The Paradox of Healing

In the vast landscape of psychotherapeutic literature, few works capture the intricate dance between healer and patient as poignantly as Harry Stack Sullivan’s play “The Physician.” This lesser-known dramatic work, highlighted by Irvin Yalom in his explorations of therapeutic dynamics, offers a window into one of therapy’s most profound truths: that those who heal are often themselves in need of healing, and that the therapeutic relationship transforms both participants in ways neither can fully anticipate.
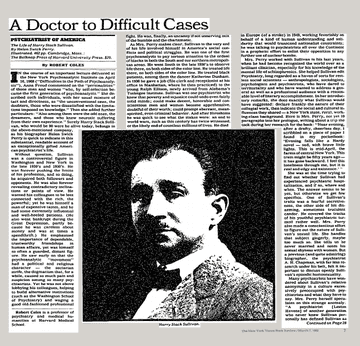
Sullivan, a pioneering psychiatrist whose influence on interpersonal psychotherapy cannot be overstated, chose an unusual medium—drama—to explore what happens when the traditional boundaries between therapist and patient dissolve. His play presents us with a psychiatrist who enrolls as a patient under false pretenses, intending to treat his own provider. This ingenious premise serves as a metaphor for the complex reality that unfolds in every therapeutic encounter: the mutual vulnerability, the shared humanity, and the bidirectional flow of healing that characterizes genuine therapeutic work.
Sullivan’s Vision: The Physician as Patient
Harry Stack Sullivan’s decision to write “The Physician” rather than another clinical paper speaks to his understanding that some truths about human connection and healing cannot be adequately conveyed through academic prose alone. The play’s central conceit—a psychiatrist becoming a patient to treat his therapist—illuminates the artificial nature of the rigid hierarchies we often impose in therapeutic relationships.
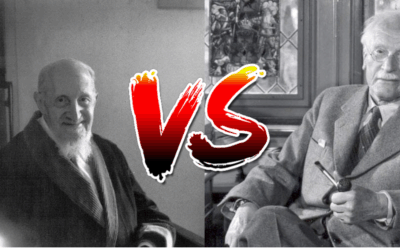
In Yalom’s discussion of this work, he notes Sullivan’s relative obscurity compared to his contemporaries, attributing this partly to Sullivan’s limited published output. Yet “The Physician” stands as a testament to Sullivan’s profound understanding of what he termed the “participant-observer” role of the therapist. The therapist is never merely an objective observer but is always participating in a shared interpersonal field with the patient.
The play dramatizes what Sullivan knew from his clinical work: that the therapist’s own wounds, anxieties, and unresolved conflicts inevitably enter the therapeutic space. Rather than viewing this as a contamination of the therapeutic process, Sullivan saw it as the very essence of healing—two human beings meeting in authentic connection, each bringing their full humanity to the encounter.
The Laboratory of Discovery: How New Therapies Emerge from Clinical Encounters
Perhaps one of the most remarkable aspects of psychotherapy is that our patients are not just recipients of established treatments—they are co-creators of entirely new therapeutic approaches. The history of psychotherapy is rich with examples of groundbreaking modalities that emerged not from abstract theorizing but from the living laboratory of the therapeutic encounter.
Consider David Grand’s discovery of Brainspotting in 2003. While conducting an EMDR session with an Olympic ice skater, Grand noticed that when her eyes remained fixed on a particular spot, she accessed deeper traumatic material than ever before. Rather than dismissing this as an anomaly or forcing the session back to standard protocol, Grand followed his patient’s process. This single moment of clinical curiosity and attunement to his patient’s unique response birthed an entirely new therapeutic modality that has since helped thousands process trauma.
Fritz Perls developed Gestalt therapy through his direct work with patients, discovering that when he encouraged them to speak to empty chairs as if addressing significant people in their lives, profound emotional breakthroughs occurred. The famous “empty chair technique” wasn’t born in a research lab but emerged from Perls’ willingness to experiment and follow his patients’ spontaneous expressions of internal conflict.
Richard Schwartz’s Internal Family Systems (IFS) therapy arose from his puzzling observation that his patients seemed to have distinct “parts” with their own perspectives and feelings. Rather than pathologizing this or trying to eliminate these parts, Schwartz began engaging with them directly. His patients taught him that these parts had protective functions and that healing came not from eliminating them but from helping them work together harmoniously. The entire IFS model—now one of the most innovative approaches to trauma treatment—emerged from Schwartz’s willingness to learn from his patients’ internal experiences.
Francine Shapiro discovered EMDR (Eye Movement Desensitization and Reprocessing) through a personal experience while walking in a park, noticing that disturbing thoughts seemed to lose their charge when her eyes moved rapidly back and forth. She then refined this observation through work with her patients, who taught her how bilateral stimulation could facilitate the processing of traumatic memories.
Eugene Gendlin’s Focusing technique emerged from his research question about why some patients improved in therapy while others didn’t. Through careful observation of therapeutic sessions, he discovered that successful patients had a particular way of attending to their bodily felt sense of problems. This observation, refined through countless clinical encounters, became a standalone therapeutic approach.
These discoveries remind us that every therapeutic session is potentially a moment of innovation. When we remain open, curious, and willing to follow our patients’ lead rather than rigidly adhering to protocols, we participate in the ongoing evolution of psychotherapy itself.
The Wounded Healer Archetype
The concept of the wounded healer predates modern psychotherapy by millennia, finding expression in shamanic traditions, Greek mythology (particularly in the figure of Chiron, the wounded centaur who became a great healer), and various spiritual traditions. Carl Jung brought this archetype into psychological discourse, recognizing that the therapist’s own wounds could become a source of healing power when properly understood and integrated.
In contemporary psychotherapy, we understand that our wounds do not disqualify us from helping others; rather, they can become the very source of our capacity for empathy, understanding, and genuine connection. The therapist who has struggled with depression may have a particular sensitivity to the subtle shadings of despair in their patients. The clinician who has wrestled with anxiety understands viscerally the prison that fear can create. The practitioner who has navigated loss knows the territory of grief in ways that textbooks alone could never teach.
This is not to suggest that therapists should use their patients’ sessions to work through their own unresolved issues—that would be a violation of the therapeutic frame and a failure of professional responsibility. Rather, it means that our own experiences of suffering, when properly processed and integrated through our own therapy, supervision, and personal work, become a wellspring of compassion and understanding that enriches our clinical work.
Learning from Our Patients: The Reciprocal Nature of Healing
One of the most humbling and beautiful aspects of therapeutic work is the recognition that we often learn more from our patients than they do from us. Each patient who enters our office brings a unique constellation of experiences, perspectives, and wisdom that expands our understanding of what it means to be human.
Yalom has written extensively about how his patients have been his greatest teachers, showing him aspects of courage, resilience, and creativity that no theoretical framework could have predicted. In “The Physician,” Sullivan dramatizes this reversal of roles, suggesting that the traditional power dynamics of therapy may obscure the mutual exchange of wisdom that occurs in genuine therapeutic encounters.
Consider the patient who, despite experiencing profound trauma, maintains a capacity for joy and connection that challenges our assumptions about resilience. Or the individual struggling with severe mental illness who demonstrates a clarity of perception about certain aspects of human nature that stops us in our tracks. These moments of recognition—when we realize that our patient has just taught us something essential about life, suffering, or healing—are among the most precious gifts of clinical work.
This reciprocal learning extends beyond individual insights to fundamental questions about the nature of healing itself. Our patients teach us about the limits of our theories, the inadequacy of our diagnostic categories, and the mystery of human transformation. They remind us that healing rarely follows the linear path described in our treatment manuals, that resistance often contains wisdom, and that symptoms frequently serve protective functions we must respect even as we work toward change.
The Creative Edge: Patients as Co-Innovators
Every patient who walks through our door presents a unique puzzle that existing therapeutic approaches may not fully address. This gap between theory and lived experience becomes the fertile ground for therapeutic innovation. When we listen deeply to our patients’ experiences and remain flexible in our approach, we often discover new pathways to healing.
Consider how Bessel van der Kolk’s groundbreaking work on trauma emerged from his observation that his patients’ bodies held trauma in ways that talk therapy couldn’t access. His patients taught him that trauma lives in the body, leading to his integration of body-based approaches into trauma treatment. The entire field of somatic psychology owes much to therapists who listened when their patients said, “I can’t think my way out of this—I feel it in my body.”
Peter Levine’s Somatic Experiencing arose from his observation of how animals in the wild discharge trauma naturally. But it was his patients who taught him how to adapt these observations to human healing, showing him the importance of titration, pendulation, and resource-building in trauma resolution.
Pat Ogden’s Sensorimotor Psychotherapy emerged from decades of clinical observation, noticing how patients’ postures, gestures, and movements revealed unspoken stories and provided doorways to healing that purely cognitive approaches missed.
Even established modalities continue to evolve through clinical encounter. Cognitive Behavioral Therapy has spawned numerous “third wave” therapies—Acceptance and Commitment Therapy, Dialectical Behavior Therapy, Mindfulness-Based Cognitive Therapy—each emerging from clinicians’ recognition that their patients needed something more than traditional CBT could offer.
The lesson here is profound: our patients are not passive recipients of our expertise but active collaborators in the discovery of what heals. When we approach each session with genuine curiosity about what might emerge, we participate in the ongoing creation of psychotherapy itself.
The Transformative Process: Becoming Through Relationship
The interpersonal school of psychotherapy, of which Sullivan was a founding figure, posits that we become ourselves through our relationships with others. This principle applies with particular force to the therapeutic relationship. Both therapist and patient are changed by their encounter, though in different ways and to different degrees.
For the therapist, each therapeutic relationship offers an opportunity for growth and refinement of clinical skills, but more importantly, for deepening self-awareness and expanding capacity for presence and connection. The challenging patient who triggers our own unresolved issues becomes an invitation to further personal work. The patient whose suffering echoes our own reminds us of the ongoing nature of healing. The patient who trusts us with their most vulnerable truths calls us to be worthy of that trust.
This ongoing process of becoming a better healer is never complete. Just as our patients are works in progress, so too are we as clinicians. Each decade of practice brings new challenges, new learning edges, new recognition of what we don’t know. The therapist at 60 is not simply a more experienced version of the therapist at 30; they are qualitatively different, shaped by thousands of hours of sitting with human suffering and resilience.
The Paradox of Professional Development
Sullivan’s play illuminates a central paradox of professional development in psychotherapy: the more we know, the more we realize how little we know. The beginning therapist may feel overwhelmed by their lack of knowledge and experience, but they may also have a certain freshness of perception, an openness to being surprised, that can be therapeutic in itself. The seasoned therapist brings wisdom and clinical acumen but must guard against the dulling of perception that can come with routine.
“The Physician” suggests that one way to maintain therapeutic vitality is to regularly experience ourselves in the patient role. Whether through our own personal therapy, peer consultation, or simply allowing ourselves to be vulnerable and open to learning from our patients, we must find ways to remember what it feels like to be on the other side of the therapeutic relationship.
This is not merely an intellectual exercise but an embodied practice. We must remember the vulnerability of sharing our deepest fears with another person, the mixture of hope and skepticism that accompanies seeking help, the frustration of being misunderstood, and the profound relief of feeling truly seen and accepted. These experiential memories keep us humble and human in our work.
The Innovation Imperative: Why We Must Remain Students
The field of psychotherapy is remarkably young—barely 130 years old if we date it from Freud’s early work. Compare this to medicine’s millennia of development, and we realize we are still in the early chapters of understanding how psychological healing occurs. This youth should inspire humility and excitement in equal measure.
Our patients often present with complex, interwoven challenges that don’t fit neatly into our diagnostic categories or respond predictably to our evidence-based protocols. A patient with trauma may also struggle with addiction, relationship patterns, and existential questions that require us to weave together multiple approaches or discover entirely new ones.
The therapist who remains rigidly attached to a single modality or theoretical orientation risks missing the unique healing path that each patient requires. Instead, we must cultivate what might be called “beginner’s mind”—approaching each patient as if they were our first, remaining curious about what approach might serve them best, even if it means venturing beyond our training.
This doesn’t mean abandoning clinical rigor or evidence-based practice. Rather, it means holding our knowledge lightly, ready to adapt, modify, or even abandon our preferred approaches when our patients show us a different way forward. The greatest therapeutic innovators have always been those who listened more carefully to their patients than to their theories.
Integration: The Ongoing Journey
The journey of the wounded healer is not a destination but an ongoing process of integration. We are continually called to metabolize our own experiences of suffering and healing in service of our work with others. This requires several key practices:
Personal Therapy: Regular engagement in our own therapeutic process, not just during training but throughout our careers, helps us maintain awareness of our own blind spots and areas of growth.
Supervision and Consultation: The willingness to expose our clinical work to the thoughtful scrutiny of colleagues keeps us honest and helps us recognize when our own issues may be interfering with our clinical judgment.
Mindfulness and Self-Reflection: Developing practices that cultivate present-moment awareness and self-observation helps us track our internal responses to patients and use these responses as clinical data rather than being unconsciously driven by them.
Continuing Education: Remaining open to new ideas, approaches, and perspectives prevents us from becoming rigid in our thinking and practice.
Self-Care: Attending to our own physical, emotional, and spiritual well-being ensures that we have the resources to be fully present for our patients.
Clinical Creativity: Maintaining a spirit of experimentation and play in our work, always with appropriate ethical boundaries, allows new approaches to emerge.
The Sacred Dimension of Therapeutic Work
Sullivan’s choice to explore these themes through drama rather than clinical writing points to something beyond the technical aspects of psychotherapy. There is a sacred dimension to the work we do—sacred not in a religious sense necessarily, but in the sense of touching something essential and mysterious about human existence.
When two people meet in the therapeutic space with genuine openness and commitment to truth, something transformative becomes possible. This transformation cannot be reduced to techniques or interventions; it emerges from the quality of human connection that develops between therapist and patient. “The Physician” dramatizes this sacred dimension, showing how the roles of healer and patient are more fluid and interdependent than our professional structures might suggest.
Implications for Training and Practice
The insights from Sullivan’s play and Yalom’s commentary, combined with the recognition that therapeutic innovation emerges from clinical practice, have important implications for how we train therapists and structure clinical practice. Traditional training models often emphasize the acquisition of knowledge and techniques, with less attention to the personal development of the therapist or the cultivation of clinical creativity.
If we take seriously the idea that the therapist’s own woundedness and ongoing healing process are integral to their effectiveness, and that new therapeutic approaches emerge from the clinical encounter itself, we must reconsider our training priorities.
This might mean:
- Requiring personal therapy as a central component of training, not just as a checkbox to complete but as an ongoing practice
- Creating more opportunities for trainees to explore their own motivations for entering the field and their personal relationships to suffering and healing
- Developing supervision models that attend not just to clinical technique but to the therapist’s personal responses and growth edges
- Teaching trainees to recognize and follow emergent therapeutic moments rather than rigidly adhering to protocols
- Normalizing experimentation and creativity within appropriate ethical boundaries
- Encouraging documentation and sharing of novel interventions that emerge in practice
- Creating forums for clinicians to share their discoveries and innovations with the broader therapeutic community
The Courage to Be Wounded and Creative
Perhaps the most profound message of “The Physician” is that effective therapeutic work requires the courage to acknowledge and embrace our own woundedness while remaining open to discovering new paths to healing. This is not a weakness to be overcome but a strength to be cultivated. The therapist who can sit with their own pain without being overwhelmed by it, who can acknowledge their limitations without being paralyzed by them, who can remain open to learning from every patient—this is the therapist who can create the conditions for genuine healing and innovation.
This courage extends to being willing to venture beyond the familiar, to follow our patients into uncharted therapeutic territory, and to trust that healing wisdom can emerge from the encounter itself. Every session holds the potential for discovery, every patient might teach us something that could benefit countless others.
The Dance of Mutual Transformation and Discovery
Harry Stack Sullivan’s “The Physician,” as illuminated by Irvin Yalom’s commentary, offers us a profound meditation on the nature of therapeutic work. It reminds us that the distinction between healer and patient is more fluid than we might imagine, that our own wounds can become sources of healing power, and that the therapeutic relationship is fundamentally a dance of mutual transformation and discovery.
As we sit with our patients, we are not simply applying techniques or interventions; we are engaging in one of the most ancient and sacred of human activities—the attempt to understand and alleviate suffering through relationship. In this process, we are all wounded healers, all students and teachers, all potential discoverers of new paths to healing.
The history of psychotherapy shows us that our greatest advances have come not from laboratories or lecture halls but from the consulting room, where therapist and patient together navigate the mysteries of human suffering and resilience. Every therapeutic innovator has been, first and foremost, someone who listened deeply to their patients and had the courage to follow where they led.
The play challenges us to embrace the full complexity of our role: to be professional yet personal, boundaried yet open, expert yet eternally learning, traditional yet innovative. It invites us to recognize that our patients are not simply recipients of our wisdom but co-creators of a therapeutic process that has the potential to transform us both and to contribute to the evolution of psychotherapy itself.
In the end, “The Physician” and Yalom’s reflections on it remind us why we entered this field in the first place—not to position ourselves as experts above the fray of human suffering, but to engage fully with the human condition in all its complexity, bringing our own wounded humanity to the service of healing while remaining open to the new discoveries that each therapeutic encounter might yield.
As we continue in our clinical work, may we carry with us the wisdom of Sullivan’s play: that the physician is always also a patient, that healing flows in multiple directions, that our patients are our greatest teachers and co-innovators, and that the therapeutic encounter, when approached with humility, creativity, and openness, has the power to transform not just the individuals involved but the field of psychotherapy itself.
Bibliography
Barker, P. (1998). The Philosophy and Practice of Psychiatric Nursing. Churchill Livingstone.
Conti, R. (2002). “The psychology of the wounded healer.” Psychotherapy in Australia, 8(2), 22-27.
Dunne, C. (2000). Carl Jung: Wounded Healer of the Soul. Parabola Books.
Gendlin, E.T. (1978). Focusing. Bantam Books.
Grand, D. (2013). Brainspotting: The Revolutionary New Therapy for Rapid and Effective Change. Sounds True.
Groesbeck, C.J. (1975). “The archetypal image of the wounded healer.” Journal of Analytical Psychology, 20(2), 122-145.
Jung, C.G. (1951). “Fundamental questions of psychotherapy.” In The Practice of Psychotherapy (Collected Works, Vol. 16). Princeton University Press.
Kirmayer, L.J. (2003). “Asklepian dreams: The ethos of the wounded-healer in the clinical encounter.” Transcultural Psychiatry, 40(2), 248-277.
Levine, P.A. (1997). Waking the Tiger: Healing Trauma. North Atlantic Books.
Miller, A. (1997). The Drama of the Gifted Child: The Search for the True Self. Basic Books.
Nouwen, H.J.M. (1972). The Wounded Healer: Ministry in Contemporary Society. Doubleday.
Ogden, P., Minton, K., & Pain, C. (2006). Trauma and the Body: A Sensorimotor Approach to Psychotherapy. Norton.
Perls, F. (1969). Gestalt Therapy Verbatim. Real People Press.
Remen, R.N. (1996). Kitchen Table Wisdom: Stories That Heal. Riverhead Books.
Schwartz, R.C. (1995). Internal Family Systems Therapy. Guilford Press.
Sedgwick, D. (1994). The Wounded Healer: Countertransference from a Jungian Perspective. Routledge.
Shapiro, F. (2001). Eye Movement Desensitization and Reprocessing (EMDR): Basic Principles, Protocols, and Procedures. Guilford Press.
Sullivan, H.S. (1953). The Interpersonal Theory of Psychiatry. Norton.
Sullivan, H.S. (1954). The Psychiatric Interview. Norton.
van der Kolk, B. (2014). The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma. Viking.
Whan, M. (1987). “Chiron’s wound: Some reflections on the wounded healer.” Harvest, 33, 28-47.
Yalom, I.D. (1989). Love’s Executioner and Other Tales of Psychotherapy. Basic Books.
Yalom, I.D. (2002). The Gift of Therapy: An Open Letter to a New Generation of Therapists and Their Patients. HarperCollins.




















0 Comments