A Revolutionary Approach to Mental Health
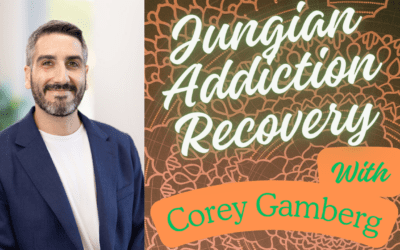
In a groundbreaking interview between Joel Blackstock and Adam O’Brien, founder of the Wounded Healer Institute, we explore the profound interconnections between dissociation, trauma, and addiction that challenge conventional psychiatric approaches. This comprehensive discussion offers mental health professionals, individuals experiencing dissociation, and anyone interested in alternative healing approaches a fresh perspective on understanding and treating complex psychological conditions.
The Limitations of the Biomedical Model in Modern Psychiatry
Why Traditional Approaches Fall Short
The conversation begins with a critical examination of the biomedical model’s dominance in mental health treatment. Both Blackstock and O’Brien express concerns about the overreliance on quantitative data at the expense of qualitative lived experience. This reductionist approach, they argue, fails to capture the complexity of human psychological experience, particularly when dealing with dissociation and trauma.
O’Brien emphasizes that the current system’s logic is heavily influenced by legal, banking, and insurance requirements rather than genuine therapeutic effectiveness. This has created a framework where diagnostic processes for dissociative disorders can take years, leaving individuals without proper support during critical periods of their healing journey.
The Hierarchy Problem in Mental Health Research
A significant issue raised is the artificial hierarchy between quantitative and qualitative research in psychology. O’Brien points out that while empirical data has its place, the dismissal of qualitative experience as “less scientific” undermines our understanding of psychological phenomena. This bias has led to the labeling of effective therapeutic approaches as “pseudoscience” simply because they don’t fit neatly into randomized controlled trial frameworks.
The Body as the Psychological Unconscious: A Paradigm Shift
Understanding the Mind-Body Connection
One of the most profound insights from the interview is O’Brien’s assertion that “the physical body is the psychological unconscious.” This perspective challenges the traditional separation of mind and body in Western medicine and psychology. According to this view, trauma, dissociation, and emotional experiences are not just stored in the brain but throughout the entire body system.
This understanding has significant implications for treatment. Rather than focusing solely on cognitive approaches, effective therapy must address the somatic experience of trauma and dissociation. The body holds memories, particularly preverbal experiences, that cannot be accessed through traditional talk therapy alone.
The Role of Natural Healing Systems
O’Brien discusses the fascinating connection between dissociation and the body’s natural opioid and cannabinoid systems. These endogenous systems, designed for healing and regulation, play a crucial role in how we respond to trauma and pain. Understanding this connection provides a biological framework for why certain individuals may be more prone to both dissociation and addiction.
Dissociation as a Primary Response Mechanism
Beyond Pathology: Understanding Dissociation as Adaptation
The interview challenges the purely pathological view of dissociation. O’Brien introduces the concept of “skilled dissociation,” acknowledging that dissociative experiences exist on a spectrum and can serve protective functions. This nuanced understanding moves away from viewing dissociation solely as a disorder to recognizing it as a primary response mechanism to overwhelming experiences.
The Connection Between Dissociation and Addiction
Blackstock shares clinical observations about the intrinsic link between dissociation and addiction. He notes that individuals often need to be familiar with dissociated states to comfortably engage with the effects of substances. This insight suggests that addiction treatment must address underlying dissociative tendencies for lasting recovery.
O’Brien’s research indicates that addiction is transdiagnostic, similar to how dissociation has recently been recognized. This means that both phenomena cut across traditional diagnostic categories, appearing in various forms throughout different mental health conditions.
Innovative Therapeutic Approaches for Dissociation and Trauma
Brainspotting: Accessing Preverbal Trauma
A significant portion of the discussion focuses on Brainspotting, a therapeutic modality that both practitioners find particularly effective for addressing dissociation and preverbal trauma. Unlike traditional talk therapy, Brainspotting works with the body’s natural healing mechanisms and can access experiences stored before language development.
O’Brien explains that Brainspotting allows therapists to work with parts of the self that may be non-verbal or difficult to access through conventional means. This approach recognizes that complex trauma often stems from experiences that occurred before the development of explicit memory and language.
The Importance of Dual Attunement
Blackstock introduces the concept of dual attunement, where the therapist maintains awareness of both their own internal state and the client’s experience. This approach is crucial when working with dissociative clients, as it helps create a safe container for processing intense experiences while preventing therapist overwhelm or secondary trauma.
Integrating Multiple Modalities
The interview highlights the value of integrating various therapeutic approaches. Blackstock mentions combining Brainspotting with Emotional Transformation Therapy (ETT), while O’Brien discusses the use of neurofeedback and QEEG brain mapping. This integrative approach recognizes that complex conditions require flexible, multifaceted treatment strategies.
Critical Analysis of Current Treatment Approaches
The Ketamine Controversy
Both practitioners express serious concerns about the use of ketamine for treating dissociative disorders. As O’Brien points out, ketamine is categorically a dissociative drug, making its use for dissociation treatment counterintuitive and potentially harmful. This critique highlights the importance of understanding the mechanisms of action of treatments rather than simply following trends in psychiatric medication.
Problems with Diagnostic Processes
The current diagnostic system comes under scrutiny for its lengthy and often traumatizing assessment processes. O’Brien questions why it should take years to diagnose dissociative disorders when the symptoms are often clearly present. This delay in diagnosis can prevent individuals from receiving appropriate treatment and understanding their experiences.
The Dismissal of Alternative Approaches
The interview addresses how effective therapeutic approaches are often dismissed using terms like “apophenia” or “pseudoscience” without proper investigation. This dismissal often comes from professionals who have limited understanding of the modalities they’re critiquing, as illustrated by Blackstock’s example of medical professionals dismissing Brainspotting based on outdated theories of memory.
The Wounded Healer Institute: A New Model for Mental Health
Community-Based Healing
O’Brien introduces the Wounded Healer Institute as a revolutionary approach to mental health support. This model recognizes that individuals who have navigated their own healing journeys often have unique insights and skills to offer others. The institute aims to create a supportive community where lived experience is valued alongside professional training.
Skill Sharing and Peer Support
The institute emphasizes skill sharing and peer support as essential components of healing. This approach acknowledges that healing happens in community and that individuals with similar experiences can offer understanding and support that traditional therapy alone cannot provide.
Redefining the Healer Role
O’Brien advocates for recognizing “healer” as a distinct profession based on trauma resolution training and lived experiences with altered states of consciousness. This challenges the traditional gatekeeping in mental health professions and opens possibilities for more diverse and effective healing approaches.
Hidden Addictions and Overlooked Patterns
Beyond Substance Use
The conversation expands the understanding of addiction beyond substance use. O’Brien identifies perfectionism, altruism, and ambition as potential “missing addictions” that society often rewards rather than recognizes as potentially problematic. This broader view of addiction helps explain why traditional addiction treatment may miss important aspects of addictive patterns.
The Role of Dissociation in Behavioral Patterns
Understanding how dissociation underlies various behavioral patterns provides a new lens for viewing seemingly disparate issues. Whether it’s workaholism, compulsive helping, or relentless achievement seeking, these behaviors may serve similar functions to substance use in managing dissociative states.
The Historical Context of Mental Health Treatment
Learning from the Past
O’Brien emphasizes the importance of understanding the historical context of mental health treatment. The anti-psychiatry movement, the rise of psychopharmacology, and shifts in cultural attitudes toward mental health have all shaped current practices. This historical awareness helps identify patterns of overcorrection and missed opportunities in treatment approaches.
Ancient Wisdom and Modern Science
The interview touches on the historical use of psychedelics and plant medicines in healing traditions. Rather than dismissing these practices as primitive, O’Brien suggests that ancient wisdom traditions understood aspects of consciousness and healing that modern psychiatry is only beginning to rediscover.
Practical Implications for Treatment
Addressing Dissociation First
A key clinical insight is that dissociation must be addressed before other therapeutic goals. As Blackstock notes, therapeutic objectives often shift as clients become less dissociated and more aware of their emotional experiences. This sequencing is crucial for effective treatment planning.
Working with Non-Verbal Parts
The interview provides practical guidance for working with non-verbal or preverbal parts of the self. O’Brien’s approach assumes all parts are present and can be communicated with, even if not through traditional verbal means. This requires therapists to develop sensitivity to non-verbal cues and somatic communications.
The Importance of Body Awareness
Both practitioners emphasize the importance of bringing clients back into body awareness. While this process may initially increase discomfort as individuals reconnect with held pain, it’s essential for genuine healing. The body’s wisdom and natural healing capacities can only be accessed through embodied presence.
The Future of Mental Health: Integration and Innovation
Moving Beyond Either/Or Thinking
The conversation advocates for moving beyond rigid either/or thinking in mental health. Rather than choosing between medical and alternative approaches, the future lies in intelligent integration that honors both scientific rigor and lived experience.
The Need for Systemic Change
O’Brien and Blackstock agree that systemic change is needed in how mental health services are conceptualized and delivered. This includes challenging insurance-driven treatment models, reconsidering diagnostic frameworks, and creating space for innovative approaches that don’t fit traditional categories.
Hope for Transformation
Despite critiques of current systems, the interview maintains a hopeful tone about the future of mental health treatment. O’Brien expresses optimism about psychology and legal systems eventually recognizing the science of qualitative experience and the potential for profound healing.
A Call for Compassionate Innovation
This comprehensive discussion between Joel Blackstock and Adam O’Brien offers a roadmap for reimagining mental health treatment. By recognizing the interconnections between dissociation, trauma, and addiction, and by valuing both scientific understanding and lived experience, we can create more effective and compassionate approaches to healing.
The Wounded Healer Institute represents one model for this integration, but the broader message is clear: healing happens when we honor the whole person, including their body wisdom, lived experience, and innate capacity for transformation. As mental health professionals and as a society, we must be willing to challenge outdated paradigms and embrace innovative approaches that truly serve those seeking healing.
For individuals experiencing dissociation, trauma, or addiction, this interview offers validation and hope. Your experiences are real, your body’s responses make sense, and healing is possible when we approach these conditions with understanding, compassion, and appropriate therapeutic support.
The journey toward a more integrated and effective mental health system requires courage to question established norms and openness to learn from diverse sources of wisdom. As this interview demonstrates, some of the most profound insights come from those who have walked the path of healing themselves and are willing to share their hard-won wisdom with others.




















0 Comments