
-
Why do we Sleep?
Sleep is a fundamental biological process that is essential for the health and well-being of all mammals, including humans. Despite its ubiquity and importance, sleep remains one of the most mysterious and poorly understood aspects of our lives. In this article, we will explore the complex architecture of sleep, including its neurobiology, evolution, and therapeutic implications. We will examine the different stages of sleep, the role of dreams in Jungian analysis, and the various ways in which sleep can be disrupted or enhanced through pharmacological and behavioral interventions. By the end of this article, you will have a deeper understanding of the science and psychology of sleep, and how this knowledge can be applied to improve your own sleep and well-being.
-
The Neurobiology of Sleep
Sleep is a highly complex and dynamic process that involves multiple regions of the brain and a delicate balance of neurotransmitters and hormones. At its most basic level, sleep is regulated by two main processes: the circadian rhythm and the homeostatic sleep drive [1].
The circadian rhythm is an internal biological clock that regulates the timing of sleep and wakefulness over a 24-hour period. This rhythm is controlled by a small region of the brain called the suprachiasmatic nucleus (SCN), which is located in the hypothalamus [2]. The SCN receives input from specialized light-sensitive cells in the retina, which allows it to synchronize the body’s internal clock with the external light-dark cycle [3].
The homeostatic sleep drive, on the other hand, is a process that builds up over the course of the day and creates a pressure to sleep. This pressure is thought to be mediated by the accumulation of a chemical called adenosine in the brain [4]. As adenosine levels rise, they inhibit the activity of wake-promoting neurons and increase the activity of sleep-promoting neurons, leading to feelings of sleepiness and the eventual onset of sleep [5].
During sleep, the brain cycles through a series of distinct stages, each characterized by specific patterns of brain activity and physiological changes. The two main types of sleep are rapid eye movement (REM) sleep and non-REM (NREM) sleep, which can be further subdivided into three stages: N1, N2, and N3 (also known as slow-wave sleep) [6].
NREM sleep is characterized by a progressive slowing of brain activity, as measured by electroencephalography (EEG). During N1 sleep, which is the lightest stage of sleep, the EEG shows a mix of alpha and theta waves, and the sleeper may experience hypnagogic hallucinations and a sense of falling [7]. As sleep deepens into N2 and N3, the EEG shows an increasing proportion of slow delta waves, and the sleeper becomes more difficult to awaken [8].
REM sleep, in contrast, is characterized by a highly active and desynchronized EEG pattern that resembles wakefulness. During REM sleep, the eyes move rapidly behind closed lids, and the sleeper experiences vivid, emotionally charged dreams [9]. REM sleep is also associated with a profound loss of muscle tone, which is thought to protect the sleeper from acting out their dreams [10].
The cycling between NREM and REM sleep occurs in a predictable pattern throughout the night, with each cycle lasting approximately 90-120 minutes [11]. In healthy adults, the first half of the night is dominated by deep NREM sleep, while the second half of the night is characterized by longer periods of REM sleep [12]. This pattern changes with age, with older adults experiencing less deep NREM sleep and more fragmented sleep overall [13].
-
The Evolution of Sleep
Sleep is a highly conserved behavior that has been observed in all mammals studied to date, as well as in many other animal species, including birds, reptiles, and even some invertebrates [14]. This suggests that sleep serves a crucial evolutionary function that has been shaped by natural selection over millions of years.
One of the leading theories for the evolution of sleep is the “energy conservation hypothesis,” which proposes that sleep evolved as a way to conserve energy during periods of inactivity [15]. According to this theory, animals that were able to reduce their metabolic rate and conserve energy during sleep would have had a selective advantage over those that remained active and expended more energy [16].
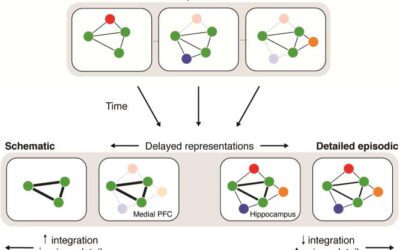
Another theory for the evolution of sleep is the “brain plasticity hypothesis,” which proposes that sleep evolved as a way to facilitate the consolidation and reorganization of memories and neural connections [17]. According to this theory, sleep provides a unique opportunity for the brain to “offline” from the demands of wakefulness and engage in the process of synaptic plasticity, which is essential for learning and memory [18].
Recent research has also suggested that sleep may play a crucial role in the clearance of metabolic waste products from the brain [19]. During sleep, the glymphatic system, which is a network of channels that surround blood vessels in the brain, becomes highly active and facilitates the removal of toxins and other waste products that accumulate during wakefulness [20]. This process is thought to be essential for maintaining brain health and preventing the buildup of neurotoxic substances that have been implicated in neurodegenerative diseases such as Alzheimer’s [21].
-
Sleep as a Compensatory Mechanism
In addition to its role in energy conservation and brain plasticity, sleep is also thought to serve as a compensatory mechanism for the brain. During wakefulness, the brain is constantly processing sensory information, making decisions, and generating responses to environmental stimuli. This high level of activity places a significant demand on the brain’s resources, including its supply of energy and neurotransmitters [22].
Over the course of the day, this demand can lead to a progressive buildup of “sleep pressure,” which is mediated by the accumulation of adenosine and other neurochemicals in the brain [23]. As sleep pressure builds, it becomes increasingly difficult to maintain wakefulness, and the brain begins to compensate by shifting its activity towards sleep-promoting regions and neurotransmitters [24].
During sleep, particularly during deep NREM sleep, the brain undergoes a process of restoration and repair that helps to counteract the effects of wakefulness [25]. This process involves the synthesis of new proteins, the replenishment of neurotransmitters, and the strengthening of neural connections that are important for learning and memory [26].
Sleep is also thought to play a role in the regulation of emotions and the processing of emotional memories [27]. During REM sleep, the brain is highly active in regions associated with emotion and memory, such as the amygdala and hippocampus [28]. This activity is thought to facilitate the integration of emotional experiences into long-term memory and the resolution of emotional conflicts [29].
-
Sleep Disruption and Its Consequences
Despite the importance of sleep for brain health and function, sleep disruption is a common problem that affects millions of people worldwide. Sleep disruption can take many forms, from difficulty falling asleep or staying asleep to abnormal sleep patterns or insufficient sleep duration [30].
One of the most common causes of sleep disruption is insomnia, which is defined as difficulty initiating or maintaining sleep that leads to daytime impairment [31]. Insomnia can be caused by a variety of factors, including stress, anxiety, depression, medical conditions, and medications [32]. Chronic insomnia has been associated with a range of negative health outcomes, including increased risk of cardiovascular disease, diabetes, and cognitive impairment [33].
Another common form of sleep disruption is sleep apnea, which is a condition characterized by repeated pauses in breathing during sleep [34]. Sleep apnea can lead to fragmented sleep, daytime sleepiness, and an increased risk of cardiovascular disease and other health problems [35].
Sleep disruption can also occur as a result of circadian rhythm disorders, which are conditions that affect the timing of sleep and wakefulness [36]. Examples of circadian rhythm disorders include jet lag, shift work disorder, and delayed sleep phase syndrome [37]. These disorders can lead to chronic sleep deprivation and associated health problems, such as obesity, diabetes, and depression [38].
-
Dreams and Jungian Analysis
One of the most fascinating aspects of sleep is the experience of dreaming, which occurs primarily during REM sleep. Dreams are often vivid, emotionally charged, and symbolically rich experiences that can provide valuable insights into the workings of the unconscious mind [39].
In Jungian analysis, dreams are seen as a direct expression of the unconscious and are used as a tool for self-discovery and personal growth [40]. According to Jung, dreams are a way for the unconscious to communicate with the conscious mind and to compensate for any imbalances or one-sidedness in the individual’s psyche [41].
Jung believed that dreams are shaped by archetypal patterns and symbols that are universal to the human experience [42]. These archetypes are thought to be inherited predispositions that shape our perceptions, emotions, and behaviors, and that are expressed through the language of symbols and metaphors [43].
In Jungian dream analysis, the goal is to uncover the symbolic meaning of the dream and to integrate its message into the conscious mind [44]. This process often involves exploring the personal associations and emotions associated with the dream symbols, as well as examining their archetypal significance [45].
One of the unique aspects of dreaming is that it occurs without the interference of the ego, which is the conscious, rational part of the mind [46]. During REM sleep, the prefrontal cortex, which is involved in executive function and self-awareness, is largely deactivated, allowing for the unfiltered expression of unconscious content [47].
This lack of ego control is what makes dreams such a valuable tool for psychotherapy, as they provide a direct window into the unconscious mind and its underlying conflicts and desires [48]. By working with dreams in therapy, individuals can gain insight into their own psychological processes and work towards greater self-awareness and personal growth [49].
-
Pharmacology and Sleep
While behavioral interventions such as sleep hygiene and cognitive-behavioral therapy are often the first line of treatment for sleep disorders, pharmacological interventions can also be useful in certain cases [50]. There are a wide variety of medications and supplements that can be used to promote sleep, each with its own mechanism of action and potential side effects [51].
One of the most commonly used medications for sleep is benzodiazepines, which are a class of sedative drugs that work by enhancing the activity of the neurotransmitter GABA [52]. Benzodiazepines such as diazepam and lorazepam are effective at promoting sleep onset and reducing nighttime awakenings, but they can also cause side effects such as daytime drowsiness, cognitive impairment, and dependence [53].
Another class of medications used for sleep is non-benzodiazepine hypnotics, such as zolpidem and eszopiclone [54]. These medications work by selectively targeting specific subtypes of the GABA receptor, which may reduce some of the side effects associated with benzodiazepines [55]. However, non-benzodiazepine hypnotics can still cause side effects such as headache, dizziness, and sleepwalking [56].
In addition to prescription medications, there are also many over-the-counter supplements and natural remedies that are used to promote sleep. Some of the most commonly used supplements include:
Melatonin:
a hormone that is naturally produced by the pineal gland and helps to regulate the sleep-wake cycle [57]. Melatonin supplements can be effective at reducing the time it takes to fall asleep and improving sleep quality, particularly in individuals with circadian rhythm disorders [58].
Valerian root:
an herb that has been used for centuries to promote sleep and reduce anxiety [59]. Valerian root is thought to work by increasing the levels of GABA in the brain, although its exact mechanism of action is not fully understood [60].
L-theanine:
an amino acid found in green tea that has been shown to promote relaxation and improve sleep quality [61]. L-theanine is thought to work by increasing the levels of GABA and serotonin in the brain, as well as reducing the levels of excitatory neurotransmitters such as glutamate [62].
Magnesium:
a mineral that is involved in a wide range of physiological processes, including muscle relaxation and neurotransmitter synthesis [63]. Magnesium deficiency has been linked to insomnia and other sleep disorders, and magnesium supplements have been shown to improve sleep quality in some studies [64].
While these supplements can be effective for some individuals, it is important to note that they can also interact with other medications and cause side effects in some cases [65]. It is always best to consult with a healthcare provider before starting any new supplement or medication for sleep.
In addition to medications and supplements, there are also certain substances that can disrupt sleep and should be avoided, particularly in the hours leading up to bedtime. These include:
Caffeine:
a stimulant found in coffee, tea, and many soft drinks that can interfere with sleep onset and quality [66]. Caffeine has a half-life of 3-5 hours, which means that it can take several hours for its effects to wear off [67].
Alcohol:
while alcohol can initially promote sleepiness, it can also disrupt sleep architecture and lead to more frequent nighttime awakenings [68]. Alcohol use has been linked to an increased risk of sleep apnea and other sleep disorders [69].
Nicotine:
a stimulant found in tobacco products that can interfere with sleep onset and quality [70]. Nicotine use has been linked to an increased risk of insomnia and other sleep disorders [71].
Marijuana:
while some individuals use marijuana to promote sleep, it can also disrupt sleep architecture and lead to more frequent nighttime awakenings [72]. Long-term marijuana use has been linked to an increased risk of insomnia and other sleep disorders [73].
-
Sleep Hygiene and Behavioral Interventions
While pharmacological interventions can be useful in certain cases, behavioral interventions are often the first line of treatment for sleep disorders [74]. Sleep hygiene is a set of behaviors and environmental factors that can promote healthy sleep, and it is an important component of many behavioral interventions for sleep [75].
Some of the key components of sleep hygiene include:
- Maintaining a consistent sleep schedule: going to bed and waking up at the same time each day, even on weekends, can help to regulate the body’s circadian rhythm and promote healthy sleep [76].
- Creating a sleep-conducive environment: the bedroom should be dark, quiet, and cool, with a comfortable mattress and pillows [77]. Electronic devices such as smartphones and televisions should be kept out of the bedroom, as the blue light emitted by these devices can interfere with the production of melatonin [78].
- Avoiding stimulants and large meals before bedtime: caffeine, alcohol, and nicotine should be avoided in the hours leading up to bedtime, as they can interfere with sleep onset and quality [79]. Large meals should also be avoided close to bedtime, as they can cause indigestion and disrupt sleep [80].
- Engaging in relaxation techniques: practices such as deep breathing, progressive muscle relaxation, and meditation can help to reduce stress and promote relaxation, making it easier to fall asleep [81].
In addition to sleep hygiene, there are also several behavioral interventions that can be effective for treating sleep disorders. These include:
- Cognitive-behavioral therapy for insomnia (CBT-I): a structured therapy that aims to identify and change the thoughts and behaviors that contribute to insomnia [82]. CBT-I typically involves a combination of sleep restriction, stimulus control, and cognitive restructuring techniques [83].
- Mindfulness-based interventions: practices such as mindfulness meditation and yoga can help to reduce stress and promote relaxation, making it easier to fall asleep and stay asleep [84]. Mindfulness interventions have been shown to be effective for treating insomnia and other sleep disorders [85].
- Lifespan integration: a therapy that aims to integrate traumatic or stressful experiences into the individual’s overall life narrative [86]. Lifespan integration has been shown to be effective for reducing symptoms of PTSD and other trauma-related disorders, which can often interfere with sleep [87].
- EMDR: a therapy that uses bilateral stimulation to help individuals process traumatic memories and reduce symptoms of PTSD [88]. EMDR has been shown to be effective for reducing symptoms of insomnia and other sleep disorders in individuals with PTSD [89].
- Parts-based therapy: a therapy that aims to identify and work with the different “parts” of the self that may be contributing to sleep disturbances [90]. Parts-based therapy can help individuals to develop a more integrated sense of self and to resolve internal conflicts that may be interfering with sleep [91].
-
Why we can’t sleep
Sleep is a complex and multifaceted process that is essential for physical and mental health. By understanding the neurobiology, evolution, and therapeutic implications of sleep, we can develop a more holistic and effective approach to promoting healthy sleep and treating sleep disorders.
The architecture of sleep is shaped by a delicate balance of neurotransmitters, hormones, and physiological processes that are regulated by the brain. Sleep serves a crucial evolutionary function, helping to conserve energy, facilitate brain plasticity, and clear metabolic waste products from the brain.
Sleep is also a compensatory mechanism that helps to counteract the effects of wakefulness and promote restoration and repair. When sleep is disrupted, it can have significant negative impacts on health and well-being, increasing the risk of cardiovascular disease, diabetes, cognitive impairment, and other health problems.
Dreams are a unique and valuable aspect of sleep that provide a direct window into the unconscious mind. In Jungian analysis, dreams are used as a tool for self-discovery and personal growth, helping individuals to gain insight into their own psychological processes and work towards greater self-awareness and wholeness.
Pharmacological interventions such as medications and supplements can be useful for treating sleep disorders in certain cases, but they can also cause side effects and interact with other medications. Behavioral interventions such as sleep hygiene, cognitive-behavioral therapy, mindfulness-based interventions, lifespan integration, EMDR, and parts-based therapy are often the first line of treatment for sleep disorders and can be highly effective in promoting healthy sleep.
By taking a holistic approach to sleep that addresses both the biological and psychological factors that contribute to sleep disturbances, we can develop more effective and sustainable solutions for promoting healthy sleep and treating sleep disorders. This may involve a combination of behavioral interventions, pharmacological treatments, and lifestyle changes that are tailored to the individual’s unique needs and circumstances.
Ultimately, the goal of understanding the architecture of sleep is to promote greater health, well-being, and quality of life for individuals and society as a whole. By prioritizing sleep as a crucial component of overall health and by developing more effective and accessible interventions for sleep disorders, we can help to create a world where everyone has the opportunity to experience the restorative and transformative power of healthy sleep.
To work on therapy for sleep in Alabama schedule teletherapy with Pamela Hayes, Kristan Baer, or Haley Beech at Taproot Therapy.
-
Bibliography
[1] Borbély, A. A., Daan, S., Wirz-Justice, A., & Deboer, T. (2016). The two-process model of sleep regulation: a reappraisal. Journal of Sleep Research, 25(2), 131-143.
[2] Mohawk, J. A., Green, C. B., & Takahashi, J. S. (2012). Central and peripheral circadian clocks in mammals. Annual Review of Neuroscience, 35, 445-462.
[3] Hattar, S., Liao, H. W., Takao, M., Berson, D. M., & Yau, K. W. (2002). Melanopsin-containing retinal ganglion cells: architecture, projections, and intrinsic photosensitivity. Science, 295(5557), 1065-1070.
[4] Porkka-Heiskanen, T., Strecker, R. E., Thakkar, M., Bjorkum, A. A., Greene, R. W., & McCarley, R. W. (1997). Adenosine: a mediator of the sleep-inducing effects of prolonged wakefulness. Science, 276(5316), 1265-1268.
[5] Saper, C. B., Fuller, P. M., Pedersen, N. P., Lu, J., & Scammell, T. E. (2010). Sleep state switching. Neuron, 68(6), 1023-1042.
[6] Carskadon, M. A., & Dement, W. C. (2011). Normal human sleep: an overview. Principles and Practice of Sleep Medicine, 5, 16-26.
[7] Ogilvie, R. D. (2001). The process of falling asleep. Sleep Medicine Reviews, 5(3), 247-270.
[8] Dijk, D. J. (2009). Regulation and functional correlates of slow wave sleep. Journal of Clinical Sleep Medicine, 5(2 Suppl), S6-S15.
[9] Hobson, J. A. (2009). REM sleep and dreaming: towards a theory of protoconsciousness. Nature Reviews Neuroscience, 10(11), 803-813.
[10] Peever, J., & Fuller, P. M. (2017). The biology of REM sleep. Current Biology, 27(22), R1237-R1248.
[11] Carskadon, M. A., & Dement, W. C. (2005). Normal human sleep: an overview. Principles and Practice of Sleep Medicine, 4, 13-23.
[12] Ohayon, M. M., Carskadon, M. A., Guilleminault, C., & Vitiello, M. V. (2004). Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep, 27(7), 1255-1273.
[13] Mander, B. A., Winer, J. R., & Walker, M. P. (2017). Sleep and human aging. Neuron, 94(1), 19-36.
[14] Siegel, J. M. (2005). Clues to the functions of mammalian sleep. Nature, 437(7063), 1264-1271.
[15] Berger, R. J., & Phillips, N. H. (1995). Energy conservation and sleep. Behavioural Brain Research, 69(1-2), 65-73.
[16] Siegel, J. M. (2009). Sleep viewed as a state of adaptive inactivity. Nature Reviews Neuroscience, 10(10), 747-753.
[17] Tononi, G., & Cirelli, C. (2014). Sleep and the price of plasticity: from synaptic and cellular homeostasis to memory consolidation and integration. Neuron, 81(1), 12-34.
[18] Rasch, B., & Born, J. (2013). About sleep’s role in memory. Physiological Reviews, 93(2), 681-766.
[19] Xie, L., Kang, H., Xu, Q., Chen, M. J., Liao, Y., Thiyagarajan, M., … & Nedergaard, M. (2013). Sleep drives metabolite clearance from the adult brain. Science, 342(6156), 373-377.
[20] Jessen, N. A., Munk, A. S. F., Lundgaard, I., & Nedergaard, M. (2015). The glymphatic system: a beginner’s guide. Neurochemical Research, 40(12), 2583-2599.
[21] Shokri-Kojori, E., Wang, G. J., Wiers, C. E., Demiral, S. B., Guo, M., Kim, S. W., … & Volkow, N. D. (2018). β-Amyloid accumulation in the human brain after one night of sleep deprivation. Proceedings of the National Academy of Sciences, 115(17), 4483-4488.
[22] Krueger, J. M., Frank, M. G., Wisor, J. P., & Roy, S. (2016). Sleep function: toward elucidating an enigma. Sleep Medicine Reviews, 28, 46-54.
[23] Porkka-Heiskanen, T., & Kalinchuk, A. V. (2011). Adenosine, energy metabolism and sleep homeostasis. Sleep Medicine Reviews, 15(2), 123-135.
[24] Saper, C. B., Scammell, T. E., & Lu, J. (2005). Hypothalamic regulation of sleep and circadian rhythms. Nature, 437(7063), 1257-1263.
[25] Vyazovskiy, V. V., & Harris, K. D. (2013). Sleep and the single neuron: the role of global slow oscillations in individual cell rest. Nature Reviews Neuroscience, 14(6), 443-451.
[26] Tononi, G., & Cirelli, C. (2006). Sleep function and synaptic homeostasis. Sleep Medicine Reviews, 10(1), 49-62.
[27] Walker, M. P., & van der Helm, E. (2009). Overnight therapy? The role of sleep in emotional brain processing. Psychological Bulletin, 135(5), 731-748.
[28] Nir, Y., & Tononi, G. (2010). Dreaming and the brain: from phenomenology to neurophysiology. Trends in Cognitive Sciences, 14(2), 88-100.
[29] Walker, M. P. (2009). The role of sleep in cognition and emotion. Annals of the New York Academy of Sciences, 1156(1), 168-197.
[30] Roth, T. (2007). Insomnia: definition, prevalence, etiology, and consequences. Journal of Clinical Sleep Medicine, 3(5 Suppl), S7-S10.
[31] American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing.
[32] Ohayon, M. M. (2002). Epidemiology of insomnia: what we know and what we still need to learn. Sleep Medicine Reviews, 6(2), 97-111.
[33] Fernandez-Mendoza, J., & Vgontzas, A. N. (2013). Insomnia and its impact on physical and mental health. Current Psychiatry Reports, 15(12), 418.
[34] Jordan, A. S., McSharry, D. G., & Malhotra, A. (2014). Adult obstructive sleep apnoea. The Lancet, 383(9918), 736-747.
[35] Lévy, P., Kohler, M., McNicholas, W. T., Barbé, F., McEvoy, R. D., Somers, V. K., … & Pépin, J. L. (2015). Obstructive sleep apnoea syndrome. Nature Reviews Disease Primers, 1(1), 1-21.
[36] Sack, R. L., Auckley, D., Auger, R. R., Carskadon, M. A., Wright Jr, K. P., Vitiello, M. V., & Zhdanova, I. V. (2007). Circadian rhythm sleep disorders: part I, basic principles, shift work and jet lag disorders. Sleep, 30(11), 1460-1483.
[37] Reid, K. J., & Abbott, S. M. (2015). Jet lag and shift work disorder. Sleep Medicine Clinics, 10(4), 523-535.
[38] Knutson, K. L., Spiegel, K., Penev, P., & Van Cauter, E. (2007). The metabolic consequences of sleep deprivation. Sleep Medicine Reviews, 11(3), 163-178.
[39] Hobson, J. A. (2005). Sleep is of the brain, by the brain and for the brain. Nature, 437(7063), 1254-1256.
[40] Jung, C. G. (2010). Dreams. Princeton University Press.
[41] Jung, C. G. (2014). The archetypes and the collective unconscious. Routledge.
[42] Knox, J. (2003). Archetype, attachment, analysis: Jungian psychology and the emergent mind. Routledge.
[43] Cambray, J. (2009). Synchronicity: Nature and psyche in an interconnected universe. Texas A&M University Press.
[44] Whitmont, E. C., & Perera, S. B. (1991). Dreams, a portal to the source. Routledge.
[45] Stevens, A. (2002). Archetype revisited: An updated natural history of the self. Routledge.
[46] Stickgold, R., Hobson, J. A., Fosse, R., & Fosse, M. (2001). Sleep, learning, and dreams: off-line memory reprocessing. Science, 294(5544), 1052-1057.
[47] Braun, A. R., Balkin, T. J., Wesenten, N. J., Carson, R. E., Varga, M., Baldwin, P., … & Herscovitch, P. (1997). Regional cerebral blood flow throughout the sleep-wake cycle. Brain, 120(7), 1173-1197.
[48] Bulkeley, K. (Ed.). (2001). Dreams: A reader on the religious, cultural, and psychological dimensions of dreaming. Springer.
[49] Hill, C. E. (2004). Dream work in therapy: Facilitating exploration, insight, and action. American Psychological Association.
[50] Morin, C. M., Vallières, A., & Ivers, H. (2007). Dysfunctional beliefs and attitudes about sleep (DBAS): validation of a brief version (DBAS-16). Sleep, 30(11), 1547-1554.
[51] Mendelson, W. B. (2017). The science of sleep: what it is, how it works, and why it matters. University of Chicago Press.
[52] Winkelman, J. W. (2015). Clinical practice. Insomnia disorder. The New England Journal of Medicine, 373(15), 1437-1444.
[53] Lader, M. (2011). Benzodiazepines revisited—will we ever learn?. Addiction, 106(12), 2086-2109.
[54] Sanger, D. J. (2004). The pharmacology and mechanisms of action of new generation, non-benzodiazepine hypnotic agents. CNS Drugs, 18(1), 9-15.
[55] Nutt, D. J., & Stahl, S. M. (2010). Searching for perfect sleep: the continuing evolution of GABAA receptor modulators as hypnotics. Journal of Psychopharmacology, 24(11), 1601-1612.
[56] Gunja, N. (2013). In the Zzz zone: the effects of Z-drugs on human performance and driving. Journal of Medical Toxicology, 9(2), 163-171.
[57] Zhdanova, I. V. (2005). Melatonin as a hypnotic: pro. Sleep Medicine Reviews, 9(1), 51-65.
[58] Ferracioli-Oda, E., Qawasmi, A., & Bloch, M. H. (2013). Meta-analysis: melatonin for the treatment of primary sleep disorders. PloS One, 8(5), e63773.
[59] Bent, S., Padula, A., Moore, D., Patterson, M., & Mehling, W. (2006). Valerian for sleep: a systematic review and meta-analysis. The American Journal of Medicine, 119(12), 1005-1012.
[60] Hadjikhani, N. (2010). Serotonin, pregnancy and increased autism prevalence: is there a link?. Medical Hypotheses, 74(5), 880-883.
[61] Nobre, A. C., Rao, A., & Owen, G. N. (2008). L-theanine, a natural constituent in tea, and its effect on mental state. Asia Pacific Journal of Clinical Nutrition, 17(S1), 167-168.
[62] Juneja, L. R., Chu, D. C., Okubo, T., Nagato, Y., & Yokogoshi, H. (1999). L-theanine—a unique amino acid of green tea and its relaxation effect in humans. Trends in Food Science & Technology, 10(6-7), 199-204.
[63] Rondanelli, M., Opizzi, A., Monteferrario, F., Antoniello, N., Manni, R., & Klersy, C. (2011). The effect of melatonin, magnesium, and zinc on primary insomnia in long‐term care facility residents in Italy: a double‐blind, placebo‐controlled clinical trial. Journal of the American Geriatrics Society, 59(1), 82-90.
[64] Abbasi, B., Kimiagar, M., Sadeghniiat, K., Shirazi, M. M., Hedayati, M., & Rashidkhani, B. (2012). The effect of magnesium supplementation on primary insomnia in elderly: A double-blind placebo-controlled clinical trial. Journal of Research in Medical Sciences: the Official Journal of Isfahan University of Medical Sciences, 17(12), 1161.
[65] Lakhan, S. E., & Vieira, K. F. (2008). Nutritional therapies for mental disorders. Nutrition Journal, 7(1), 2.
[66] Drake, C., Roehrs, T., Shambroom, J., & Roth, T. (2013). Caffeine effects on sleep taken 0, 3, or 6 hours before going to bed. Journal of Clinical Sleep Medicine, 9(11), 1195-1200.
[67] Roehrs, T., & Roth, T. (2008). Caffeine: sleep and daytime sleepiness. Sleep Medicine Reviews, 12(2), 153-162.
[68] Stein, M. D., & Friedberg, J. S. (2001). Sleep, alcohol, and alcoholism. Alcohol Research & Health, 25(2), 101-109.
[69] Heinzer, R., Vat, S., Marques-Vidal, P., Marti-Soler, H., Andries, D., Tobback, N., … & Haba-Rubio, J. (2015). Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. The Lancet Respiratory Medicine, 3(4), 310-318.
[70] Jaehne, A., Loessl, B., Bárkai, Z., Riemann, D., & Hornyak, M. (2009). Effects of nicotine on sleep during consumption, withdrawal and replacement therapy. Sleep Medicine Reviews, 13(5), 363-377.
[71] Davila, D. G., Hurt, R. D., Offord, K. P., Harris, C. D., & Shepard Jr, J. W. (1994). Acute effects of transdermal nicotine on sleep architecture, snoring, and sleep-disordered breathing in nonsmokers. American Journal of Respiratory and Critical Care Medicine, 150(2), 469-474.
[72] Schierenbeck, T., Riemann, D., Berger, M., & Hornyak, M. (2008). Effect of illicit recreational drugs upon sleep: cocaine, ecstasy and marijuana. Sleep Medicine Reviews, 12(5), 381-389.
[73] Babson, K. A., Sottile, J., & Morabito, D. (2017). Cannabis, cannabinoids, and sleep: a review of the literature. Current Psychiatry Reports, 19(4), 23.
[74] Irish, L. A., Kline, C. E., Gunn, H. E., Buysse, D. J., & Hall, M. H. (2015). The role of sleep hygiene in promoting public health: A review of empirical evidence. Sleep Medicine Reviews, 22, 23-36.
[75] Stepanski, E. J., & Wyatt, J. K. (2003). Use of sleep hygiene in the treatment of insomnia. Sleep Medicine Reviews, 7(3), 215-225.
[76] Youngstedt, S. D., O’Connor, P. J., & Dishman, R. K. (1997). The effects of acute exercise on sleep: a quantitative synthesis. Sleep, 20(3), 203-214.
[77] Czeisler, C. A., Kronauer, R. E., Allan, J. S., Duffy, J. F., Jewett, M. E., Brown, E. N., & Ronda, J. M. (1989). Bright light induction of strong (type 0) resetting of the human circadian pacemaker. Science, 244(4910), 1328-1333.
[78] Chang, A. M., Aeschbach, D., Duffy, J. F., & Czeisler, C. A. (2015). Evening use of light-emitting eReaders negatively affects sleep, circadian timing, and next-morning alertness. Proceedings of the National Academy of Sciences, 112(4), 1232-1237.
[79] Cain, N., & Gradisar, M. (2010). Electronic media use and sleep in school-aged children and adolescents: A review. Sleep Medicine, 11(8), 735-742.
[80] Vela-Bueno, A., Fernandez-Mendoza, J., & Olavarrieta-Bernardino, S. (2009). Sleep patterns in the transition from adolescence to young adulthood. Sleep Medicine Clinics, 4(1), 77-85.
[81] Morin, C. M., Hauri, P. J., Espie, C. A., Spielman, A. J., Buysse, D. J., & Bootzin, R. R. (1999). Nonpharmacologic treatment of chronic insomnia. Sleep, 22(8), 1134-1156.
[82] Edinger, J. D., & Carney, C. E. (2015). Overcoming insomnia: A cognitive-behavioral therapy approach, therapist guide. Oxford University Press.
[83] Edinger, J. D., & Means, M. K. (2005). Cognitive–behavioral therapy for primary insomnia. Clinical Psychology Review, 25(5), 539-558.
[84] Winbush, N. Y., Gross, C. R., & Kreitzer, M. J. (2007). The effects of mindfulness-based stress reduction on sleep disturbance: a systematic review. Explore, 3(6), 585-591.
[85] Gross, C. R., Kreitzer, M. J., Reilly-Spong, M., Wall, M., Winbush, N. Y., Patterson, R., … & Cramer-Bornemann, M. (2011). Mindfulness-based stress reduction versus pharmacotherapy for chronic primary insomnia: a randomized controlled clinical trial. Explore, 7(2), 76-87.
[86] Pace-Schott, E. F., Germain, A., & Milad, M. R. (2015). Sleep and REM sleep disturbance in the pathophysiology of PTSD: the role of extinction memory. Biology of Mood & Anxiety Disorders, 5(1), 3.
[87] Krakow, B., Hollifield, M., Johnston, L., Koss, M., Schrader, R., Warner, T. D., … & Prince, H. (2001). Imagery rehearsal therapy for chronic nightmares in sexual assault survivors with posttraumatic stress disorder: a randomized controlled trial. JAMA, 286(5), 537-545.
[88] Raboni, M. R., Alonso, F. F. D., Tufik, S., & Suchecki, D. (2014). Improvement of mood and sleep alterations in posttraumatic stress disorder patients by eye movement desensitization and reprocessing. Frontiers in Behavioral Neuroscience, 8, 209.
[89] Raboni, M. R., Tufik, S., & Suchecki, D. (2006). Treatment of PTSD by eye movement desensitization reprocessing (EMDR) improves sleep quality, quality of life, and perception of stress. Annals of the New York Academy of Sciences, 1071(1), 508-513.
[90] Schwartz, R. C. (1995). Internal family systems therapy. Guilford Press.
[91] Anderson, R., & Braud, W. (2011). Transforming self and others through research: Transpersonal research methods and skills for the human sciences and humanities. Suny Press.

















0 Comments