Pain Reprocessing Therapy: Rewiring the Brain’s Response to Chronic Pain
Understanding the Chronic Pain Crisis
Chronic pain affects over 50 million adults in the United States alone, representing one of the most significant health challenges of our time. Unlike acute pain, which serves as a protective warning signal for tissue damage, chronic pain often persists long after any initial injury has healed—or sometimes develops without any identifiable physical cause at all. This disconnect between pain and actual tissue damage has led researchers to fundamentally reconsider how we understand and treat persistent pain conditions.
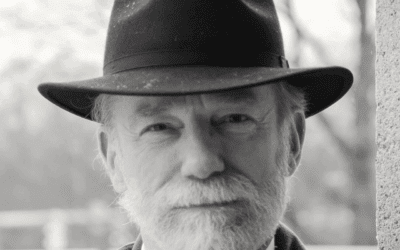
Pain Reprocessing Therapy (PRT) represents a revolutionary approach that emerged from this new understanding. Developed by Alan Gordon and refined through collaboration with neuroscientists at the University of Colorado Boulder, PRT is grounded in the recognition that chronic pain is often maintained by learned neural pathways in the brain rather than ongoing tissue damage. This therapy aims to teach the brain to reinterpret pain signals as safe rather than dangerous, effectively breaking the cycle of chronic pain.
The Neurobiological Foundation of Chronic Pain
To understand how PRT works, we must first examine what happens in the nervous system when acute pain transitions to chronic pain. Pain begins as nociception—the detection of potentially harmful stimuli by specialized nerve endings called nociceptors. These signals travel through the spinal cord to the brain, where they undergo complex processing across multiple regions including the thalamus, somatosensory cortex, anterior cingulate cortex, insular cortex, and prefrontal cortex.
The Amygdala’s Central Role in Pain Chronification
The amygdala, often called the brain’s “alarm system,” plays a pivotal role in the development and maintenance of chronic pain that deserves special attention. This almond-shaped structure deep in the temporal lobe is primarily known for processing fear and threat, but its involvement in pain goes far beyond simple fear responses.
In acute pain, the amygdala appropriately activates to signal potential danger, triggering protective responses like withdrawal, increased vigilance, and stress hormone release. However, in chronic pain states, the amygdala becomes hyperactive and hypersensitive. Neuroimaging studies consistently show increased amygdala volume and activity in chronic pain patients, with the degree of enlargement often correlating with pain intensity and duration.
The amygdala doesn’t just respond to pain—it actively modulates it through extensive connections with other brain regions. It sends projections to the periaqueductal gray, a key component of descending pain modulation, where it can either amplify or suppress pain signals. In chronic pain, the amygdala’s outputs tend to facilitate rather than inhibit pain transmission. It also connects bidirectionally with the prefrontal cortex, and in chronic pain states, this connection often weakens, reducing top-down emotional regulation.
Perhaps most importantly, the amygdala is responsible for fear conditioning related to pain. When pain becomes associated with certain movements, positions, or activities, the amygdala encodes these associations as threat memories. These implicit memories can trigger pain responses even in the absence of actual tissue damage. The amygdala’s role in implicit memory means these associations often operate below conscious awareness, making them particularly resistant to cognitive interventions alone.
The amygdala also shows altered neurotransmitter function in chronic pain. GABA, the primary inhibitory neurotransmitter that normally keeps the amygdala’s responses in check, is often reduced. Meanwhile, glutamate and substance P, which promote excitation and pain transmission, are elevated. This neurochemical imbalance maintains the amygdala in a state of perpetual activation, constantly scanning for and amplifying potential threats.
In acute pain, this system functions adaptively. You touch a hot stove, nociceptors fire, your brain processes the danger, and you quickly withdraw your hand. The pain subsides as the tissue heals. However, in chronic pain, this elegant warning system becomes dysregulated through a process called central sensitization.
Central sensitization involves several key changes in the nervous system. First, neurons in the spinal cord and brain become hyperexcitable, firing more readily and intensely in response to stimuli. This amplification means that normal sensations—like light touch or movement—can be interpreted as painful. Second, the brain’s pain processing networks undergo structural and functional changes. Neuroimaging studies have shown altered connectivity between regions involved in sensory processing, emotional regulation, and cognitive evaluation of pain.
The brain areas most affected include the default mode network, which is involved in self-referential thinking and rumination; the salience network, which determines what stimuli deserve attention; and the descending pain modulatory system, which normally helps dampen pain signals. In chronic pain, the default mode network often shows increased activity during rest, contributing to persistent awareness of pain. The salience network becomes hypervigilant to bodily sensations, while the descending modulatory system becomes less effective at inhibiting pain signals.
Perhaps most importantly, chronic pain involves powerful learning mechanisms. Through classical conditioning, neutral stimuli like certain movements, activities, or even thoughts become associated with pain. The brain learns to predict pain and begins generating it preemptively—a phenomenon called predictive coding. This means the brain can create genuine pain sensations based on expectations rather than actual tissue damage.
The fear-avoidance cycle plays a crucial role in maintaining chronic pain. When someone experiences pain, they naturally develop fear around activities they believe might worsen it. This leads to avoidance behaviors, which prevent the person from learning that these activities are actually safe. The avoidance itself becomes reinforcing, strengthening the brain’s belief that danger exists. Meanwhile, physical deconditioning from reduced activity can make movement genuinely more uncomfortable, seeming to confirm the threat.
How Pain Reprocessing Therapy Interrupts Chronic Pain Cycles
PRT directly targets these neurobiological mechanisms through a systematic approach to retraining the brain’s interpretation of pain signals. The therapy is built on several core principles that work together to interrupt the chronic pain cycle at multiple levels.
Calming the Amygdala Through Safety Learning
The fundamental mechanism of PRT involves shifting pain from a threat-based interpretation to a safety-based interpretation, with particular focus on retraining the amygdala’s response patterns. When the brain categorizes pain signals as dangerous, the amygdala activates stress response systems, increases vigilance, and amplifies the pain experience. PRT teaches patients to reappraise these signals as safe—as false alarms from an overprotective nervous system rather than indicators of tissue damage.
This reappraisal process specifically targets the amygdala through what neuroscientists call “extinction learning” or more accurately, “inhibitory learning.” Rather than erasing fear memories stored in the amygdala, PRT helps create new safety memories that compete with and override fear associations. Research shows that successful safety learning involves strengthening connections between the ventromedial prefrontal cortex and the amygdala, allowing cognitive areas to regulate emotional alarm responses.
The process of calming the amygdala requires repeated experiences of safety in the presence of previously feared stimuli. Each time a patient experiences a sensation without catastrophic consequences, it creates a prediction error that the amygdala must process. Over time, these prediction errors accumulate, gradually updating the amygdala’s threat detection algorithms. Brain imaging studies of successful PRT treatment show decreased amygdala activation during pain processing, often returning to levels similar to pain-free controls.
PRT also leverages the power of prediction error—the mismatch between expected and actual outcomes—to update learned pain associations. When patients engage in previously avoided activities with a sense of safety and experience less pain than anticipated, it creates a prediction error that can weaken conditioned pain responses. Repeated safe exposures help the brain update its predictive models, gradually reducing anticipatory anxiety and pain generation.
The therapy addresses the attentional mechanisms that maintain chronic pain. In chronic pain states, attention becomes selectively biased toward bodily sensations and potential threats. PRT includes techniques to shift attention away from pain scanning and toward engaging with life activities. This isn’t about distraction or ignoring pain, but rather about changing the quality of attention from fearful vigilance to curious, non-judgmental awareness.
Distinguishing Between Trauma Responses and Genuine Intuition
One of the most sophisticated aspects of PRT involves helping patients differentiate between trauma-based alarm signals from the amygdala and genuine intuitive warnings about actual danger. This distinction is crucial because both can manifest as bodily sensations, emotional responses, and strong urges to avoid certain situations. However, their origins, qualities, and appropriate responses differ significantly.
Understanding Trauma-Based Signals
Trauma responses originating from an overactive amygdala have distinct characteristics. They tend to be intense and immediate, often disproportionate to the actual situation. These responses are typically accompanied by familiar patterns of physical tension, rapid heartbeat, shallow breathing, or a sense of panic. The amygdala, operating on implicit memories, triggers these responses based on pattern matching—when current situations share any similarity with past threatening experiences, even if the resemblance is superficial.
Trauma-based signals often have a desperate, urgent quality—a sense that something terrible will happen if you don’t immediately escape or avoid. They’re frequently accompanied by catastrophic thinking and worst-case scenario predictions. The body feels activated in a way that’s disconnected from present-moment reality. These responses tend to be rigid and repetitive, showing up in predictable patterns regardless of actual circumstances.
Importantly, trauma responses stored in the amygdala don’t update easily with new information. You might cognitively know you’re safe, but your body continues reacting as if under threat. This disconnect between cognitive understanding and embodied experience is a hallmark of trauma-based amygdala activation. The sensations often have an “old” quality to them—they feel familiar in a way that connects to past experiences rather than present circumstances.
Recognizing Genuine Intuition
True intuition, in contrast, has a different quality and neurobiological basis. While the amygdala plays a role in intuitive responses, genuine intuition involves integration across multiple brain networks, including the insula, anterior cingulate cortex, and areas involved in implicit pattern recognition. Intuition draws on vast stores of implicit knowledge and subtle environmental cues processed below conscious awareness.
Genuine intuitive warnings tend to be calmer and clearer than trauma responses. There’s often a sense of knowing without panic—a clear message without the overwhelming physiological activation. True intuition might manifest as a quiet sense of unease, a subtle pulling back, or a clear “no” that doesn’t come with elaborate catastrophic narratives. The body might feel alert but not dysregulated.
Intuition is also more flexible and context-specific. It responds to actual present-moment cues rather than operating from rigid patterns. When you pause to investigate intuitive feelings, they often reveal specific, current information—perhaps subtle behavioral cues from another person, environmental factors you hadn’t consciously noticed, or patterns your brain has detected without explicit awareness.
Unlike trauma responses, genuine intuition often becomes clearer when you slow down and tune in, rather than more chaotic. It doesn’t require immediate action but allows for thoughtful response. There’s usually coherence between the intuitive sense and observable reality—even if you can’t immediately articulate why, investigation often reveals legitimate reasons for the intuitive warning.
Developing Discernment Through PRT
Pain Reprocessing Therapy helps patients develop discernment between these two types of signals through several specific practices. Somatic tracking, when applied to emotional and intuitive experiences, helps patients notice the different qualities of trauma responses versus genuine intuition. Patients learn to ask themselves key questions: Is this familiar? Does it feel old or current? Is my response proportionate to the actual situation? Am I responding to what’s here now or to a memory?
The therapy teaches patients to test their responses through graduated behavioral experiments. If avoiding a certain movement is trauma-based rather than intuitively protective, gentle, mindful engagement with that movement in a safe context will gradually reduce the alarm response. True intuitive warnings about genuine danger, however, remain consistent and are often validated by external evidence.
Patients learn to notice the narratives accompanying their bodily responses. Trauma-based amygdala activation often comes with familiar stories—”I’m broken,” “This will never get better,” “Movement is dangerous.” These narratives tend to be absolute, catastrophic, and historically rooted. Genuine intuition might offer simpler, present-focused information—”This particular movement needs modification,” “This situation requires caution,” without the overlay of historical trauma.
PRT also helps patients recognize how their amygdala’s sensitivity settings have been calibrated by past experiences. Trauma, especially developmental trauma, can set the amygdala’s threat detection threshold extremely low, causing it to sound alarms for non-threatening stimuli. Understanding this helps patients approach their alarm signals with curiosity rather than immediate belief, creating space to evaluate whether the warning reflects current reality or historical conditioning.
Core Techniques and Components of PRT
Pain Reprocessing Therapy employs a structured set of techniques delivered typically over 4-8 weeks of treatment. Each component targets specific aspects of the chronic pain cycle while building on previous elements to create lasting change.
Pain Education and Reconceptualization forms the foundation of PRT. Patients learn about the neuroscience of pain, understanding how the brain can generate real pain without tissue damage. This education specifically includes understanding the amygdala’s role in maintaining chronic pain and how trauma responses differ from genuine body wisdom. Patients learn that their amygdala, while trying to protect them, has become overprotective based on past experiences. This cognitive framework provides the basis for all subsequent interventions.
Somatic Tracking represents PRT’s signature technique. Unlike traditional mindfulness approaches that emphasize non-judgmental awareness, somatic tracking specifically aims to attend to pain sensations through a lens of safety. Patients are guided to observe their pain with curiosity rather than fear, noticing its qualities—intensity, location, texture—while simultaneously reinforcing messages of safety. This practice directly communicates with the amygdala through embodied experience rather than just cognitive understanding.
During somatic tracking, patients also learn to differentiate between sensations that represent amygdala-driven alarm versus actual tissue signals. They might notice that anxiety-driven pain has a particular quality—perhaps electric, diffuse, or moving—while mechanical sensations from actual tissue stress feel different—more localized, consistent with movement patterns, and proportionate to activity. This differentiation helps build trust in the body’s communication while recognizing when the amygdala is creating false alarms.
Safety Reappraisal involves systematically examining evidence that the body is fundamentally safe and healthy. This process specifically targets the amygdala’s threat detection system by providing repeated disconfirming experiences. Patients review medical tests showing no structural damage, recall activities they can do without lasting harm, and identify patterns suggesting their pain is brain-generated rather than tissue-based. Each piece of safety evidence helps update the amygdala’s threat assessment algorithms.
Addressing Emotional Threats recognizes that chronic pain often develops in contexts of psychological stress or trauma. PRT helps patients identify and process emotions that may be maintaining amygdala hypervigilance. This includes distinguishing between current emotional needs and historical trauma responses. Patients learn to recognize when their pain intensifies due to emotional activation rather than physical factors, understanding how the amygdala converts emotional threats into physical pain signals.
Trauma-Informed Movement represents a crucial addition to standard PRT protocols. Recognizing that many chronic pain patients have trauma histories that affect their relationship with their bodies, this component helps patients distinguish between trauma-based movement fears and genuine bodily limitations. Patients learn to approach movement with compassion for their amygdala’s protective responses while gradually demonstrating safety through positive movement experiences.
Gradual Exposure with Amygdala Retraining helps patients return to avoided activities while specifically focusing on calming amygdala responses. Unlike traditional exposure that may inadvertently reinforce threat perception through white-knuckling through fear, PRT’s approach emphasizes creating positive prediction errors for the amygdala. Patients engage in previously feared activities with playfulness, social connection, and positive affect—conditions that naturally downregulate amygdala activation.
Positive Affect Induction actively cultivates emotional states that directly counter amygdala hyperactivation. Laughter, play, and social connection activate neural circuits that inhibit amygdala fear responses. This isn’t about forcing positivity but rather strategically engaging systems that naturally regulate the amygdala. Patients learn to recognize how positive emotional states immediately influence their pain, providing experiential evidence that pain is neuroplastically maintained.
Intuition Restoration helps patients rebuild trust in their body’s wisdom while recognizing trauma-based false alarms. Through careful attention and behavioral experiments, patients learn to honor genuine intuitive warnings while not being controlled by trauma responses. This might involve noticing that their intuition accurately guides them in non-pain-related areas of life, helping them recognize that their inner knowing remains intact despite the amygdala’s overactivity around pain.
The Therapeutic Process: What Patients Experience
The journey through Pain Reprocessing Therapy typically unfolds in distinct phases, each bringing its own challenges and revelations. Understanding this process helps patients navigate the ups and downs of recovery while maintaining hope and engagement.
Initially, many patients experience skepticism. After years of being told their pain is real and searching for physical solutions, the idea that pain could be brain-generated seems impossible or even insulting. Skilled PRT therapists validate these concerns while gently introducing evidence that challenges purely structural explanations. They might point out inconsistencies—why does pain worsen with stress but not always with physical activity? Why do some people with severe disc herniations have no pain while others with normal imaging suffer tremendously?
The Amygdala Recalibration Phase
As patients begin understanding the amygdala’s role in their pain, many experience a mixture of relief and apprehension. Relief comes from finally having an explanation that accounts for their pain’s puzzling patterns—why it moves, fluctuates with emotions, or appears in multiple body areas. Apprehension arises from recognizing that healing requires facing fears their amygdala has been protecting them from.
During early somatic tracking sessions, patients often notice their amygdala’s immediate activation when attention turns to pain. Heart rate increases, breathing becomes shallow, and catastrophic thoughts arise automatically. Therapists help patients recognize these as amygdala responses rather than indicators of tissue damage. With practice, patients learn to observe these alarm signals with compassion, understanding their amygdala is trying to protect them based on outdated information.
A crucial phase involves learning to distinguish trauma responses from intuition. One patient might realize their back pain intensifies whenever they consider setting boundaries—their amygdala having learned in childhood that assertiveness led to punishment. They learn to recognize this as a trauma response rather than intuitive guidance to remain passive. Another might discover their pain genuinely worsens with specific movements that need modification, representing accurate bodily feedback rather than false alarms.
Processing Trauma and Emotions
The emotional processing component often reveals connections between trauma history and pain patterns. Many patients discover their amygdala became hypervigilant following specific traumatic events—perhaps a difficult surgery, accident, or period of intense stress. Some find deeper connections to developmental trauma, where the amygdala learned early that the body wasn’t safe.
Processing these connections doesn’t mean reliving trauma in detail. Instead, PRT helps patients understand how past experiences calibrated their amygdala’s sensitivity. They learn to offer compassion to the part of their brain that’s been working overtime to protect them. This compassionate understanding, combined with present-moment safety experiences, helps the amygdala gradually recalibrate.
Patients often report breakthrough moments when they successfully differentiate between trauma and intuition. One patient described suddenly recognizing that her urge to avoid exercise came with familiar childhood feelings of shame and inadequacy—trauma responses rather than intuitive body wisdom. When she approached movement with curiosity instead of fear, she discovered her body actually craved gentle activity.
Integration and Embodied Trust
As treatment progresses, patients develop increasing sophistication in reading their body’s signals. They learn to recognize the “signature” of amygdala-driven pain—perhaps a particular quality of urgency, familiar accompanying thoughts, or predictable triggers. They also become more attuned to genuine bodily communication—the difference between inflammatory pain that needs rest and neuroplastic pain that benefits from movement.
This discernment extends beyond pain to overall embodied wisdom. Patients report improved ability to recognize genuine hunger versus emotional eating, authentic fatigue versus depression-related lethargy, and real interpersonal threats versus trauma-based social anxiety. The amygdala retraining generalizes to improve overall emotional regulation and body trust.
Outcomes and Benefits: What the Research Shows
The empirical support for Pain Reprocessing Therapy has grown substantially, with several high-quality studies demonstrating its effectiveness. The landmark randomized controlled trial published in JAMA Psychiatry in 2021 provided compelling evidence for PRT’s efficacy in treating chronic back pain.
In this study, 151 participants with chronic back pain were randomized to receive either PRT, placebo injection, or usual care. After four weeks of treatment, 66% of PRT participants were pain-free or nearly pain-free, compared to just 20% in the placebo group and 10% in the usual care group. Perhaps more remarkably, these gains were largely maintained at one-year follow-up, with 60% of PRT participants still reporting minimal or no pain.
Neurobiological Changes: The Amygdala Evidence
Brain imaging data from PRT studies reveals specific changes in amygdala function that correlate with clinical improvement. Successful treatment is associated with decreased amygdala volume, returning toward levels seen in pain-free individuals. Functional MRI shows reduced amygdala activation in response to pain-related stimuli, indicating decreased threat perception.
Connectivity analyses reveal strengthened connections between the prefrontal cortex and amygdala following PRT, suggesting improved top-down regulation of fear responses. The amygdala also shows normalized neurotransmitter function, with increases in GABA and decreases in excitatory neurotransmitters. These neurochemical changes provide a biological foundation for sustained improvement.
Studies examining fear conditioning—a primary amygdala function—show that PRT participants develop improved extinction learning. They more readily form new safety associations and show less return of fear, indicating fundamental changes in how the amygdala processes and stores threat-related memories.
Beyond pain reduction, patients report numerous additional benefits from PRT. Many experience significant improvements in mood and anxiety, likely due to both pain relief and improved amygdala regulation. Sleep often improves as nighttime hypervigilance decreases. Patients frequently report enhanced body trust—no longer fearing that normal sensations signal danger.
The functional improvements can be dramatic. Patients return to work, resume exercise, travel, and engage in activities they’d abandoned for years. These functional gains often exceed what would be expected from pain reduction alone, suggesting PRT helps resolve the broader fear-avoidance patterns maintained by amygdala hyperactivation.
Trauma Resolution and Intuitive Restoration
A particularly meaningful outcome for many patients is the restoration of trust in their intuition. After learning to differentiate trauma responses from genuine intuitive wisdom, patients report improved decision-making in all life areas. They describe feeling more connected to their authentic selves, able to honor genuine bodily wisdom while not being controlled by trauma-based fears.
Some patients experience resolution of trauma symptoms beyond pain. The amygdala retraining and emotional processing in PRT can lead to improvements in PTSD symptoms, including decreased hypervigilance, fewer intrusive memories, and reduced emotional numbing. While PRT isn’t primarily a trauma therapy, its focus on safety learning and amygdala regulation can have broader therapeutic benefits.
Quality of life measures consistently show improvement following PRT. Patients report greater life satisfaction, improved relationships, and renewed sense of purpose. Many describe feeling freed not just from pain but from the prison of chronic fear and body mistrust. The constant amygdala-driven vigilance gradually gives way to embodied presence and trust.
Integration with Other Approaches
While PRT can be effective as a standalone treatment, it often works best as part of a comprehensive approach to chronic pain recovery. Understanding how PRT integrates with other modalities helps patients and clinicians design optimal treatment plans.
Trauma-Informed Therapies
For patients with significant trauma histories, combining PRT with trauma-focused therapies can be particularly powerful. EMDR (Eye Movement Desensitization and Reprocessing) can help process specific traumatic memories that maintain amygdala hyperactivation. Somatic Experiencing helps regulate nervous system dysregulation that often accompanies both trauma and chronic pain. Internal Family Systems therapy can address the protective parts that maintain pain as a defense against overwhelming emotions.
The key is sequencing and integration. Some patients benefit from trauma therapy before PRT to stabilize their nervous system enough to engage with pain reprocessing. Others find that PRT’s focus on safety and empowerment provides a foundation for deeper trauma work. Clinicians skilled in both approaches can weave them together, using PRT techniques for pain while addressing underlying trauma that maintains amygdala sensitization.
Physical therapy and movement practices complement PRT beautifully when approached through a neuroplastic lens. Rather than focusing on structural corrections or strengthening weak muscles, movement becomes an opportunity to reinforce safety and restore confidence. Yoga, tai chi, and dance can be particularly helpful, combining movement with mindfulness and positive affect. The key is ensuring movement practices don’t inadvertently reinforce threat perception through excessive focus on “proper” form or fear-based precautions.
Psychological therapies like cognitive-behavioral therapy (CBT) and acceptance and commitment therapy (ACT) share some overlaps with PRT but differ in emphasis. While CBT for pain often focuses on coping strategies and challenging catastrophic thoughts, PRT specifically targets the brain’s danger detection system. ACT’s emphasis on psychological flexibility and values-based action can support PRT’s exposure and engagement components. Many patients benefit from combining approaches, using PRT for pain reprocessing while drawing on other modalities for broader psychological support.
Medication management may still play a role during PRT treatment, though the goal is typically to reduce or eliminate pharmaceutical dependence. Some patients find that low-dose antidepressants or anti-anxiety medications help calm the nervous system enough to engage with PRT techniques. However, opioids and other strong pain medications can interfere with the relearning process by preventing the brain from updating its pain predictions. Careful tapering with medical supervision may be necessary.
Mindfulness and meditation practices align well with PRT’s somatic tracking component. However, traditional mindfulness’s emphasis on non-judgmental awareness differs from PRT’s active safety reappraisal. Some patients find that combining both approaches—using traditional mindfulness for general awareness and PRT-style somatic tracking specifically for pain—provides the best results.
Challenges and Limitations
Despite its promise, Pain Reprocessing Therapy isn’t without challenges and limitations. Understanding these helps set realistic expectations and identify patients most likely to benefit.
When Trauma Complicates Treatment
For patients with complex trauma histories, distinguishing between trauma responses and intuition can be particularly challenging. Years or decades of amygdala hyperactivation can make it difficult to recognize what normal, non-threatened bodily sensations feel like. These patients may need extended treatment and additional trauma-focused support to successfully recalibrate their threat detection systems.
Some patients become overwhelmed when beginning to differentiate trauma from intuition, realizing how much of their life has been governed by trauma responses rather than authentic choice. This recognition, while ultimately liberating, can initially increase distress. Skilled therapists must balance validation of this difficulty with encouragement about the possibility of change.
The process of amygdala retraining can sometimes trigger trauma memories or emotional flooding. While PRT doesn’t require detailed trauma processing, the focus on safety and body awareness can bring suppressed material to consciousness. Therapists need trauma-informed training to handle these situations appropriately, knowing when to continue with PRT techniques versus when to shift to stabilization or refer for specialized trauma treatment.
Not all chronic pain is neuroplastic. Conditions involving ongoing inflammation, active disease processes, or structural damage requiring medical intervention need appropriate medical care. PRT is most applicable to primary neuroplastic pain—pain without clear peripheral pathology—or secondary neuroplastic pain where central sensitization amplifies pain beyond what tissue damage would predict. Careful assessment is crucial to determine appropriateness for PRT.
Patient readiness and belief represent significant factors in treatment success. Those strongly attached to structural explanations for their pain may struggle with PRT’s paradigm shift. Years of medical messaging about “slipped discs” or “bone on bone” arthritis create powerful beliefs that can be difficult to overcome. Some patients feel invalidated by suggestions their pain is brain-generated, interpreting this as meaning it’s not real or they’re somehow at fault.
The emotional processing component can be challenging for patients with significant trauma or limited emotional awareness. While PRT isn’t psychotherapy, it does require engaging with emotions that may have been long suppressed. Some patients need concurrent psychological support to safely process what emerges during treatment.
Access and availability remain practical limitations. Trained PRT practitioners are still relatively few, concentrated mainly in urban areas. While self-help resources and online programs are emerging, the therapeutic relationship and personalized guidance appear important for optimal outcomes. Insurance coverage varies, with many patients paying out of pocket for treatment.
Individual variation in response is considerable. While studies show impressive group-level outcomes, not everyone responds equally to PRT. Factors influencing response include pain duration, comorbid conditions, psychological flexibility, and social support. Some patients experience rapid, complete resolution while others see gradual, partial improvement. A small percentage show minimal response despite full engagement with treatment.
The Future of Pain Reprocessing Therapy
As PRT gains recognition and empirical support, several exciting developments are emerging. Research continues to refine our understanding of who responds best to treatment and how to optimize protocols for different populations and pain conditions.
Advancing Amygdala-Focused Interventions
Future research is likely to develop more sophisticated methods for directly targeting amygdala function in chronic pain. Real-time fMRI neurofeedback studies are exploring whether patients can learn to consciously regulate amygdala activity, potentially accelerating the retraining process. Transcranial magnetic stimulation protocols targeting amygdala-prefrontal circuits show promise for enhancing safety learning.
Researchers are also investigating biomarkers that might predict which patients have primarily amygdala-driven pain versus other mechanisms. Genetic variations in amygdala neurotransmitter systems, early life stress exposure, and specific connectivity patterns may help personalize treatment selection. This precision medicine approach could match patients to interventions most likely to address their specific neurobiological patterns.
The development of better tools for differentiating trauma responses from intuition represents another frontier. Researchers are exploring whether heart rate variability, skin conductance patterns, or other physiological markers can help patients and clinicians distinguish between these different types of bodily signals. Apps and wearables might eventually provide real-time feedback about whether a sensation represents amygdala activation versus other processes.
Neuroimaging studies are identifying biomarkers that might predict treatment response. Patterns of brain connectivity, particularly in the default mode and salience networks, may indicate likelihood of success with PRT. This could allow more personalized treatment selection, matching patients to interventions most likely to help them.
Technology-assisted delivery is expanding access to PRT principles. Virtual reality applications allow immersive somatic tracking experiences, while smartphone apps provide guided exercises and progress tracking. AI-powered chatbots are being developed to provide basic PRT education and support, though these cannot replace skilled therapeutic relationships for complex cases.
Integration with healthcare systems represents both opportunity and challenge. As evidence accumulates, some progressive healthcare organizations are beginning to incorporate PRT into pain management programs. However, this requires significant paradigm shifts in medical education and practice. Training healthcare providers to understand and convey neuroplastic pain concepts without inadvertently invalidating patient experiences requires careful attention.
Research is expanding to investigate PRT’s application to other chronic symptoms beyond pain. Conditions like chronic fatigue, irritable bowel syndrome, and functional neurological disorders share similar neurobiological mechanisms of central sensitization and threat perception. Preliminary studies suggest PRT principles may benefit these conditions, though specific protocols need development.
The societal implications of widespread PRT adoption could be profound. Chronic pain costs hundreds of billions annually in medical expenses and lost productivity. If even a fraction of chronic pain patients could recover through PRT, the economic and human benefits would be enormous. Moreover, shifting from a purely biomedical model to one recognizing the brain’s role in chronic symptoms could transform how we approach many chronic conditions.
Conclusion: A Paradigm Shift in Understanding and Treating Chronic Pain
Pain Reprocessing Therapy represents more than just another treatment option for chronic pain—it embodies a fundamental shift in how we understand the relationship between mind, brain, and body. By recognizing chronic pain as often resulting from learned neural pathways and amygdala hyperactivation rather than ongoing tissue damage, PRT opens possibilities for recovery that seemed impossible under purely structural models.
The therapy’s power lies not in denying the reality of pain or placing blame on sufferers, but in revealing the brain’s remarkable capacity for change. Through systematic retraining of danger detection systems—particularly the amygdala—emotional processing, and gradual re-engagement with life, patients can break free from cycles of pain that may have persisted for years or decades. The sophisticated understanding of how trauma responses differ from genuine intuition adds another layer of healing, helping patients reclaim not just physical comfort but embodied wisdom and authentic self-trust.
As research continues to validate and refine PRT approaches, particularly around amygdala retraining and trauma-informed modifications, hope grows for the millions suffering from chronic pain worldwide. While not a panacea for all pain conditions, PRT offers a scientifically grounded, empowering approach that returns agency to patients and recognizes the profound intelligence of the nervous system—both in generating chronic pain and in healing from it.
The journey through Pain Reprocessing Therapy asks patients to reconceptualize their pain, face their fears, process difficult emotions, distinguish trauma from intuition, and trust their bodies again. For those who undertake this journey, the rewards often extend far beyond pain relief to encompass a transformed relationship with their bodies, emotions, and lives. In teaching the brain—and especially the amygdala—that it is safe, PRT doesn’t just treat chronic pain—it facilitates a return to wholeness, authentic embodiment, and vitality that many thought permanently lost.




















0 Comments