Flaws of the Modern Medical Research Establishment
For as long as I can remember, I’ve suffered from chronic ear and sinus infections. The cycle is always the same – an ear infection treated with antibiotics migrates to my sinuses, causing a sinus infection. When I treat the sinus infection, it moves back to the other ear. This pattern has plagued me since childhood, making me intimately familiar with the misery of constant congestion.
From a young age, doctors routinely prescribed oral decongestants, insisting I take them regularly. But even as a child, I knew they didn’t work for me. I told the doctors that these medicines made me drowsy without relieving my congestion, but they dismissed my concerns as unscientific. They cited evidence of the drugs’ effectiveness and instructed my mother to administer them to me every morning.
The side effects of these medications, forced on me despite my protests, contributed to my being diagnosed with and overmedicated for ADHD – but that’s a story for another time. The crux of the matter is this: from the age of 6 until 31, I, the patient, repeatedly told medical professionals that oral decongestants were ineffective for me, yet I was continuously told that research magically proved my lived experience false.
The Illusion of Evidence-Based Medicine
Fast forward to the present, and we find that oral decongestants are being pulled from pharmacy shelves en masse. How could this happen when we’ve been assured that evidence-based research and our hyper-empirical medical model are rational, sane, and infallible? The answer lies in understanding the incentive structures underpinning medical research.
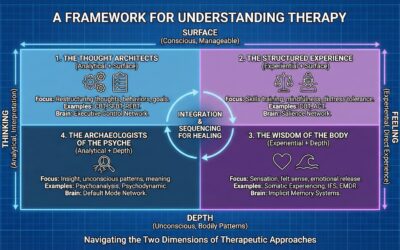
At its core, the incentive structure of research is driven by sales. In the field of psychology, for example, I’ve previously written about how treatments like cognitive behavioral therapy (CBT) garner more research validation despite lack of clinical advocacy or efficacy. Why? Because CBT relies on empirical assessment, making it far more conducive to research than models with subjective or intuitive elements.
The Flawed Drug Development Process
On the surface, the drug development process appears rigorous, with multiple stages designed to ensure safety and efficacy:
- Discovery and Development: This stage involves basic research to understand a disease, identify potential drug targets, and discover lead compounds that could potentially treat the disease. Initial safety tests are also conducted.
- Preclinical Research: Here, the potential drug is tested in vitro (in the lab) and in vivo (in animal models) to assess its safety and biological activity. Toxicity testing is a key component of this stage.
- Clinical Research: If the preclinical results are promising, the drug moves into human trials. These typically include:
- Phase 1: Safety testing in a small group of healthy volunteers.
- Phase 2: Efficacy and side effect studies in a larger group of people with the condition the drug is designed to treat.
- Phase 3: Large-scale testing for efficacy and monitoring of adverse reactions.
- Review and Approval: If the clinical trials are successful, the drug developer submits a New Drug Application (NDA) or Biologics License Application (BLA) to regulatory agencies such as the FDA. The agency reviews all the data and may request additional information or studies before making a decision.
- Post-Market Monitoring: Even after approval, the drug continues to be monitored for safety and effectiveness in the general population.
In theory, this rigorous process should prevent ineffective or harmful drugs from reaching consumers. However, each step is compromised by the profit motive driving the pharmaceutical industry and the academic institutions that conduct much of the research.
The McNamara Fallacy and the Failure of Objective Measures
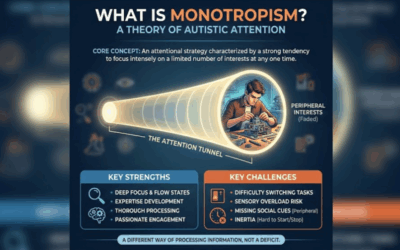
The overreliance on quantitative data in medical research, to the exclusion of qualitative factors, is a prime example of the McNamara fallacy. Named after Robert McNamara, the U.S. Secretary of Defense during the Vietnam War, this fallacy refers to the mistake of making decisions based solely on quantitative observations and ignoring all other forms of evidence.
In the context of medical research, this plays out in the overemphasis on objective, quantifiable measures, such as symptom reduction or biomarker changes, while ignoring the subjective experiences of patients and the intuitive observations of clinicians. This narrow focus fails to capture the full complexity of human health and illness.
Moreover, even these supposedly objective measures can be gamed. Pharmaceutical companies have been known to cherry-pick data, change study protocols midstream, and selectively publish positive results while burying negative ones. This manipulation of “objective” data undermines the very foundation of evidence-based medicine.
The Influence of Money on Research
The corruption of medical research by financial interests is pervasive and well-documented. Pharmaceutical companies fund a large proportion of medical research, and this funding comes with strings attached. Studies funded by industry are more likely to produce results favorable to the sponsor’s product, a clear conflict of interest.
But the influence of money goes beyond just direct research funding. Pharmaceutical companies also pay for medical education, sponsor conferences, and provide lucrative consulting and speaking gigs for key opinion leaders. This creates a culture in which challenging the status quo or questioning the effectiveness of profitable drugs becomes difficult, if not career-limiting.
Academic researchers are also under immense pressure to secure grants and publish in high-impact journals. This “publish or perish” culture incentivizes researchers to pursue trendy, marketable topics rather than asking tough questions or investigating less profitable areas. The result is a research agenda driven more by financial considerations than by genuine scientific inquiry or patient needs.
The STARD Scandal: A Prime Example*
The STARD study is a prime example of how this corrupted process fails patients. STARD was a massive research initiative that appeared to demonstrate the effectiveness of antidepressant medications. Funded by the National Institute of Mental Health and conducted by leading academic psychiatrists, it was hailed as definitive proof that antidepressants work.
However, a re-analysis of the STARD data revealed serious problems. The study’s definition of “response” was unacceptably broad, the criteria for remission were changed midway through the study, and participants who dropped out due to lack of efficacy were not included in the final analysis. When these issues were corrected for, the effectiveness of antidepressants looked much less impressive.*
Despite these flaws, the initial, inflated results of STARD were widely publicized and used to guide treatment for years. Millions of patients were prescribed antidepressants based on faulty data, while alternative therapies were sidelined. The STARD scandal illustrates how even the most influential and seemingly rigorous studies can be manipulated to serve industry interests, misleading doctors and harming patients.
The Marginalization of Psychotherapy
The bias towards pharmacological interventions and against psychotherapy is another consequence of the profit-driven model of medical research. Drug companies have no incentive to fund studies on non-pharmacological treatments, so research into these interventions lags behind.
Moreover, the kind of research that is done on psychotherapy often fails to capture what makes it effective. Randomized controlled trials, the gold standard of medical research, are ill-suited to studying the highly personal, context-dependent process of psychotherapy. By trying to standardize and manualize therapy for the sake of research, we risk losing the very elements that make it powerful – the therapeutic relationship, the flexibility to adapt to individual needs, and the space for intuition and creativity.
As a result, many of the most effective forms of psychotherapy, particularly for complex conditions like trauma and personality disorders, remain understudied and underutilized. Patients are deprived of potentially life-changing treatments, while being over-prescribed medications that may be ineffective or even harmful.
The Human Cost of a Broken System
The ultimate consequence of this broken system is the suffering of patients. When research is biased, treatments are ineffective, and patient voices are ignored, people are harmed. They are subjected to unnecessary side effects, deprived of effective therapies, and left to struggle with chronic conditions that could be alleviated with proper care.
My own story is just one example among millions. How many other patients have been dismissed, gaslit, or harmed because their experiences didn’t align with the supposed “evidence”? How many have been denied the treatments they need because those treatments aren’t profitable enough to research? How many have suffered needlessly because the system prioritizes money over human wellbeing?
The Way Forward: Recentering Ethics, Transparency, and Patient Voice
Fixing this broken system will require a radical reshaping of the incentive structures and power dynamics in medical research. We need to:
- Strengthen conflict of interest regulations and enforce real consequences for violations.
- Demand transparency in research funding, study design, and data analysis.
- Prioritize funding for independent research driven by scientific merit and patient need, not profit potential.
- Reform academic incentives to reward clinical impact and patient outcomes, not just publication metrics.
- Integrate patient voices and real-world clinical evidence into the research process.
- Broaden our definition of “evidence” to include qualitative, experiential data alongside quantitative measures.
- Invest in research on non-pharmacological interventions, including psychotherapy, lifestyle changes, and complementary medicine.
Most importantly, we need to re-center ethics and patient wellbeing as the guiding principles of medical research and practice. We must never forget that behind every data point is a human being, and that our ultimate duty is to alleviate suffering and improve lives.
The Path Ahead
The failures of evidence-based medicine, as illuminated by my own journey through chronic illness, are not just academic concerns. They have real, often devastating consequences for patients. The corruption of medical research by profit motives, the narrowing of what counts as “evidence,” and the silencing of patient voices have created a system that too often fails to deliver real healing.
But change is possible. By speaking out, by demanding accountability, and by advocating for a patient-centered, ethically grounded approach to research and care, we can build a medical system that truly serves those it purports to help. It won’t be easy, and it will require challenging entrenched interests and ways of thinking. But the stakes – the health and wellbeing of millions – could not be higher.
As we move forward, let us remember the human faces behind the numbers, the real lives impacted by the choices we make in medicine. Let us have the courage to question dogma, to value lived experience alongside empirical data, and to always, always put patients first. Only then can we build an evidence base and a healthcare system worthy of the trust patients place in us. The future of medicine, and the lives it touches, depend on it.
Read More About Evidence Based Practice and Research Psychology:
Lessons from the STAR*D Scandal
The Corporatization of Healthcare
Incentives in Evidence Based Practice
Psychotherapy is Indivisible form Philosophy and Anthropology
The Broken Incetives in Research and Clinical Practice
Healing The Modern Soul Series Part 1 Part 2 Part 3 Part 4 Healing the Modern Soul Appendix













0 Comments