief: The mental compulsion provides a fleeting sense of relief or certainty, but this relief is short-lived. By engaging in the ritual, the brain learns that the obsession was a genuine threat that was narrowly averted, thus strengthening the connection between the obsession and the compulsion and making the cycle more powerful the next time it occurs.
Reframing the experience from a mysterious thought disorder to this known, treatable OCD pattern is a foundational shift that opens the door to proven therapeutic strategies.
Inside the Mind: Common Themes and Covert Compulsions
The Nature of Intrusive Thoughts
It is a fundamental aspect of the human condition to experience thousands of thoughts each day, many of which are random, strange, or nonsensical.10 Intrusive thoughts are a normal part of this mental chatter. The critical difference in OCD is the meaning and distress attached to them. For someone with OCD, an intrusive thought is experienced as “ego-dystonic”—it is repulsive, distressing, and fundamentally at odds with their true values, beliefs, and character.2 A gentle, loving parent may have an intrusive thought of harming their child; a devout person may have a blasphemous image flash through their mind.
This profound clash between the thought and the self is what generates the intense anxiety, guilt, and shame that fuel the disorder.1 The degree of horror a person feels in response to an intrusive thought is not an indicator of their hidden desires, but rather a direct measure of how deeply the thought violates their core values. The content of OCD is not a confession; it is an attack on what the individual holds most dear. This understanding is a crucial diagnostic clue that helps differentiate OCD from psychotic disorders, where intrusive thoughts are often “ego-syntonic” and believed to be real.6
Common Obsessional Themes
Because the obsessions in Pure O are often ego-dystonic and related to taboo subjects, sufferers are frequently terrified of sharing them for fear of being judged, misunderstood, or even incriminated.5 Some of the most common themes include:
- Harm OCD: Persistent fears of losing control and violently harming oneself or others. This can manifest as intrusive images of stabbing a loved one, pushing a stranger in front of a train, or driving a car into a crowd.1
- Sexual OCD: Unwanted and disturbing sexual thoughts, images, or urges. These often involve socially taboo subjects, leading to fears that one might be a pedophile (POCD), is attracted to family members, or is in denial about their sexual orientation (SO-OCD).1
- Relationship OCD (R-OCD): Constant, pervasive doubts about the “rightness” of a relationship, the suitability of a partner, or the authenticity of one’s own feelings of love. Sufferers may endlessly analyze their partner’s flaws or monitor their own feelings for proof of their commitment.1
- Moral/Religious Scrupulosity: An obsessive preoccupation with being a “bad” or immoral person. This can involve extreme guilt over minor past mistakes, a fear of violating religious doctrines, or a terror of committing blasphemy.7
- Existential OCD: Obsessive and unresolvable questioning about the nature of reality, the meaning of life, or the universe. These philosophical concerns become a source of profound and paralyzing anxiety.7
Unmasking the Mental Rituals
The key to understanding and treating Pure O is to unmask the hidden compulsions. These are not passive worries; they are active, intentional mental behaviors performed to reduce distress.7 Common mental rituals include:
- Mental Reviewing/Analysis: Compulsively scanning past memories to check for evidence related to a fear. For example, a person with Harm OCD might mentally replay a time they used a kitchen knife to ensure they didn’t accidentally hurt anyone.3
- Neutralizing: Actively trying to cancel out a “bad” thought, image, or feeling with a “good” or “safe” one. This can involve mentally repeating a specific prayer, phrase, or positive image immediately after an intrusive thought occurs.3
- Rumination: Engaging in a prolonged, circular, and unproductive internal debate in an attempt to “solve” or “figure out” an obsessive doubt. Unlike productive problem-solving, OCD rumination never leads to a satisfying conclusion and only serves to deepen the obsession.5
- Reassurance-Seeking: This can be internal (e.g., repeatedly telling oneself, “I am a good person, I would never do that”) or external (e.g., repeatedly asking a partner, “Do you think I’m a good person?” or “Do you still love me?”). It also includes excessive online research to find definitive answers to one’s fears.1
- Thought Monitoring: A state of hypervigilance where the individual constantly scans their own mind and body for the presence or absence of certain thoughts, feelings, or physical sensations (e.g., checking for feelings of sexual arousal in a triggering situation).9
- Avoidance: While a behavioral compulsion, it is often subtle and directly linked to the mental obsessions. This includes avoiding people, places, objects, or media (e.g., news stories, movies) that could trigger an intrusive thought.1
The following table illustrates the direct link between common obsessions and their corresponding mental compulsions, making the invisible process more concrete.
| Theme | Example Obsession (Intrusive Thought) | Common Mental Compulsions (Covert Rituals) |
| Harm OCD | “What if I lose control and stab my partner while cooking dinner?” | – Mentally reviewing every past instance of using a knife to “prove” safety. – Silently repeating “I love my partner” to neutralize the thought. – Avoiding being in the kitchen with the partner. |
| Sexual OCD (POCD) | An unwanted sexual image of a child enters the mind, followed by “Does this mean I’m a pedophile?” | – Mentally checking one’s body for any sign of physical arousal. – Ruminating for hours on the definition of pedophilia. – Mentally reviewing all past interactions with children for “evidence.” |
| Relationship OCD | “What if I don’t really love my partner? Am I lying to them?” | – Constantly “checking” one’s feelings for the presence of love. – Mentally comparing one’s relationship to others. – Seeking reassurance by asking the partner, “Are we okay?” |
| Scrupulosity | “I had a blasphemous thought about God. Does this mean I’m going to hell?” | – Repetitive, compulsive prayer to atone for the thought. – Mentally reviewing past actions to see if they were sinful. – Seeking reassurance from a religious authority figure. |
An Informal Screener for Purely Obsessional OCD
Disclaimer: This is an informal screener based on common symptoms of Purely Obsessional OCD. It is not a diagnostic tool and cannot replace a formal evaluation by a qualified mental health professional. The purpose of this screener is to serve as an educational resource to help you explore your experiences and decide if seeking professional advice is the right next step. While this tool is informed by clinical research and evidence, your score is simply an indicator, not a diagnosis.
Instructions
Read each statement below carefully. For each one, consider how much it has bothered or distressed you over the past month. Rate each statement on the following scale:
- 0 – Not at all
- 1 – A little
- 2 – Moderately
- 3 – A lot
- 4 – Extremely
Record the number that best reflects your experience for each question.
The Screener
Part A: Intrusive Thoughts & Distress
- I am upset by unwanted, nasty, or frightening thoughts that come into my mind against my will.
- I find it difficult to control my own thoughts, no matter how hard I try.
- The content of my unwanted thoughts feels shameful, immoral, or dangerous.
- I worry that my thoughts mean something terrible about my character or future actions.
- These intrusive thoughts cause me significant anxiety or distress.
Part B: Mental Reviewing & Analysis
- I mentally replay past conversations or events to check if I made a mistake or did something wrong.
- I spend a significant amount of time trying to “figure out” the “true meaning” of my thoughts.
- I analyze my memories in great detail to prove to myself that a feared event did not happen.
- I get stuck in my head, going over and over a particular doubt or worry without reaching a conclusion.
- I mentally scan my past for evidence to confirm or deny a fear about my identity (e.g., my sexuality, morality).
Part C: Neutralizing & Mental Rituals
- I feel the need to repeat a “good” or “safe” word, phrase, or prayer in my head to cancel out a “bad” thought.
- I feel compelled to count silently or perform other mental patterns to reduce anxiety or prevent a bad event.
- I try to replace an upsetting mental image with a specific “calming” or “correct” one.
- I have superstitious thoughts that if I don’t think or do something in a certain way, something terrible will happen.
- I feel a strong urge to mentally “undo” or “take back” a thought that feels wrong or dangerous.
Part D: Reassurance & Certainty Seeking
- I mentally argue with myself, trying to prove with 100% certainty that my fears won’t come true.
- I repeatedly ask others for reassurance about my fears (e.g., “Are you sure I didn’t hurt anyone?”).
- I find myself researching my symptoms or fears online for hours, looking for a definitive answer.
- I mentally tell myself over and over that “everything is okay” or “I would never do that” to calm myself down.
- I feel an overwhelming need for certainty about things that are inherently uncertain.
Part E: Avoidance & Monitoring
- I avoid certain people, places, or media (TV shows, news) because I’m afraid they will trigger my unwanted thoughts.
- I constantly “check” my feelings or physical sensations to see if they align with my fears (e.g., checking for arousal, anger, or anxiety).
- I try to suppress or push away unwanted thoughts, only to find they come back stronger.
- I put off making decisions because I’m afraid of making the “wrong” one.
- I monitor my own mind to make sure I am not having a particular “bad” thought.
Part F: Impact on Life
- My internal struggles with thoughts and mental rituals take up more than one hour per day.
- I feel intense shame, guilt, or frustration about the content of my thoughts.
- My preoccupation with these thoughts makes it difficult to concentrate on work, school, or conversations.
- My relationships have been negatively affected by my internal distress or reassurance-seeking.
- These mental battles have significantly reduced my overall quality of life or ability to enjoy things.
Scoring and Interpretation
Add up the numbers you recorded for all 30 questions to get your total score.
- Total Score Range: 0 – 120
This score is not a diagnosis. It is a reflection of the level of distress you reported in relation to common experiences of Purely Obsessional OCD. A higher score may suggest that the patterns of thinking and mental rituals described in this screener are causing a significant impact on your life. If you are concerned about your score or if these experiences resonate with you, it may be beneficial to share these results with a licensed mental health professional who specializes in the treatment of OCD.
The Path to Recovery: Evidence-Based Treatments for Pure O
Recovery from Pure O is not only possible but probable with the right, specialized treatment. Because the disorder is entirely internal—an intrusive thought triggering a mental compulsion—the therapeutic approach must be skillfully adapted to this internal battlefield. A generic approach to therapy is unlikely to be effective; success requires a clinician with specific expertise in treating OCD with primarily mental compulsions.11
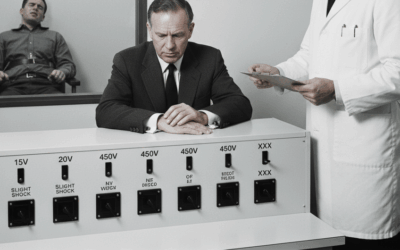
The Gold Standard: Exposure and Response Prevention (ERP)
Exposure and Response Prevention (ERP) is the first-line, evidence-based psychotherapy for all forms of OCD, with decades of research supporting its effectiveness. Approximately 80% of people with OCD experience significant symptom relief with ERP.5 ERP has two components:
- Exposure: Gradually and systematically confronting the thoughts, images, and situations that trigger obsessional fear.
- Response Prevention: Actively resisting the urge to perform the compulsive behaviors (in this case, mental rituals) that are typically used to reduce anxiety.
Adapting ERP for Pure O
For Pure O, where triggers are internal thoughts and compulsions are mental rituals, ERP is adapted in specific ways:
- Imaginal Exposure: This is the primary exposure tool. The therapist and client work together to create written scripts or audio recordings that detail the client’s feared scenarios in a vivid, present-tense narrative. The client then repeatedly listens to or reads these scripts, allowing the anxiety to rise without performing any compulsions.12 For example, a person with Harm OCD might listen to a script that says, “I am holding the knife, and the thought that I could harm my partner is in my mind. The feeling of anxiety is rising in my chest. I may or may not lose control. I am choosing to sit with this uncertainty.”
- Response Prevention for Mental Rituals: This is the most challenging but crucial part of treatment. It means making a conscious, deliberate choice to not engage in the mental rituals when an obsession is triggered. This involves:
- Dropping the mental review.
- Allowing the “bad” thought to be present without neutralizing it.
- Resisting the urge to ruminate and “figure it out.”
- Not providing oneself with mental reassurance.
Through this process, the brain undergoes a process called habituation, learning that the feared outcomes do not occur and that the anxiety, when not fought with compulsions, will naturally decrease on its own.14
A Powerful Ally: Acceptance and Commitment Therapy (ACT)
Acceptance and Commitment Therapy (ACT) is another evidence-based psychotherapy that is highly effective for OCD. It can be integrated with ERP to boost its effectiveness or used as a primary approach, particularly for individuals who find traditional ERP difficult.11 The goal of ACT is not to eliminate intrusive thoughts but to fundamentally change one’s relationship with them, thereby increasing psychological flexibility.16
Core Principles of ACT for Pure O
ACT teaches skills through its six core principles, which are perfectly suited for the internal nature of Pure O 17:
- Acceptance: Instead of fighting or suppressing thoughts, one learns to make room for them, allowing them to come and go without a struggle. This is like letting a beach ball you’ve been holding underwater pop up to the surface; it takes far less energy to let it float than to keep it submerged.18
- Cognitive Defusion: This involves learning to “unhook” from thoughts and see them for what they are: simply words and images generated by the mind, not literal truths or commands. A common technique is to rephrase a thought like “I am a bad person” to “I am having the thought that I am a bad person”.13 Another powerful metaphor is to imagine thoughts as leaves floating down a stream; the goal is to sit on the bank and watch them pass by without having to jump in the water after them.18
- Being Present: Through mindfulness practices, individuals learn to anchor their attention in the present moment, rather than being lost in ruminations about the past or catastrophic worries about the future.
- Self-as-Context: This principle helps individuals realize that they are not their thoughts, feelings, or experiences. They are the stable, observing “sky” in which the “weather” of their thoughts and emotions passes through.
- Values: ACT helps individuals clarify what is truly important to them in life—their core values, such as connection, compassion, creativity, or growth.
- Committed Action: This is the process of setting goals and taking concrete actions that are guided by one’s values, even in the presence of anxiety and intrusive thoughts. The question shifts from “How do I get rid of this anxiety?” to “What truly matters to me, and what small step can I take in that direction right now?”
The Role of Medication in Treatment
For many individuals, medication is a crucial component of an effective treatment plan, often used in conjunction with therapy.
- First-Line Medications: The most well-researched and effective medications for OCD are a class of antidepressants called Selective Serotonin Reuptake Inhibitors (SSRIs). These include fluoxetine, sertraline, fluvoxamine, and others. The tricyclic antidepressant Clomipramine is also a highly effective first-line option.11
- Key Considerations: It is important to note that treating OCD with these medications typically requires higher doses and a longer trial period (8-12 weeks or more) than when treating depression.22 It is vital to work with a psychiatrist or other qualified prescriber who has experience treating OCD.
- Adjunctive Medications: For individuals who do not respond fully to a first-line medication, a prescriber may recommend an augmentation strategy. This involves adding another type of medication, such as a low dose of an atypical antipsychotic (e.g., Risperidone, Aripiprazole), to enhance the effects of the primary medication.22
Finding Help and Further Resources
Taking the first step toward getting help can be daunting, but it is the most important one. Recovery is possible, and there are excellent resources available to guide the way.
Finding the Right Therapist
When seeking a therapist, it is critical to find someone with specialized training in treating OCD. General talk therapy that is not tailored for OCD can be unhelpful or even worsen symptoms.14 Look for clinicians who explicitly state that they specialize in OCD and use Exposure and Response Prevention (ERP). Many skilled OCD therapists also integrate Acceptance and Commitment Therapy (ACT) into their practice.
Key Organizations
The following non-profit organizations are dedicated to providing accurate information, support, and resources for individuals with OCD and their families.
- International OCD Foundation (IOCDF): The IOCDF is the premier global resource for the OCD community. Their website offers comprehensive information about all forms of OCD, hosts conferences, funds research, and provides a crucial Treatment Provider Directory to help individuals find qualified specialists in their area.14
- Anxiety & Depression Association of America (ADAA): The ADAA is another reputable organization that provides education, resources, and support for individuals living with anxiety, depression, and co-occurring disorders like OCD.26
- National Institute of Mental Health (NIMH): As part of the U.S. National Institutes of Health, the NIMH is an authoritative source for the latest research-backed information on the causes, symptoms, and treatments for OCD.28
Self-Help and Support
While not a substitute for professional therapy, self-help resources and peer support can be invaluable complements to treatment. Joining a support group, either in-person or online, can reduce feelings of isolation by connecting individuals with others who truly understand the struggle.29 Additionally, workbooks based on ERP and ACT, such as The Mindfulness Workbook for OCD, can provide structured exercises to practice therapeutic skills between sessions.11
Reclaiming Your Mind and Your Life
Living with Purely Obsessional OCD can feel like being held captive by your own mind. The constant barrage of intrusive thoughts and the exhausting mental rituals performed in secret can shrink one’s world, creating a life governed by fear, shame, and doubt. However, there is a clear and well-researched path to freedom.
The journey begins with a crucial shift in understanding: “Pure O” is not a life sentence of uncontrollable thoughts. It is a treatable form of OCD, defined not by an absence of compulsions, but by compulsions that are mental. The disturbing content of these obsessions is a symptom of a neurological disorder, not a reflection of one’s true character or desires. With evidence-based treatments like Exposure and Response Prevention and Acceptance and Commitment Therapy, it is possible to learn to relate to these thoughts differently, to stop fueling them with mental rituals, and to reclaim the mental space they once occupied. Recovery means learning to live with uncertainty, to act in accordance with your values, and to build a life that is rich and meaningful, not in the absence of intrusive thoughts, but in spite of them.
Cited Sources and Resources:
- Aafjes-van Doorn, K., Békés, V., Prout, T. A., & Hoffman, L. (2014). The role of attachment in the clinical process: An empirical-clinical perspective. Psychoanalytic Psychology, 31(4), 488–503.
- Abramowitz, J. S., Deacon, B. J., Woods, C. M., & Tolin, D. F. (2003). Association between obsessive-compulsive symptom dimensions and implicit anxiety. Behaviour Research and Therapy, 41(10), 1249-1261.
- Anxiety and Depression Association of America (ADAA). (n.d.). Obsessive-Compulsive Disorder (OCD).
- Becker, E. (1973). The denial of death. Free Press.
- Brose-Dierkes, A., Brose, A., & Schmied, G. (2019). Mindfulness-based interventions for obsessive-compulsive disorder: A systematic review. Journal of Obsessive-Compulsive and Related Disorders, 22, 100448.
- Fineberg, N. A., & Sahakian, B. J. (2021). Obsessive-compulsive disorder: A clinical and neurobiological perspective. Oxford University Press.
- Healthline. (n.d.). Pure O OCD.
- Hillman, J. (1975). Re-visioning psychology. Harper & Row.
- Hollis, J. (2013). The middle passage: From misery to meaning in midlife. Inner City Books.
- Institute of Living. (2016). Obsessive-Compulsive Disorder (OCD) Assessment Tool.
- International OCD Foundation (IOCDF). (n.d.). OCD Screener.
- International OCD Foundation (IOCDF). (n.d.). OCD Treatment Guide.
- Johns Hopkins Medicine. (n.d.). Obsessive-Compulsive Disorder (OCD).
- Jung, C. G. (1967). Collected works of C.G. Jung, Volume 7: Two essays on analytical psychology. Princeton University Press.
- May, R. (1977). The meaning of anxiety. W.W. Norton & Company.
- Mayo Clinic. (n.d.). Obsessive-compulsive disorder (OCD).
- MedlinePlus. (n.d.). Obsessive-Compulsive Disorder.
- Mind. (n.d.). Symptoms of OCD.
- Moulding, R., Anglim, J., Nedeljkovic, M., & Kyrios, M. (2014). The relationship between ego-dystonicity and obsessive-compulsive disorder symptoms. Journal of Clinical Psychology, 70(1), 1-11.
- National Institute of Mental Health (NIMH). (n.d.). Obsessive-Compulsive Disorder (OCD).
- NOCD. (n.d.). Pure OCD (purely obsessional OCD).
- Osborne, S. (2019). Ritual: An essential guide to creating meaningful ceremonies. Golden Notebook Press.
- Simply Psychology. (n.d.). ‘Pure O’ or ‘purely obsessional’ OCD.
- Stanford Medicine. (n.d.). Pharmacotherapy for OCD.
- Stein, D. J., Costa, D. L. C., Lochner, C., Miguel, E. C., Reddy, Y. C. J., Shavitt, R. G., van den Heuvel, O. A., & Simpson, H. B. (2019). Obsessive-compulsive disorder. Nature Reviews Disease Primers, 5(1), 52.
- Suzuki, D. T. (1966). Zen Buddhism: Selected writings of D.T. Suzuki. Doubleday.
- Talkspace. (n.d.). Obsessive-Compulsive Disorder Test.
- Whitehead, C., Jones, R., & Oliver, J. E. (2021). Metacognitive therapy for obsessive-compulsive disorder: A systematic review and meta-analysis. Journal of Anxiety Disorders, 77, 102334.
- Williams, M. T., Farris, S. G., Turkheimer, E., Pinto, A., Ozanick, K., Franklin, M. E., Simpson, H. B., & Foa, E. B. (2011). Myth of the pure obsessional: A study of obsessional-only obsessive-compulsive disorder. Depression and Anxiety, 28(6), 495-500.
- Williams, M. T., & Wetterneck, C. T. (2019). Cognitive-behavioral therapy for obsessive-compulsive disorder: A guide for professionals. Routledge.
- Woodman, M. (1998). The pregnant virgin: A process of psychological transformation. Inner City Books.

















0 Comments