 How Therapists can Use the Pupil to Heal Trauma
How Therapists can Use the Pupil to Heal Trauma
One of the reasons that I left EMDR and started to pursue brainspotting as the primary brain based medicine that I use as a provider was because of pupil dilation. Years ago when I was just starting out as a therapist I noticed that pupil dilation patterns were a good indicator of how well a patient was processing trauma. I would use a patient’s pupil dilation and movement to see how well EMDR was working. During EMDR patients don’t talk much until the end of a cycle of eye movement. I learned that when I saw certain patterns of movement in the pupil during EMDR, that was when a patient would have a big revelation or emotional insight. When I saw the pupil tracking relatively smoothly with no movement, I knew before the patient spoke that the EMDR was not working and that we needed to adjust the target or framing of the treatment to try again.
I was actually doing a treatment similar to brainspotting for about three months before I knew brainspotting existed. I immediately noticed as an EMDR provider that patients’ eyes would “flutter” or rapidly expand and contract the pupil, on certain spots along the EMDR movement line. It seemed like most of the neurological change was happening in these spots. I began to slow down my finger as I passed these spots that seemed to produce the most profound change. Eventually I stopped moving on these spots completely and patients entered fugue states and emerged with profound insight. I started to experiment with the distance my finger was from the eye and this seemed to make difficult and avoided memories more clear and easier for patients to process.
I was not seeing subtle movements of the pupil either. Some patients’ eyes moved so quickly between contracted and open they looked like a strobe light. Others dilated so wide that there was hardly any iris available at all and they saw strange colors and patterns. (Watch a video of what this looks like here). I told a friend of mine who is an ophthalmologist what kinds of things I was seeing in the eye and they told me those movements were not possible without a stroke or tumor. I felt confident the more than eighty patients I had seen by that point did not all have a brain tumor or stroke. Something else about how the brain processes trauma and sensory input was at play.
I looked for more and more EMDR providers to help me expand or understand this phenomenon. EMDR is very hierarchical and protocol driven. All of the trainers treated me like a heretic and told me to forget what I was noticing and return to the EMDR formula. Nevermind that patients were requesting “this” instead of EMDR even though they were not aware I was doing anything new. Never mind that patients who had benefited and completed EMDR protocol felt this new technique was leading them to new layers of understanding and healing that EMDR alone did not produce. I felt overwhelmed and alone. I had been a therapist for about three months at that point
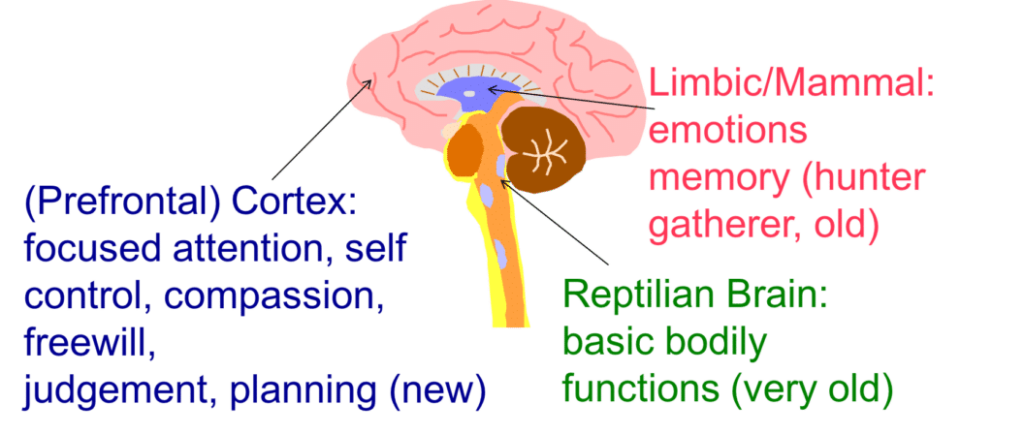
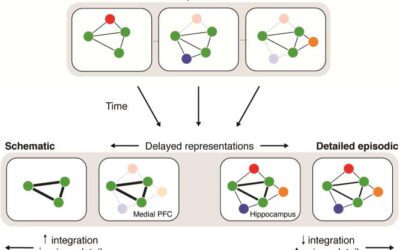
My understanding at the time was that trauma was a “stuck” memory in the subcortical and somatic brain. The body remembered the somatic re-experiencing of the traumatic event even though the rational and intellectual part of the brain knew that it was over. These traumatic, somatic associations affected posture, muscle tension, motion and mood, even though patients were not always intellectually aware of them. Different parts of the brain remember things in different ways, as they serve different functions. Traumatic experiences make implicit memory centers that govern emotion, kinesthetic, and somatic experience cling to physical memories not integrated with what the intellectual and conscious emotional brain is doing.
It made sense to me then that the eye might also “remember” where it was looking during a trauma and the brain might associate eye positions with somatic, traumatic memories. These associations could have been created all at once, like the patient that watched his friend’s car explode from an IED. They could also be created in layers of association overtime, like the numerous patients who remembered staring down at the floor or inside a classroom when they had been yelled at by an adult as children. QEEG brainscans have revealed that childhood trauma shows up in the brain similarly to ADHD, and inflammatory and chronic pain conditions like fibromyalgia.
What is Brainspotting?
I was insecure because patients were now exclusively requesting this “new” technique but I did not know what it was. After asking many peers a fellow therapist told me that what I was doing sounded like something called Brainspotting, invented by Dr. David Grand. When I spoke to David Grand,he said that he was also an EMDR professional who had followed his own intuition to create brainspotting and leave EMDR behind when he saw the same cues in the eye that I had followed.
Dr. Grand told me that I needed to experience the technique I was practicing myself at a brainspotting training, which I soon did. Brainspotting is an experiential therapy that practitioners learn how to do by going through themselves. I am enormously grateful that there was a body of academic work done by Dr. Grand and his collaborators that I was able to stumble upon and learn from. I would never have been able to develop the nuance and intricacy of the brainspotting technique on my own.
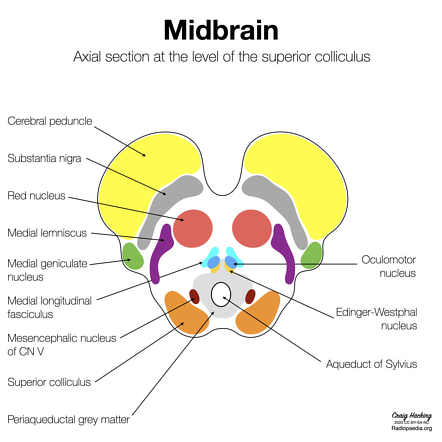
Now that the science of brainspotting has advanced for more than two decades it has discovered lots of tricks. Brainspotting stimulation with one eye covered means that the brain will have to pull associations from a traumatic experience from one side of the brain and allow for integration with the other brain hemisphere. This helps the midbrain “get on the same page” with what the subcortical brain used to be feeling in isolation. This is one example but there are literally hundreds of tricks brainspotting practitioners have found.
What is Emotional Transformation Therapy (ETT)?
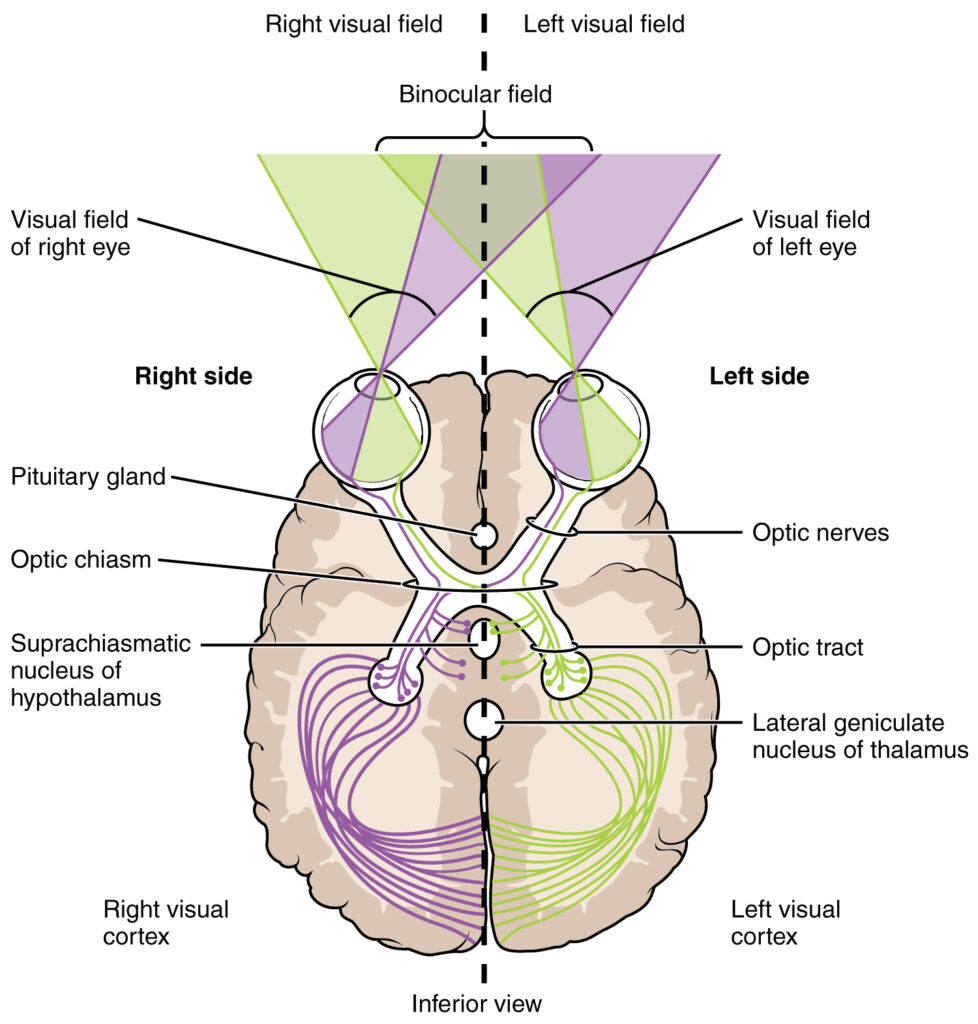
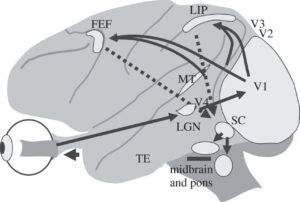
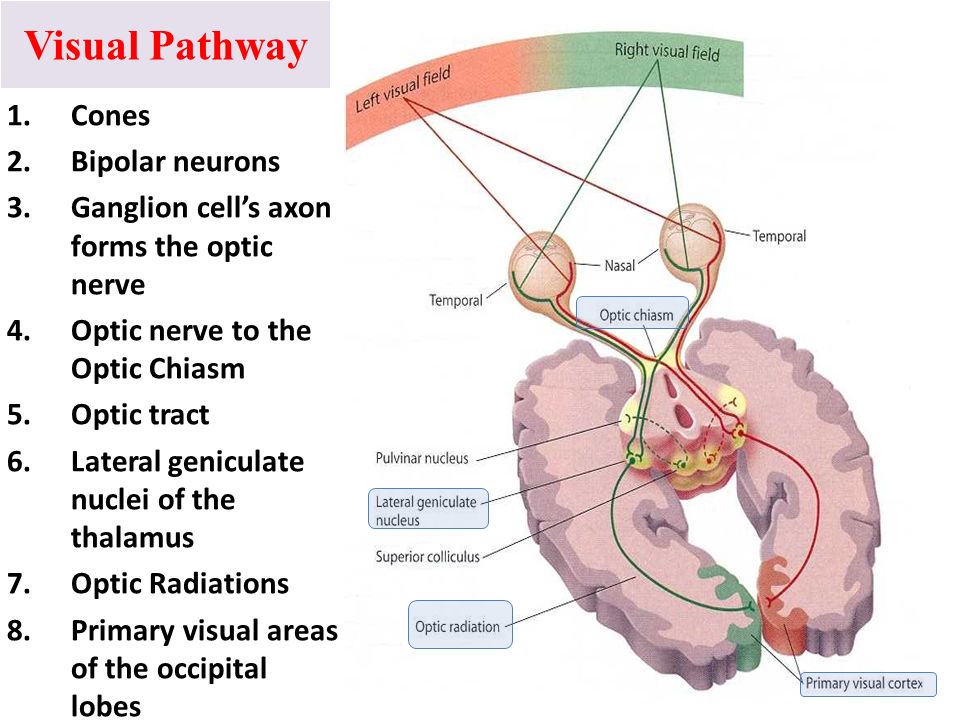
 Looking for fast and effective scientific modalities also led me to Emotional Transformation Therapy, developed by Dr. Steven Vazquez. Dr. Vasquez’s technique uses color, light direction, frequency and hue to integrate traumatic memory. The visual pathway’s through the brain connects directly to the oldest parts of our brain with the deepest wiring to the body and most unconscious or implicit memories. Other senses travel through more modern additions to the brain in the mid and frontal structure. This is one of the reasons that visual stimuli is such a powerful tool for profound emotional change and healing.
Looking for fast and effective scientific modalities also led me to Emotional Transformation Therapy, developed by Dr. Steven Vazquez. Dr. Vasquez’s technique uses color, light direction, frequency and hue to integrate traumatic memory. The visual pathway’s through the brain connects directly to the oldest parts of our brain with the deepest wiring to the body and most unconscious or implicit memories. Other senses travel through more modern additions to the brain in the mid and frontal structure. This is one of the reasons that visual stimuli is such a powerful tool for profound emotional change and healing.
I’m now the second person in the state of Alabama trained in ETT, and the only one trained in EMDR, Brainspotting, and ETT that I have been able to find in the world. I hope learning these established brain based medicines can pave the way to new discoveries and the future of the psychotherapy profession.
Beyond the eye movement section ETT contains many other brain based medicine techniques that use the retina. ETT modules include a light device that can recreate specific hues, flicker rate frequency’s, and light directions. There are color wands that use eye position with specific colors to keep certain kinesthetic mid brain networks active during eye movement. There are goggles that use light direction to hypothetically interrupt pain and mood blocks in the stellate ganglia. There is also a color chart that can immediately detect dissociation. These techniques are not heavily evidence based yet, yet they were developed based on Dr. Vazquez’s review of thousands of studies on how the eyes process stimuli and how it affects brain function. Tens of thousands of providers and patients have experienced and vouch for these techniques as well.
What happens in the Brain during ETT, Brainspotting, or EMDR?
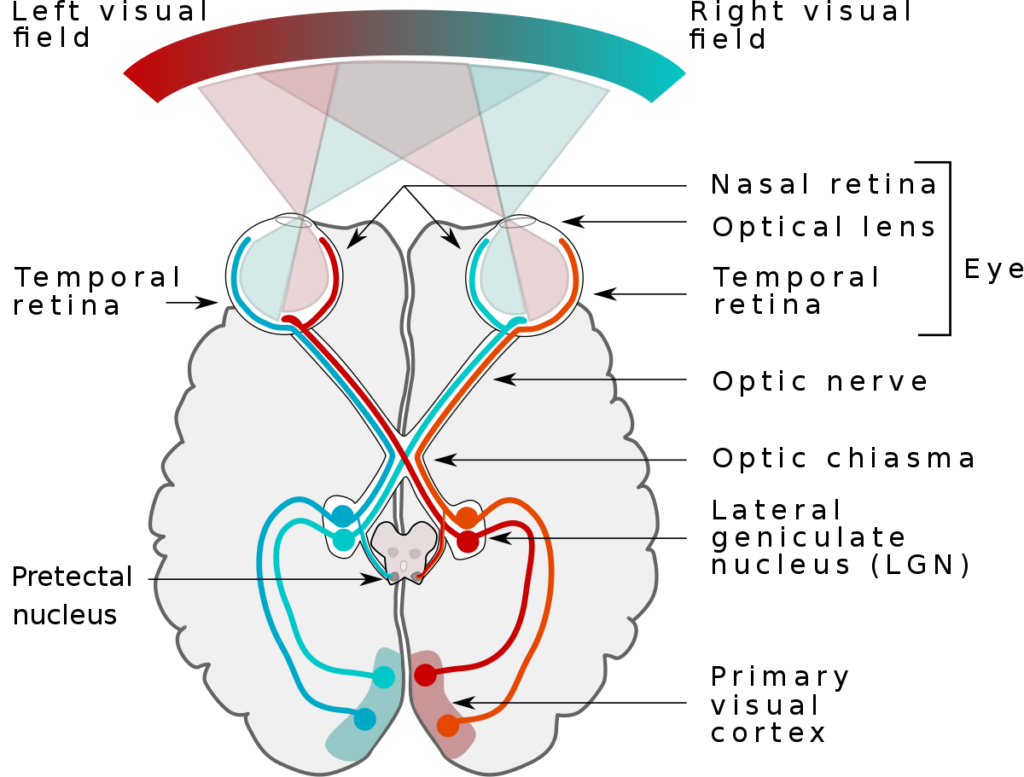
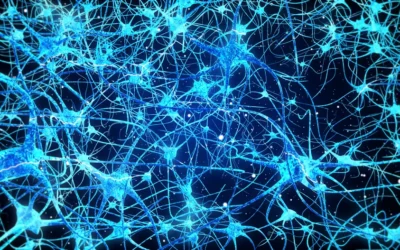
The human eyes, often overlooked for their complexity, play a pivotal role beyond mere vision. I would argue that we should think of eyes as extensions of the brain. Extensive scientific research has unraveled the intricate neural pathways that light-initiated impulses follow through the nervous system, influencing a wide range of brain functions. Surprisingly, there are three major neural pathways responsible for transmitting these impulses, affecting nearly every significant aspect of brain activity. By manipulating factors like wavelength, light angle, brightness, light direction, psychological state, exposure duration, and strobe rate, one can direct these impulses to specific brain functions, ultimately impacting emotional and somatic regulation.
The First Pathway: Integrating Visual Functions
Photoreceptor cells in the eyes convert light into electrical impulses, creating a connection between vision and various non-visual functions. This pathway blends visual experiences with auditory and movement functions, eye orientation, and general spatial awareness.
 The Second Pathway: Sensory Integration and Regulation
The Second Pathway: Sensory Integration and Regulation
This pathway begins with the lateral geniculate nucleus in the thalamus, which selects visual information to relay to the visual cortex. The visual cortex, the brain’s largest sensory area, then communicates with three major integration centers: the hypothalamus, controlling the autonomic nervous system and various bodily functions, and the pineal gland, overseeing hormones, the immune system, and more. Light exposure impacts our physiological rhythms and the “biological clock,” called the suprachiasmatic nucleus.
The Third Pathway: Broad Impact on Brain Functions
This pathway accesses previously mentioned brain functions and stimulates the brain stem, general arousal, the central nervous system, and emotions.It offers an alternative route to influence mid-brain and hypothalamus activity.
Visual Pathways and Pupil Movement
For over a century, only rod and cone cells were recognized as photosensitive in the eyes.
In the 90s new visual stimuli cells were discovered in mice, responsible for regulating circadian rhythms. In the 2000’s a new cell, the Retinal Ganglion Cell, was identified in humans. These cells are activated mainly by blue light. They transmit impulses to the hypothalamus and the mid-brain’s olivary nucleus, affecting pupil size and other behaviors.
These cells are associated with sleep regulation through melatonin, control energy and mood through glutamate release and the availability of neurotransmitters through pituitary adenylate polypeptide. These visual cells control far more in the body and brain than what we see. These neural pathways play a vital role in brain function and are a rapid and poorly understood pathway for trauma treatment.
What can pupil dilation teach us?
 The language of the pupil taught both me and Dr. Grand that there was more to the brain than the EMDR procedure made room for. Is there more that the pupil has to teach us about trauma and the brain? I think so. Whenever I encounter someone that had no results in brainspotting I always ask them what the sessions were like. I have never met a brainspotting non responder who did sessions with a brainspotting provider that was using the pupil to find spots. Patients who had negative experiences with brainspotting have all reported to me that their provider moved the pointer to different places and asked the patient what they felt for several sessions until the patient didn’t go back.
The language of the pupil taught both me and Dr. Grand that there was more to the brain than the EMDR procedure made room for. Is there more that the pupil has to teach us about trauma and the brain? I think so. Whenever I encounter someone that had no results in brainspotting I always ask them what the sessions were like. I have never met a brainspotting non responder who did sessions with a brainspotting provider that was using the pupil to find spots. Patients who had negative experiences with brainspotting have all reported to me that their provider moved the pointer to different places and asked the patient what they felt for several sessions until the patient didn’t go back.
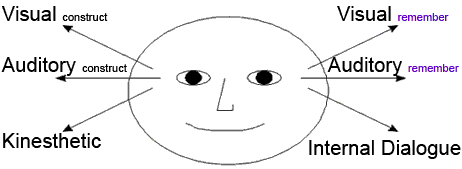
Francine Shapiro (EMDR), David Grand (Brainspotting), and Steven Vazquez (ETT) were not the first to connect the relationship between emotion and the pupil. Danie Beaulieu (EMI) used eye movement to heal patients’ trauma in the 1970s before EMDR when she created eye movement integration. . Richard Bandler and John Grinder, the creators of Neuro-Linguistic Programming (NLP), developed the concept of NLP “eye cues” through their observations of various therapists and their techniques. They did not base NLP eye cues on the work of a single individual but rather drew inspiration from several sources, including the work of Virginia Satir (a family therapist), Fritz Perls (the founder of Gestalt therapy), and Milton H. Erickson (a renowned hypnotherapist)
Bandler and Grinder’s approach involved studying the language patterns and non-verbal cues used by these successful therapists and modeling their techniques. This modeling process led to the development of NLP, which encompasses various tools and techniques, including the observation of eye movements or eye accessing cues.
To my knowledge there is no official record or mention of it. However, I have heard from several older therapists that Bandler (NLP), Shapiro (EMDR), and Beaulieu (EMI) attended the same somatic medicine conferences and discussed eye movement to treat trauma and how pupil dilations that could indicate trauma was present for several years before they created their own models. The idea of using eye movement in therapy has been around a long time. The confusion and disagreements come down to what the most effective metric and techniques are.
What do pupil dilations tell us about the brain?
Pupil Dilations and Movement are Windows into Brain Function
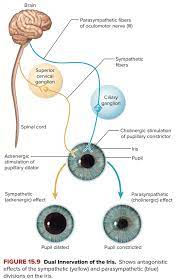
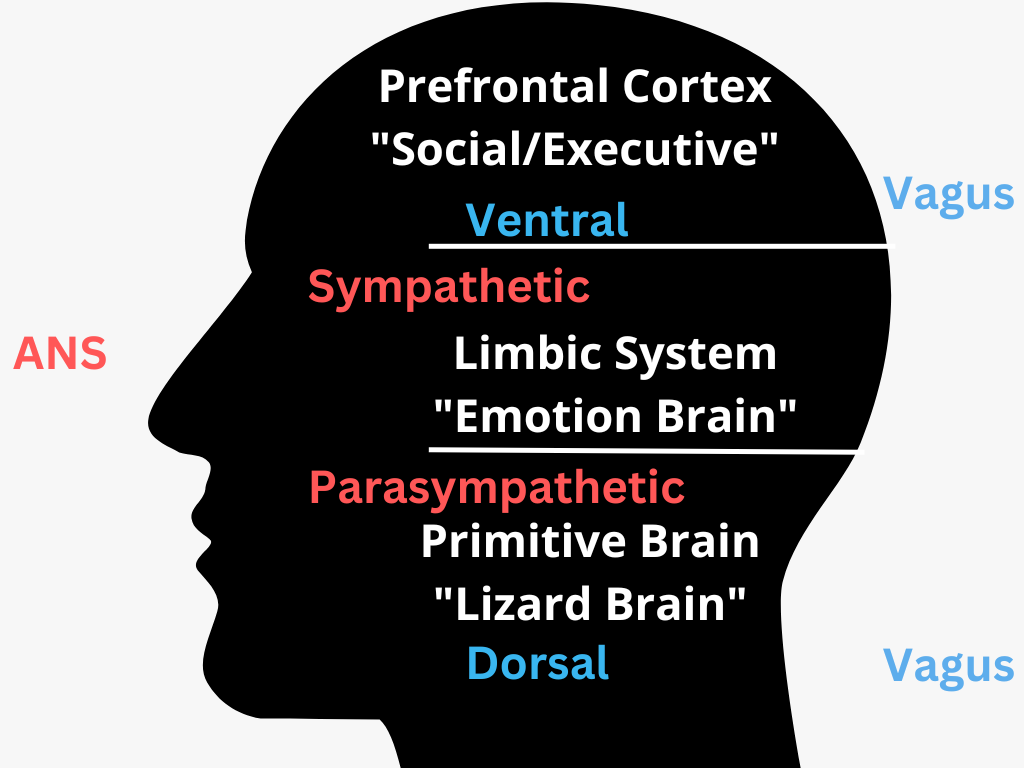
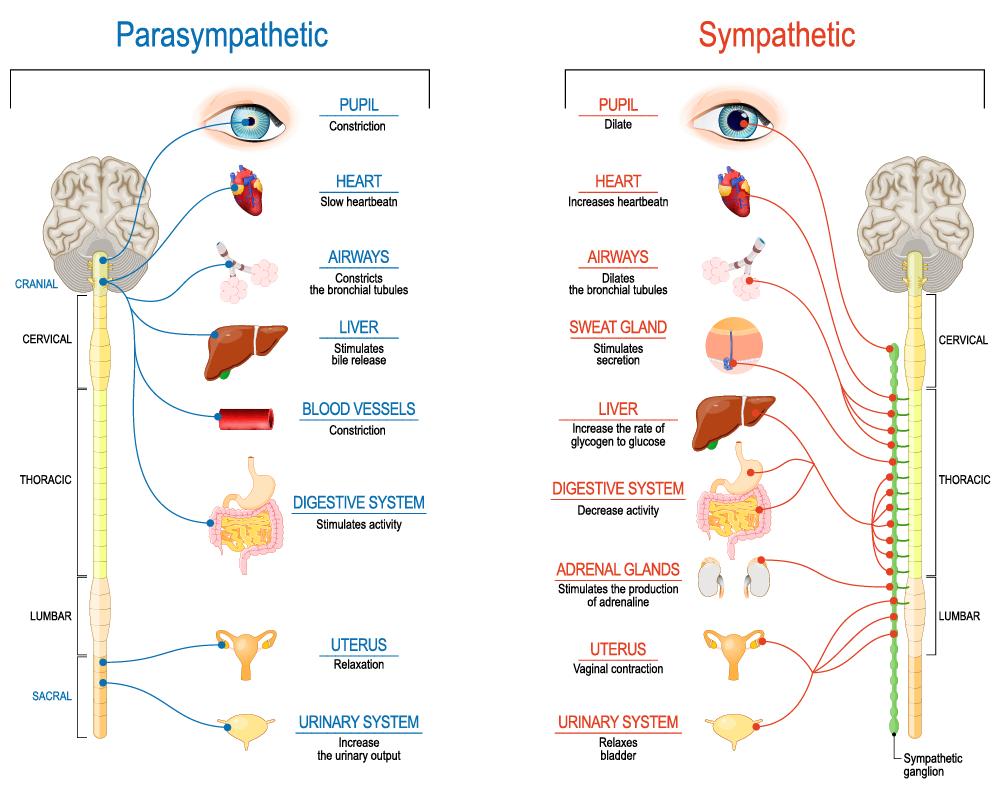
The human eye, often called the “window to the soul,” gives us our most . Pupil dilation gives us one of the most immediate and simple ways to glimpse brain function. We have long known that pupil dilation and movement, are controlled by the autonomic nervous system (ANS), have the potential to reveal valuable insights into the type of brain activity occurring.
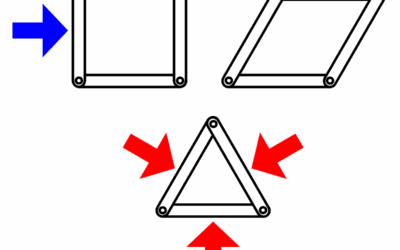
Can the Sympathetic and Parasympathetic Nervous Systems go “out of sync”
The parasympathetic and sympathetic nervous systems can indeed become unbalanced or dysregulated, leading to a state where they appear to be “out of sync.” Both of these systems are part of the autonomic nervous system, which controls involuntary bodily functions such as heart rate, digestion, respiratory rate, pupillary response, urination, and sexual arousal.
The sympathetic nervous system is responsible for the body’s fight-or-flight response, triggering the release of stress hormones like adrenaline and cortisol. This response prepares the body to react to perceived threats by increasing heart rate, dilating the pupils, and redirecting blood flow to the muscles to enhance physical strength and reaction time. On the other hand, the parasympathetic nervous system is responsible for the body’s rest-and-digest response, promoting relaxation, slowing the heart rate, and aiding in digestion.
When these systems are not properly regulated, it can lead to various health issues. For instance, chronic stress can cause an overactive sympathetic nervous system, leading to persistent high blood pressure, increased heart rate, and heightened anxiety. Over time, this can contribute to the development of cardiovascular diseases, gastrointestinal issues, and compromised immune function.
Conversely, an underactive parasympathetic nervous system can result in poor digestion, low heart rate variability, and inadequate stress recovery. This can leave individuals feeling fatigued, mentally exhausted, and more susceptible to certain health problems.
Several factors can contribute to an imbalance between the sympathetic and parasympathetic nervous systems, including chronic stress, trauma, poor sleep, unhealthy lifestyle choices, and certain medical conditions. Techniques such as mindfulness practices, deep breathing exercises, regular physical activity, and stress-reduction strategies can help restore balance and promote the overall well-being of the autonomic nervous system. If you suspect an imbalance, consulting a healthcare professional for a comprehensive assessment and guidance is advisable.
Can Brain Based Medicines regulate and “resync the parasympathetic and sympathetic nervous systems?
Various therapeutic approaches, including Brainspotting, meditation, yoga, Emotional Transformation Therapy (ETT), Eye Movement Desensitization and Reprocessing (EMDR), and Neuro-Linguistic Programming (NLP) eye cues, have shown promise in helping individuals heal from trauma and regulate their nervous systems. While each method operates differently, they often aim to facilitate emotional regulation, reduce the impact of traumatic memories, and promote overall well-being.
Brainspotting:
This therapeutic technique involves identifying specific eye positions to access and process unresolved trauma and distress. By focusing on these “brainspots,” individuals can promote deep self-healing and address the neurological imprints of trauma. It is believed to work by accessing the subcortical brain where traumatic experiences are stored.
Meditation and Yoga:
These practices can help regulate the nervous system by promoting relaxation, reducing stress, and increasing mindfulness. They have been shown to positively impact emotional well-being and reduce symptoms of anxiety and depression. Mindfulness-based practices can enhance emotional regulation and help individuals develop a healthier relationship with their thoughts and feelings.
Emotional Transformation Therapy (ETT):
ETT combines elements of traditional psychology with techniques like color light therapy to address emotional distress and trauma. By integrating the use of visual stimulation and emotional focus, ETT aims to facilitate emotional healing and promote overall psychological well-being.
Eye Movement Desensitization and Reprocessing (EMDR):
EMDR utilizes bilateral stimulation, such as eye movements, to help individuals process traumatic memories and associated negative emotions. It enables individuals to reprocess distressing memories in a way that reduces their emotional intensity and facilitates the development of adaptive coping mechanisms.
Neuro-Linguistic Programming (NLP) Eye Cues:
NLP techniques, including the use of eye cues, aim to reframe thought patterns and behaviors to promote positive changes in emotional responses. By recognizing and modifying unconscious patterns of thought and behavior, individuals can work toward resolving emotional trauma and developing healthier cognitive processes.
Is using pupil dilation to detect brain function evidence based?
Oddly industries other than mental health are more likely to trust the science between pupil dilation and movement. Silicon valley companies trust it with billion dollar deliverables, advertising companies trust it with multi million dollar ad campaigns and movie studios trust it with summer blockbusters. Dr. Clotaire Rapaille was one of the pioneers of helping ad and tech companies tap into the pupil to see a customer’s emotional connection to their brand.
Have you ever wondered why every movie trailer has shots of extreme emotion in close ups on faces, explosions, screams and fire? Well that is because thousands of hours of footage was used to see what made test audiences eyes dilate the most. The findings were shots of eyes, shots of fire, and shots of extreme emotion like screaming produced the strongest pupillary reaction. Google and other GUI designers use eye tracking to design interfaces that represent the way the eyes seek information naturally. Advertising companies study the potential effect of different ads by seeing if focus groups have emotional reactions to the product with pupillometry.
We have understood that pupil movement and dilation corresponds to pupil dilation’s link to emotion has practical uses in various fields. In the entertainment industry, movie studios often screen trailers to test audiences while monitoring their pupil dilation to gauge emotional reactions. This helps filmmakers refine their marketing strategies and identify the most captivating scenes to include in trailers. Additionally, market researchers and advertisers use pupillometry to evaluate consumer reactions to advertisements and product packaging, enabling them to create more appealing and emotionally engaging campaigns.
How does brain function affect the pupil?
 Pupil Dilation and the Sympathetic System
Pupil Dilation and the Sympathetic System
The sympathetic nervous system is responsible for the body’s “fight or flight” response during stress or perceived threats. When the brain detects danger or excitement, it activates the sympathetic system, which, in turn, affects pupil dilation:
Sympathetic Preganglionic Neurons:
These neurons, located in the spinal cord, transmit signals to the sympathetic ganglia. When activated, they stimulate the release of acetylcholine, initiating pupil dilation.
Sympathetic Ganglia:
These are clusters of neurons located outside the spinal cord. They relay signals from preganglionic neurons to postganglionic neurons. Activation of sympathetic ganglia leads to a rapid dilation of the pupils.
Sympathetic Postganglionic Neurons:
These neurons release norepinephrine, which contracts the muscles of the iris, causing pupil dilation. This process enhances visual perception, allowing for better detection of potential threats.
Modern and Primitive Parasympathetic Brain Functions
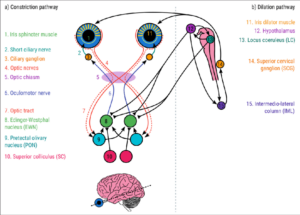 Modern Parasympathetic Function:
Modern Parasympathetic Function:
This response is associated with relaxation and recovery. When the brain activates the modern parasympathetic preganglionic neurons, it leads to smooth and controlled constriction of the pupils. Pupil movement is gradual and reflects a calm and relaxed state.
Primitive Parasympathetic Function:
The primitive parasympathetic response, often referred to as the “freeze” response, is associated with intense stress or trauma. During this response, the brain may send mixed signals to preganglionic neurons, resulting in irregular pupil fluctuations. Pupil dilation and constriction may occur abruptly and unpredictably.
Interpreting Brain Function Through Pupil Dilation and Movement
The key to using pupil dilation and movement to indicate brain function lies in pattern recognition and analysis. By tracking and analyzing these patterns, researchers and clinicians may be able to make educated hypotheses about the state of the autonomic nervous system and the brain:
High-Stress Situations:
Rapid and pronounced pupil dilation might suggest heightened sympathetic activity, indicating that the brain is responding to stress or a perceived threat.
Relaxation and Calmness:
Gradual, smooth pupil constriction may signify the dominance of the modern parasympathetic system, indicating a state of relaxation and calm.
Traumatic Events:
Irregular fluctuations in pupil size, including moments of rapid dilation and constriction or back and forth “jitter”, could be indicative of primitive parasympathetic responses triggered by traumatic events.
How can Clinicians Use the Pupil During Brainspotting or ETT
Changes in pupil size and activity could provide insights into a patient’s brain function, thought processes, or emotional state, although this field is still evolving, and the interpretations may vary depending on the specific context and individual variability. Here are some hypothetical scenarios on how pupillometry could be used:
Emotional State Assessment:
- Positive vs. Negative Emotions: Pupillometry might distinguish between positive and negative emotions. Research suggests that positive emotions could lead to different patterns of pupil responses compared to negative emotions. For instance, increased pupil dilation might correlate with excitement or joy, while smaller pupils might relate to sadness or fear.
- Intensity of Emotion: The degree of pupil dilation might correspond to the intensity of an emotional response. Larger dilation might indicate stronger emotions, while smaller changes may suggest milder emotional reactions.
Cognitive Load and Thought Processes:
Cognitive Load:
- Pupillometry could potentially reflect cognitive load. Higher cognitive demand or mental effort, such as solving complex problems or deep thinking, might be associated with larger pupils. Conversely, relaxed or low-cognitive-load situations could lead to smaller pupils.
Working Memory:
- Changes in pupil size might indicate the engagement of working memory. When someone is actively holding information in their working memory, their pupils could dilate as the cognitive load increases.
Brain Function and Task Performance:
Attention and Focus:
Pupillometry can reflect shifts in attention. When a patient focuses on a specific task or thought process, their pupils might constrict due to increased parasympathetic activity. Sudden distractions or shifts in focus could trigger pupil dilation.
Memory Recall:
During memory recall or introspection, changes in pupil size might indicate the brain’s engagement with the retrieval process. Larger pupils could correspond to the active retrieval of detailed memories.
Autonomic Nervous System Regulation:
Sympathetic vs. Parasympathetic Dominance:
Pupil responses might also indicate the dominance of the sympathetic or parasympathetic branches of the autonomic nervous system. Sympathetic dominance could be associated with pupil dilation, while parasympathetic dominance might lead to constriction.
While the use of pupil dilation and movement to decode brain function remains hypothetical and complex, ongoing research in this field holds immense promise. Advances in technology, including high-resolution pupil tracking systems and sophisticated data analysis, may soon allow us to harness the potential of the eyes as a direct window into the mind. Understanding these patterns could revolutionize our ability to diagnose and treat conditions related to the autonomic nervous system, trauma, and emotional states, providing profound insights into the human brain and its intricate functions.
What happens in the brain to affect pupil dilation?
Pupil dilation is primarily regulated by the autonomic nervous system, specifically through the interplay of the sympathetic and parasympathetic branches. These branches work in opposition to control the size of the pupil.
Sympathetic Nervous System (Dilation):
The sympathetic nervous system is responsible for the dilation of the pupils, a process known as mydriasis. When the brain perceives a need for increased visual sensitivity, typically in response to emotional or environmental stimuli, it activates the sympathetic system. The key mechanisms involved in sympathetic-induced pupil dilation include:
Dilation of the Iris:
Reduction in Parasympathetic Activity:
Sympathetic activation also leads to the inhibition of the parasympathetic system, which normally constricts the pupil. By reducing parasympathetic input, the sympathetic system further promotes pupil dilation.
Neurotransmitters:
Neurotransmitters like norepinephrine play a role in sympathetic-induced pupil dilation. Norepinephrine is released from sympathetic nerve endings and binds to adrenergic receptors on the dilator pupillae muscles, initiating their contraction.
Parasympathetic Nervous System (Constriction):
Conversely, the parasympathetic nervous system controls pupil constriction, or miosis. When the brain perceives a need to reduce the amount of light entering the eye, such as in bright light conditions or during activities that require close-up vision, it activates the parasympathetic system. Key mechanisms involved in parasympathetic-induced pupil constriction include:
Contraction of the Sphincter Pupillae:
The parasympathetic system stimulates the sphincter pupillae muscles, which encircle the pupil in a circular fashion within the iris. When these muscles contract, they constrict the pupil, reducing its size.
Release of Acetylcholine:
The neurotransmitter acetylcholine plays a pivotal role in parasympathetic-mediated pupil constriction. Acetylcholine binds to muscarinic receptors on the sphincter pupillae muscles, initiating their contraction.
Inhibition of Sympathetic Activity:
Parasympathetic activation also inhibits the sympathetic system, preventing pupil dilation.
The balance between sympathetic and parasympathetic input to the iris determines the size of the pupil at any given moment. Various factors, including light levels, emotional responses, and cognitive processes, can influence this balance. Emotional and cognitive stimuli can trigger changes in autonomic nervous system activity, leading to alterations in pupil size. This dynamic regulation of pupil diameter is what allows researchers and clinicians to use pupillometry as a window into an individual’s emotional and cognitive states.
Emotion and Pupil Dilation:
Emotions play a significant role in pupil dilation. When a person experiences strong emotions, such as fear, excitement, or stress, their pupils tend to dilate.
This response is mediated by the autonomic nervous system, specifically the sympathetic branch, which activates the fight-or-flight response, causing the pupils to widen to allow more light into the eyes and improve visual awareness.
In brain spotting, therapists use changes in pupil size to gauge the emotional intensity of a client’s response to specific memories or thoughts. The therapist observes how the client’s pupils react during discussions or when focusing on certain points in their visual field.
Introverted Sensing and Pupil Dilation:
How Brain Spotting Can Uses Pupil Dilation:
The therapist observes the client’s eyes and pupils as they focus on these points. Any changes in pupil size, such as dilations or contractions, are considered significant and may indicate the activation and processing of emotional material.
By tracking pupil responses, therapists can identify when a client is accessing deep emotional content, allowing for precise targeting of unresolved issues and providing a pathway to healing and resolution.
In brain spotting, therapists guide clients through a process that involves tracking their own internal experiences and sensations. The therapist pays close attention to any shifts in pupil dilation as a client recalls and processes past traumas or unresolved emotions.
The process of observing and using pupil dilation in brain spotting can help clients access and release buried emotions, reduce the impact of trauma, and promote emotional healing.
A New Model for Eye Movement Therapy
Trauma makes us predisposed to addiction, damaging relationships, and predatory religious and advertising tactics. The more thoroughly and deeply we can remove trauma from our world the better. Just like talk therapy models there will never be a perfect model of eye movement or brain based medicine. We are always looking for and then testing better theoretical models in soft science. EMDR paved the way for brainspotting. ETT and brainspotting contain new nuggets of insight that can enrich each modality simultaneously. EMI and NLP contain forgotten insights and pointers.
No one modality is ever 100% correct in the assumptions that it has to make to have a theoretical framework. We are called as providers and innovators in the field of trauma to find new. After all even the worst modalities do work for some people. You would be hard pressed to find a therapy model that does nothing for no one person. Nothing works for everything despite what the zealots in this profession will tell you.
The best models work for the most amount of patients and more conditions most of the time with less room for clinician error. In my experience brainspotting works better for more people than EMDR did. In my experience ETT can help bypass conditions that might make brainspotting from working in some cases. The science cannot stop here. In fact we have noticed several other things about the pupil at Taproot Therapy Collective since we all got trained in brainspotting and I got trained in ETT. New models and new techniques are coming. Watch the pupil. Learn to build the next revolutionary thing in the world of trauma treatment.
Did you enjoy this article? Checkout the podcast here: https://gettherapybirmingham.podbean.com/
Bibliography:
- Grand, D. (2013). Brainspotting: The Revolutionary New Therapy for Rapid and Effective Change. Sounds True.
- Shapiro, F. (2017). Eye Movement Desensitization and Reprocessing (EMDR) Therapy, Third Edition: Basic Principles, Protocols, and Procedures. The Guilford Press.
- Vazquez, S. R. (2009). Emotional Transformation Therapy: An Interactive Ecological Psychotherapy. Jason Aronson, Incorporated.
- Bandler, R., & Grinder, J. (1979). Frogs into Princes: Neuro Linguistic Programming. Real People Press.
- Beaulieu, D. (2003). Eye Movement Integration Therapy: The Comprehensive Clinical Guide. Crown House Publishing.
- Rapaille, C. (2007). The Culture Code: An Ingenious Way to Understand Why People Around the World Live and Buy as They Do. Broadway Books.
- Laeng, B., Sirois, S., & Gredebäck, G. (2012). Pupillometry: A Window to the Preconscious? Perspectives on Psychological Science, 7(1), 18-27.
- Oka, S., Chapman, C. R., Kim, B., Nakajima, I., Shimizu, O., & Oi, Y. (2007). Pupil dilation response to noxious stimulation: effect of varying nitrous oxide concentration. Clinical Neurophysiology, 118(9), 2016-2024.
- Laeng, B., & Sulutvedt, U. (2014). The Eye Pupil Adjusts to Imaginary Light. Psychological Science, 25(1), 188-197.
Further Reading:
- Corrigan, F. M., & Grand, D. (2013). Brainspotting: Recruiting the midbrain for accessing and healing sensorimotor memories of traumatic activation. Medical Hypotheses, 80(6), 759-766.
- Daniels, J. K., & McFarlane, A. C. (2019). Neurobiology of traumatic stress disorders and their impact on physical health. Dialogues in Clinical Neuroscience, 21(3), 255-273.
- Einhäuser, W. (2017). The Pupil as Marker of Cognitive Processes. In Q. Zhao (Ed.), Computational and Cognitive Neuroscience of Vision (pp. 141-169). Springer Singapore.
- Nummenmaa, L., Glerean, E., Hari, R., & Hietanen, J. K. (2014). Bodily maps of emotions. Proceedings of the National Academy of Sciences, 111(2), 646-651.
- Porges, S. W. (2011). The Polyvagal Theory: Neurophysiological Foundations of Emotions, Attachment, Communication, and Self-regulation. W. W. Norton & Company.
- Schwartz, M. S., Andrasik, F., & Andrasik, F. (Eds.). (2017). Biofeedback: A Practitioner’s Guide. The Guilford Press.
- van der Kolk, B. (2015). The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma. Penguin Books.















0 Comments