The Role of Natural Supplements and Holistic Approaches
Oppositional Defiant Disorder (ODD) represents one of the most challenging behavioral conditions affecting children and adolescents today. Characterized by persistent patterns of angry, irritable mood, argumentative and defiant behavior, and vindictiveness toward authority figures, ODD can significantly impact a child’s development and family dynamics. While conventional treatments such as behavioral therapy and medication play crucial roles in management, growing interest in complementary approaches has led many families to explore natural alternatives, including nutritional supplements and holistic interventions.
Understanding the Nature of ODD
Oppositional Defiant Disorder is defined as a pattern of negativistic, hostile, and defiant behavior lasting at least six months. Children with ODD frequently lose their temper, argue with adults, actively defy rules, deliberately annoy others, blame others for their mistakes, and may display spiteful or vindictive behavior. These symptoms typically manifest in multiple settings, though they may be more pronounced at home or school.
According to the Cleveland Clinic, researchers estimate that ODD affects between 2% and 11% of children, with prevalence typically declining with increasing age. The symptoms usually begin by age 8 and often remain stable between ages 5 and 10 before potentially diminishing in adolescence. However, if left untreated, ODD can evolve into more serious conduct problems and potentially develop into conduct disorder in approximately 30% of cases.
The etiology of ODD appears multifaceted. Research suggests a complex interplay of genetic, biological, and environmental factors. Studies indicate that genetics may account for about 50% of ODD development, with many affected children having close family members with other mental health conditions. Neurobiological factors, including alterations in certain brain regions and neurotransmitter systems, likely play roles as well. Environmental factors such as inconsistent parenting, family dysfunction, and early traumatic experiences can further contribute to the development of oppositional behaviors.
Conventional Treatment Approaches
The foundation of ODD treatment typically involves psychosocial interventions. Parent Management Training (PMT) stands as the primary evidence-based treatment, demonstrating medium effect sizes in reducing antisocial behaviors. These programs focus on teaching parents to use positive reinforcement while implementing natural, non-violent consequences for behavior, ultimately improving parent-child communication.
Individual cognitive-behavioral therapy helps children develop problem-solving skills and anger management techniques. School-based interventions address behavioral issues in educational settings, while family therapy works to improve overall family dynamics. When these behavioral approaches prove insufficient, particularly in cases with comorbid conditions like ADHD, medication may be considered.
Pharmaceutical interventions for ODD often include stimulants like methylphenidate (Ritalin), particularly when ADHD coexists. Studies have shown that these medications can effectively reduce symptoms of both ADHD and ODD when they occur together. Low-dose atypical neuroleptics such as aripiprazole (Abilify) and risperidone (Risperdal) have also shown promise in improving oppositional behaviors, though they are not FDA-approved specifically for ODD. It’s worth noting that stimulants typically don’t reduce ODD symptoms when ADHD is absent, underscoring the importance of treating any underlying conditions.
The Emerging Role of Nutritional Supplements
As interest in complementary approaches grows, research has begun exploring the potential benefits of nutritional supplements for behavioral disorders like ODD. While specific studies focusing exclusively on ODD remain limited, evidence from related conditions such as ADHD, anxiety, and mood disorders provides valuable insights.
Omega-3 Fatty Acids
Omega-3 fatty acids, found in fatty fish, flaxseeds, and walnuts, have received significant attention for their potential role in brain development and function. These essential fatty acids form critical components of neural cell membranes and influence neurotransmitter systems. Research suggests potential benefits for children with behavioral problems, including reduced aggression and improved emotional regulation.
A systematic review published in the Journal of Child Psychology and Psychiatry found that omega-3 supplementation produced small but significant improvements in conduct problems and aggression in children with disruptive behavior disorders. The mechanisms may involve anti-inflammatory effects and optimization of neural signaling pathways important for mood regulation and impulse control.
Vitamin D
Emerging research has identified associations between vitamin D deficiency and various behavioral issues in children. This essential nutrient plays crucial roles in brain development and function, influencing neurotransmitter synthesis and nerve growth factors. A study in the Journal of Child Psychology and Psychiatry found that children with behavior problems had significantly lower vitamin D levels compared to controls, and supplementation was associated with modest improvements in conduct.
Considering the high prevalence of vitamin D insufficiency in many populations, particularly in regions with limited sun exposure, assessment and supplementation may represent a reasonable adjunctive approach for children with ODD.
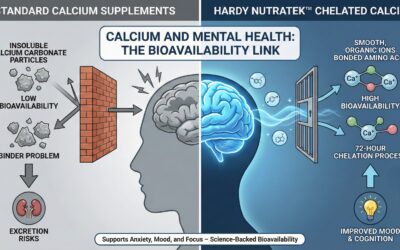
Magnesium
Magnesium deficiency has been linked to increased irritability, anxiety, and poor stress resilience—symptoms that often overlap with ODD presentation. This essential mineral regulates over 300 enzyme systems in the body and plays crucial roles in neurotransmitter release and stress response.
Research published in the journal Medical Hypotheses suggests that magnesium supplementation may help modulate the stress response and reduce irritability in children with behavioral problems. Given that many contemporary diets provide suboptimal magnesium levels, supplementation might benefit children with symptoms of irritability and poor emotional regulation.
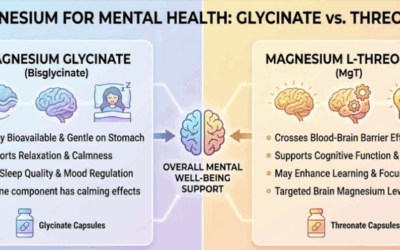
Zinc
Zinc plays essential roles in brain development and neurotransmitter regulation. Deficiencies have been associated with increased emotional liability and behavioral problems in children. A study in the Journal of Child and Adolescent Psychopharmacology found correlations between zinc deficiency and severity of conduct problems in children with disruptive behavior disorders.
Supplementation may be particularly beneficial in populations at risk for zinc deficiency or those consuming primarily plant-based diets, as plant sources contain less bioavailable forms of this mineral compared to animal foods.
B Complex Vitamins
B vitamins serve as essential cofactors in neurotransmitter synthesis pathways and energy production in brain cells. Deficiencies in various B vitamins have been linked to irritability, mood disturbances, and poor stress tolerance. A comprehensive review in Nutrients journal highlighted the importance of B vitamins for psychological functioning and stress resilience.
While specific research on B vitamins for ODD remains limited, their fundamental roles in brain function and mood regulation suggest potential benefits, particularly in children with suboptimal dietary patterns or increased stress responses.
Herbal Approaches with Potential Benefits
Several herbal remedies have demonstrated calming and mood-regulating effects that might benefit children with ODD, though research specifically for ODD remains preliminary.
L-Theanine
This amino acid found in green tea has been studied for its calming effects without sedation. Research in the Journal of Clinical Psychiatry demonstrated that L-theanine supplementation reduced anxiety symptoms and improved attention in children with ADHD. Its mechanisms involve increasing alpha brain wave activity associated with relaxed alertness and modulating inhibitory neurotransmitters.
For children with ODD who struggle with emotional regulation and impulsivity, L-theanine represents a potentially beneficial supplement with an excellent safety profile.
Lemon Balm (Melissa officinalis)
This gentle herb has been traditionally used for its calming properties and has shown anxiolytic effects in several clinical studies. A randomized controlled trial in the journal Phytomedicine found that lemon balm extract improved mood and cognitive performance while reducing stress-induced impairments.
For children with ODD who experience heightened stress responses and irritability, lemon balm might offer a gentle, natural option to support emotional regulation.
Chamomile (Matricaria recutita)
Long valued for its mild sedative and anti-anxiety properties, chamomile contains compounds that bind to GABA receptors, producing calming effects similar to pharmaceutical anxiolytics but with a milder profile. A study in the Journal of Clinical Psychopharmacology found chamomile extract produced modest improvements in symptoms of generalized anxiety disorder.
This gentle herb may benefit children with ODD who experience anxiety alongside their oppositional behaviors, potentially helping reduce the emotional arousal that often precedes defiant episodes.
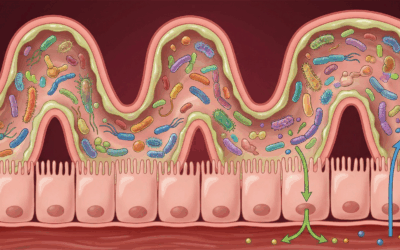
Gut-Brain Connection: The Microbiome Approach
Exciting developments in understanding the gut-brain axis have opened new avenues for addressing behavioral disorders. The gut microbiome communicates with the brain through multiple pathways, including the vagus nerve, immune signaling, and neurotransmitter production.
Probiotics
Research has demonstrated connections between gut microbiota composition and behavioral traits, including emotional regulation and stress response. A groundbreaking study in the journal Brain, Behavior, and Immunity found that specific probiotic strains improved mood and reduced inflammatory markers associated with anxiety and depression.
For children with ODD, particularly those with comorbid anxiety or mood symptoms, probiotics containing specific beneficial bacteria like Lactobacillus rhamnosus and Bifidobacterium longum may help modulate stress responses and support emotional regulation. These approaches may be especially relevant for children with histories of antibiotic use, digestive issues, or restricted dietary patterns.
Prebiotic Fibers
Prebiotic fibers serve as “food” for beneficial gut bacteria, potentially enhancing the growth of microbes that produce short-chain fatty acids with anti-inflammatory and neuroprotective effects. A study in Psychopharmacology found that prebiotic supplementation reduced stress hormone responses and improved emotional processing.
Foods rich in prebiotic fibers include garlic, onions, leeks, asparagus, bananas, and oats—making dietary approaches a practical way to support gut health in children with behavioral issues like ODD.
Dietary Patterns and Food Sensitivities
Beyond specific supplements, overall dietary patterns may significantly influence behavioral symptoms. Some research suggests that certain food components may exacerbate behavioral problems in susceptible children.
Elimination Diets
Elimination diets involve temporarily removing potentially problematic foods, then systematically reintroducing them while monitoring behavioral responses. Research published in The Lancet found that an elimination diet focusing on common allergenic foods reduced ADHD symptoms in children with food sensitivities.
While not all children with ODD will respond to dietary modifications, those with comorbid allergic conditions, eczema, or digestive complaints may be more likely to benefit from identifying and addressing food sensitivities.
Mediterranean-Style Diet
The Mediterranean diet, rich in fruits, vegetables, whole grains, olive oil, and fish, provides numerous nutrients important for brain health while limiting processed foods and refined sugars. Research in the journal Nutritional Neuroscience has linked adherence to Mediterranean dietary patterns with reduced risk of depression and improved cognitive performance in children and adolescents.
This dietary approach provides essential nutrients like omega-3 fatty acids, antioxidants, and complex carbohydrates that support optimal brain function and stress resilience, potentially benefiting children with emotional and behavioral regulation challenges like ODD.
Lifestyle and Environmental Modifications
Beyond supplements and dietary approaches, various lifestyle modifications can significantly impact ODD symptoms and complement other interventions.
Physical Activity
Regular exercise has well-documented benefits for mood, attention, and behavioral regulation in children. A meta-analysis in the Journal of Pediatric Psychology found that physical activity interventions produced significant improvements in externalizing behaviors, including those characteristic of ODD.
The mechanisms likely involve increased production of neurotrophic factors that support brain health, enhanced stress resilience, improved sleep quality, and positive effects on neurotransmitter systems involved in mood regulation. Encouraging daily physical activity, particularly outdoors and in non-competitive formats, may help children with ODD manage their emotional arousal and improve self-regulation.
Sleep Hygiene
Sleep problems frequently accompany behavioral disorders and may exacerbate irritability and poor emotional control. Research in the Journal of Child Psychology and Psychiatry has demonstrated bidirectional relationships between sleep disruption and behavioral problems in children.
Establishing consistent sleep routines, limiting screen time before bed, creating calming bedtime rituals, and addressing any underlying sleep disorders can significantly improve daytime behavior in children with ODD. Supplements like melatonin may help in cases of circadian rhythm disruption, though should be used under healthcare provider guidance.
Mindfulness and Relaxation Techniques
Age-appropriate mindfulness practices and relaxation techniques can help children develop greater awareness of their emotional states and improve self-regulation. A systematic review in Clinical Child and Family Psychology Review found that mindfulness interventions produced significant improvements in executive functioning and emotional regulation in children with behavioral disorders.
Simple practices like deep breathing exercises, progressive muscle relaxation, guided imagery, and child-oriented meditation can be incorporated into daily routines to help children with ODD recognize and manage the escalation of negative emotions before they lead to behavioral outbursts.
Integrated Approaches to ODD Management
The most effective approach to ODD typically involves integrating conventional treatments with complementary strategies tailored to the individual child’s needs. This personalized, holistic perspective acknowledges the complex, multifactorial nature of the disorder while addressing biological, psychological, and environmental factors simultaneously.
Nutritional Assessment and Intervention
A comprehensive nutritional assessment can identify potential deficiencies or imbalances that might contribute to behavioral symptoms. This may include laboratory testing for key nutrients like vitamin D, zinc, iron, and magnesium, particularly in children with restricted diets or poor nutritional intake.
Based on assessment findings, targeted supplementation can address specific deficiencies, while broader dietary counseling helps families establish sustainable, brain-supportive eating patterns. The goal isn’t necessarily to replace conventional treatments but to optimize physiological foundations for emotional and behavioral regulation.
Collaborative Care Model
Most effective management plans involve collaboration between various professionals, including pediatricians, child psychiatrists, psychologists, nutritionists, and educators. This team approach ensures comprehensive assessment and coordinated interventions across different domains of functioning.
Parents serve as essential partners in this collaborative model, providing valuable insights about their child’s patterns and responses while implementing consistent approaches across environments. Regular communication between team members helps track progress and modify interventions as needed.
Monitoring and Adjustment
Any complementary approach should include systematic monitoring of both benefits and potential adverse effects. Standardized rating scales completed by parents and teachers can track behavioral changes objectively, while regular follow-up with healthcare providers ensures appropriate oversight.
Families should maintain detailed records of which supplements or approaches have been tried, at what dosages, for what duration, and with what results. This information proves invaluable in refining the treatment approach over time and identifying the most effective strategies for each child.
A Balanced Perspective
While research on complementary approaches to ODD continues to evolve, the available evidence suggests that nutritional and holistic interventions may offer valuable adjuncts to conventional treatments. The potential benefits include improved emotional regulation, reduced irritability, enhanced stress resilience, and better overall well-being.
However, these approaches should be pursued thoughtfully, with realistic expectations and appropriate medical supervision. Not all children will respond to the same interventions, and what works for one child may not work for another. The goal should be to develop a personalized, comprehensive approach that addresses the unique needs and circumstances of each child and family affected by ODD.
By combining evidence-based conventional treatments with thoughtfully selected complementary approaches, families can develop a more holistic strategy for managing ODD—one that supports not only behavioral improvement but also overall health, resilience, and quality of life for the affected child and their entire family.
For more information on supplemens for mental health consult our comprehensive guide for micronutrient and supplement therapy and how it can treat specific issues and enhance certain modalities of therapy.
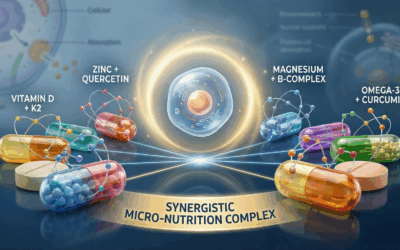
If you’re interested in exploring micronutrient therapy as part of your anxiety treatment plan, Hardy Nutritionals offers a range of products to fit your specific needs. Their Daily Essential Nutrients clinical strength formula provides comprehensive, research-backed dosages in convenient capsule or powder form.
For 15% off in savings, use the offer code “Taproot” at checkout on the Hardy Nutritionals website to receive 15% off your order. @ GetHardy.com
It’s important to remember that while micronutrient therapy can be a powerful tool for managing anxiety, it is not a replacement for professional mental health care. Always consult with a qualified healthcare provider before starting any new supplement regimen, particularly if you have pre-existing health conditions or are taking medications.
Disclaimer: These statements have not been evaluated by the Food and Drug Administration. These products are not intended to diagnose, treat, cure, or prevent any disease. Please consult with a qualified healthcare professional before beginning any supplement regimen, particularly if you are pregnant, nursing, have a medical condition, or are taking medications. The information on this website doesnot constitute medical advice. We recieve a small commision on sales with Hardy Nutritionals through our offer code. Our affiliation does not effect treatment or recomendations made by Taproot authors, therapists or other staff.
References
- American Psychiatric Association. (2022). Diagnostic and Statistical Manual of Mental Disorders (5th ed., Text Revision). https://doi.org/10.1176/appi.books.9780890425787
- Cleveland Clinic. (2023). Oppositional Defiant Disorder (ODD): Symptoms & Treatment. https://my.clevelandclinic.org/health/diseases/9905-oppositional-defiant-disorder
- Aggarwal, A., Marwaha, R., & Sah, P. (2023). Oppositional Defiant Disorder. StatPearls Publishing.
- Gratz, S. S., Jellinek, M. S., Murphy, J. M., & Bishop, S. J. (2008). Oppositional Defiant Disorder. American Family Physician, 78(7), 861-866.
- Amen Clinics. (2023). What Are the Signs and Symptoms of ODD? https://www.amenclinics.com/blog/signs-symptoms-odd/
- ADDitude. (2023). Oppositional Defiant Disorder: ODD Treatment for Children & Adults. https://www.additudemag.com/oppositional-defiant-disorder-odd-treatment/
- Johns Hopkins Medicine. (2024). Oppositional Defiant Disorder (ODD) in Children. https://www.hopkinsmedicine.org/health/conditions-and-diseases/oppositional-defiant-disorder
- Medical News Today. (2023). Oppositional defiant disorder (ODD): Treatment options. https://www.medicalnewstoday.com/articles/treatment-for-oppositional-defiance-disorder
- Psychcentral. (2021). Treating Oppositional Defiant Disorder (ODD). https://psychcentral.com/disorders/oppositional-defiant-disorder-treatment
- Firth, J., Teasdale, S. B., Allott, K., Siskind, D., Marx, W., Cotter, J., … & Sarris, J. (2019). The efficacy and safety of nutrient supplements in the treatment of mental disorders: a meta-review of meta-analyses of randomized controlled trials. World Psychiatry, 18(3), 308-324.
- Johnson, C. R., Turner, K. S., Foldes, E., Brooks, M. M., Kronk, R., & Wiggs, L. (2019). Behavioral parent training to address sleep disturbances in young children with autism spectrum disorder: a pilot trial. Sleep Medicine, 55, 14-23.
- Sarris, J., Logan, A. C., Akbaraly, T. N., Amminger, G. P., Balanzá-Martínez, V., Freeman, M. P., … & Jacka, F. N. (2015). Nutritional medicine as mainstream in psychiatry. The Lancet Psychiatry, 2(3), 271-274.
- Bozzatello, P., Brignolo, E., De Grandi, E., & Bellino, S. (2016). Supplementation with omega-3 fatty acids in psychiatric disorders: a review of literature data. Journal of Clinical Medicine, 5(8), 67.
- Ghodse-Elahi, J., & Manocha, R. (2020). Complementary and Integrative Medicine in Child and Adolescent Psychiatric Disorders: A Practical Clinical Primer. Child and Adolescent Psychiatric Clinics, 29(3), 503-515.
- Cortese, S., Angriman, M., Lecendreux, M., & Konofal, E. (2012). Iron and attention deficit/hyperactivity disorder: What is the empirical evidence so far? A systematic review of the literature. Expert Review of Neurotherapeutics, 12(10), 1227-1240.


















0 Comments