The Limitations of Current Trauma Diagnosis
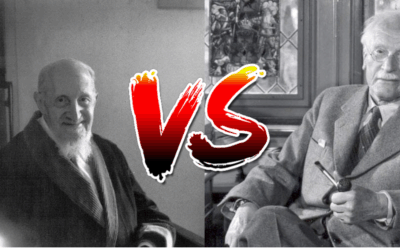
Leading trauma experts Gabor Maté and Bessel van der Kolk have long argued that the DSM-5’s approach to trauma diagnosis fails to capture the complexity of how trauma manifests in different memory systems and psychological processes. As van der Kolk notes in “The Body Keeps the Score,” trauma isn’t a singular experience but rather a constellation of disruptions across multiple domains of functioning. Similarly, Maté emphasizes in his work on trauma and addiction that our diagnostic categories often miss the nuanced ways trauma shapes identity, relationships, and neurological functioning.
The current diagnostic framework tends to compress diverse trauma presentations under the PTSD umbrella, missing critical distinctions that could inform more targeted and effective treatment. This one-size-fits-all approach fails to recognize that trauma can differentially impact various memory systems—from procedural body memories to episodic recall to relational templates—each requiring distinct therapeutic approaches.
Understanding Trauma Through Memory Systems
Relational Memory Trauma
Relational memory trauma involves disrupted attachment patterns and interpersonal schemas formed through early adverse experiences. This type of trauma lives in our implicit expectations about relationships, trust, and safety with others.
Treatment Approaches:
- Dialectical Behavior Therapy (DBT) is particularly effective here, as it directly addresses interpersonal effectiveness skills and emotion regulation within relationships
- Emotionally Focused Therapy (EFT) helps rewire attachment patterns through corrective emotional experiences in current relationships
- Group therapy modalities provide a laboratory for practicing new relational patterns in real-time with peer feedback
Flashbulb Memory Experiencing
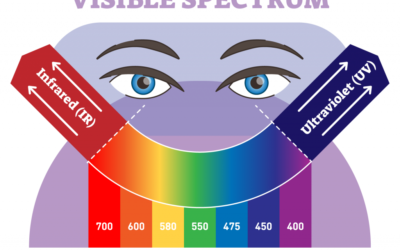
Flashbulb memories are vivid, intrusive sensory memories that feel frozen in time. Unlike narrative memories, these experiences lack temporal context and feel perpetually present, often accompanied by intense physiological activation.
Treatment Approaches:
- Brainspottinghelps individuals connect with and process the somatic and emotional charge of these memories while maintaining dual awareness
- EMDR (Eye Movement Desensitization and Reprocessing) specifically targets these isolated memory networks to facilitate integration
- Somatic Experiencing works with the body’s natural discharge mechanisms to complete interrupted defensive responses
Dissociative Responses and “Third Space”
Dissociation represents a fundamental disruption in consciousness, memory, identity, or perception. When patients retreat to what some clinicians call a “third space”—neither fully present nor completely absent—traditional talk therapy often falls short.
Treatment Approaches:
- Phase-oriented treatment that prioritizes stabilization and resource building before any trauma processing
- Sensorimotor Psychotherapyhelps individuals track and tolerate physical sensations while staying within their window of tolerance
- Internal Family Systems (IFS) works with dissociated parts as protective mechanisms deserving compassion rather than elimination
Alexithymia and Emotional Disconnection
Many trauma survivors experience alexithymia—difficulty identifying and describing emotions. This isn’t simply emotional suppression but a fundamental disconnection from one’s internal emotional landscape.
Treatment Approaches:
- Brainspottingcan help bypass cognitive defenses to access subcortical emotional processing
- Art and expressive therapies provide non-verbal channels for emotional expression and recognition
- Mindfulness-based approaches gradually build interoceptive awareness and emotional vocabulary
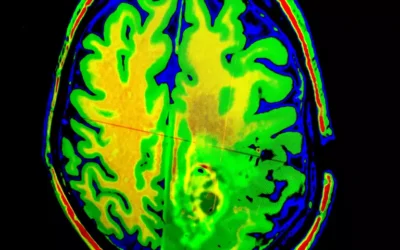
Procedural/Body Memory Trauma
Trauma stored in procedural memory manifests as chronic tension patterns, movement inhibitions, or somatic symptoms without conscious narrative content. The body literally holds the score, as van der Kolk famously stated.
Treatment Approaches:
- Somatic therapies like Hakomi or Somatic Experiencing work directly with body sensations and movement patterns
- Trauma-sensitive yoga helps reclaim agency over one’s body and build new procedural memories of safety
- Craniosacral therapy and bodywork can help release held trauma patterns in the nervous system
The Case for Complex PTSD and Spectrum Approaches
The absence of Complex PTSD (CPTSD) as a formal diagnosis in the DSM-5 represents a significant gap in our diagnostic framework. As Maté and others argue, developmental trauma creates a fundamentally different clinical picture than single-incident trauma, affecting:
- Self-concept and identity formation
- Emotional regulation capacity
- Interpersonal functioning
- Consciousness and dissociation
- Behavioral control
- Meaning-making systems
Learning from the Autism Spectrum Model
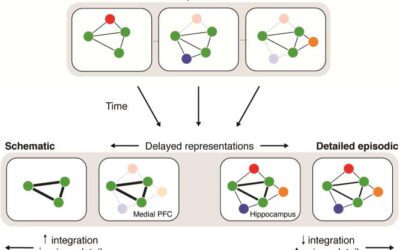
The evolution in how we understand autism offers a powerful template for reconceptualizing trauma diagnosis. Just as autism moved from a binary diagnosis to a multidimensional spectrum recognizing varied presentations across different domains, CPTSD could benefit from a similar framework. The autism spectrum model acknowledges that individuals can have significant challenges in one area (like sensory processing) while having typical or even exceptional functioning in another (like pattern recognition).
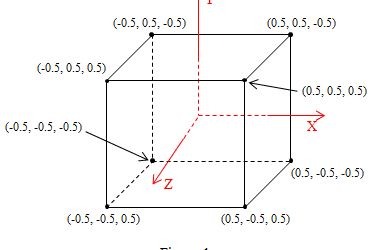
Imagine CPTSD as a multi-pointed star, where each point represents a different domain of trauma impact:
- Relational/Attachment Axis: Ranging from secure relational templates to severe attachment disruption
- Memory Integration Axis: From fully integrated narrative memory to severe fragmentation and flashbulb experiencing
- Somatic/Body Axis: From embodied presence to complete disconnection or chronic somatic symptoms
- Dissociative Axis: From normal consciousness to frequent dissociative episodes and identity fragmentation
- Emotional Regulation Axis: From adaptive emotional processing to alexithymia or emotional dysregulation
This multidimensional model would recognize that someone might have severe relational trauma impacts (scoring high on that axis) while maintaining relatively intact narrative memory processing, or vice versa. Just as we now understand that autism isn’t “more or less severe” but rather presents differently across multiple domains, trauma’s impacts are similarly complex and multifaceted.
Rather than forcing diverse presentations into narrow diagnostic boxes, we need a spectrum approach that recognizes trauma’s varied impacts across multiple domains. This would allow for:
- More precise assessment of which memory systems and functional domains are affected
- Targeted treatment planning that matches interventions to specific deficits
- Recognition of subclinical presentations that don’t meet full criteria but still cause significant impairment
- Validation of developmental trauma as distinct from adult-onset PTSD
Implications for Screening and Treatment
Current screening tools often miss trauma presentations that don’t fit neatly into PTSD criteria. A multidimensional spectrum model, similar to autism assessment tools, would revolutionize trauma treatment by creating individualized trauma profiles. Just as autism support is tailored to someone’s specific profile across different domains, trauma treatment could be precisely matched to where someone falls on each axis of the trauma star.
We need assessment approaches that:
- Screen for different types of memory disruption
- Assess relational patterns and attachment styles
- Evaluate somatic symptoms and body awareness
- Measure dissociative tendencies across a spectrum
- Consider developmental timing and cumulative trauma load
As both Maté and van der Kolk emphasize, healing happens when we match our interventions to the specific ways trauma has impacted an individual. A person with primarily relational trauma needs different support than someone with isolated flashbulb memories or pervasive dissociation. With a multidimensional trauma spectrum model, we could create treatment plans as individualized as those developed for people on the autism spectrum—recognizing that someone might need intensive somatic work for body-based trauma while requiring minimal intervention for emotional regulation, or vice versa.
Moving Forward: An Integrated Approach
The future of trauma treatment lies not in broader diagnostic categories but in more nuanced understanding of trauma’s varied manifestations. By recognizing different memory systems, honoring the wisdom of protective responses like dissociation, and matching treatments to specific presentations, we can offer more effective and compassionate care.
This isn’t about creating more labels but about seeing our clients more clearly. When we understand that DBT might transform someone’s relational patterns while barely touching their somatic hypervigilance, or that EMDR might resolve intrusive memories while leaving attachment wounds untouched, we can craft truly integrative treatment plans.
As our understanding of trauma’s neurobiological impacts continues to evolve, our diagnostic and treatment frameworks must evolve as well. The pioneers like Maté and van der Kolk have shown us the path—now it’s up to the field to walk it.


















0 Comments