Understanding Trauma Through Schizophrenia and Schizophrenia Through Trauma
The relationship between schizophrenia and trauma has long been a subject of fascination and debate in the fields of psychiatry and psychology. While early theories often focused on developmental and psychodynamic factors, recent research has shed new light on the neurological and genetic underpinnings of the disorder. However, this does not mean that environmental factors, such as trauma, have been ruled out as contributing to the onset and course of schizophrenia. In fact, there is growing evidence to suggest that schizophrenia may exist on a spectrum, with some cases being primarily genetically driven while others are more heavily influenced by traumatic experiences.
Part 1: The Neurological and Genetic Basis of Schizophrenia
“When the defenses of a culture fail, the person is left alone to face the full terror of existence. This is the schizophrenic dilemma: too much reality and not enough illusion.” (Escape from Evil)
– Ernest Becker
In recent years, there has been a significant shift in our understanding of the causes of schizophrenia. While earlier theories often emphasized developmental and psychological factors, such as family dynamics and early childhood experiences, newer research has revealed a strong genetic component to the disorder. Studies have shown that individuals with a family history of schizophrenia are at a much higher risk of developing the condition themselves, suggesting that there may be specific genes or combinations of genes that predispose certain people to psychosis.
However, genetics alone cannot fully explain the development of schizophrenia. While having a genetic vulnerability may increase the likelihood of developing the disorder, it does not necessarily mean that an individual will go on to experience psychotic symptoms. Instead, it appears that a complex interplay of genetic and environmental factors is involved in the onset and course of schizophrenia.
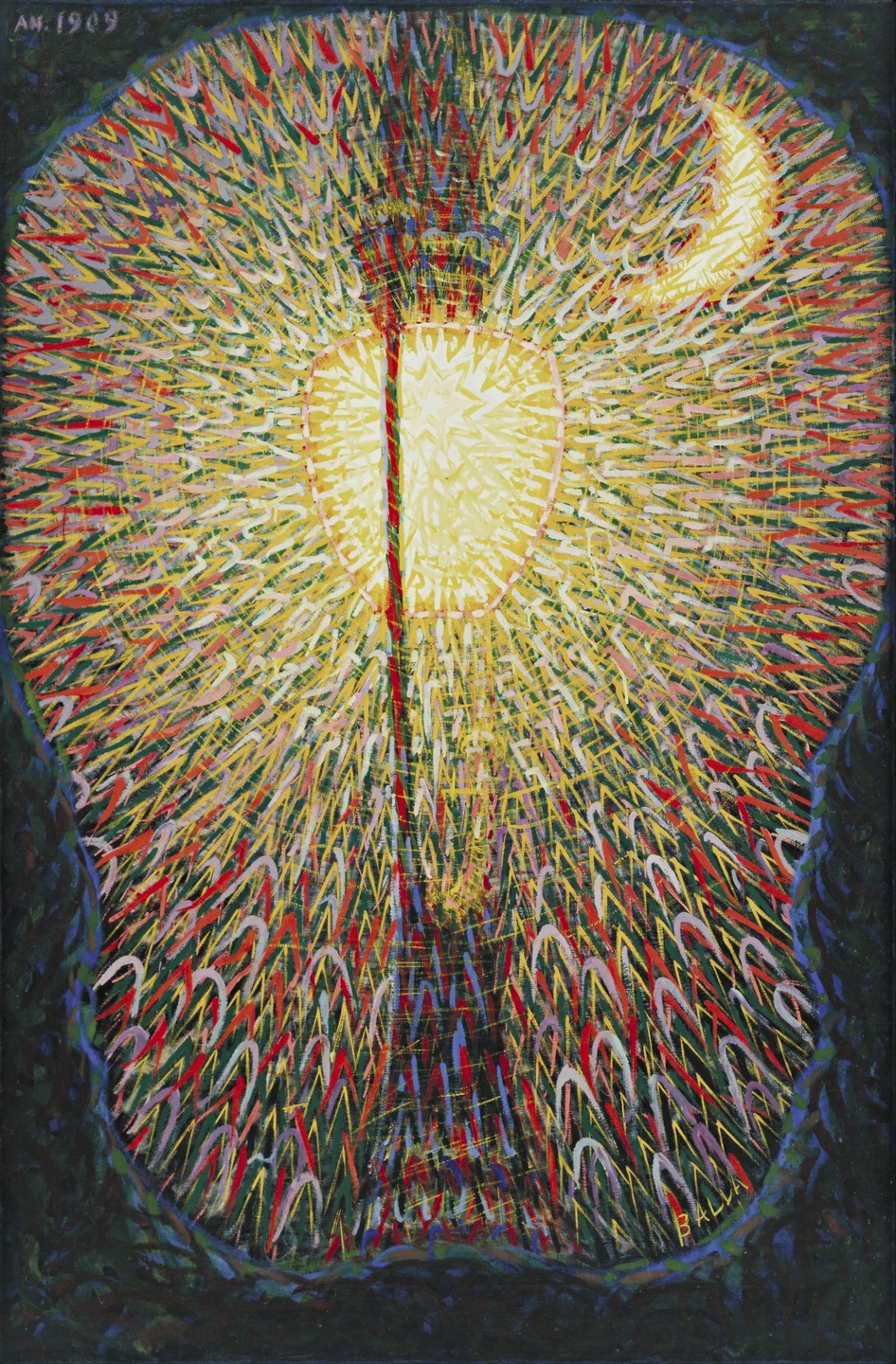
One area of research that has provided important insights into the neurobiology of schizophrenia is the study of sensory gating. Sensory gating refers to the brain’s ability to filter out irrelevant stimuli and focus on the most salient information in the environment. In individuals with schizophrenia, this filtering process is often impaired, leading to a flood of sensory input that can be overwhelming and difficult to process.
Recent studies have suggested that abnormalities in the brain’s indirect pathway, a neural circuit that connects the striatum, globus pallidus, and thalamus, may be responsible for the sensory gating deficits seen in schizophrenia. This same pathway has also been implicated in the neurobiology of post-traumatic stress disorder (PTSD), suggesting that there may be a common neurological substrate for both conditions.
The link between the indirect pathway and schizophrenia has important implications for our understanding of how trauma may contribute to the development of psychotic symptoms. It is well established that trauma can have a profound impact on the brain, leading to changes in neural circuitry and neurotransmitter systems. If the indirect pathway is already compromised due to genetic factors, exposure to trauma may further disrupt its functioning, increasing the risk of sensory gating deficits and psychotic experiences.
This idea is supported by research showing that individuals with a history of trauma are more likely to develop schizophrenia than those without such a history. In fact, some studies have found that up to 80% of people with schizophrenia report having experienced some form of childhood trauma, such as physical or sexual abuse, neglect, or witnessing violence.
However, it is important to note that not everyone who experiences trauma goes on to develop schizophrenia, and not everyone with schizophrenia has a history of trauma. This suggests that there may be different subtypes of schizophrenia, with some cases being primarily genetically driven while others are more heavily influenced by environmental factors.
One way to conceptualize this is to think of schizophrenia as existing on a spectrum, with purely genetic cases at one end and purely trauma-induced cases at the other. In between these two extremes, there may be a range of cases that involve varying degrees of genetic vulnerability and environmental stress.
For example, some individuals may have a very strong genetic predisposition to schizophrenia, such that they are likely to develop the disorder even in the absence of significant trauma or stress. These individuals may have a more classic presentation of schizophrenia, with an earlier age of onset and a more chronic course.
On the other hand, there may be individuals who have a milder genetic vulnerability to schizophrenia, but who experience a significant traumatic event or chronic stress that triggers the onset of psychotic symptoms. These individuals may have a later age of onset and a more episodic course, with periods of relative stability punctuated by acute psychotic episodes.
There is also evidence to suggest that certain environmental factors, such as substance abuse or exposure to psychedelic drugs, may interact with genetic vulnerability to increase the risk of psychosis. For example, research has shown that individuals with a family history of schizophrenia who use cannabis are at a much higher risk of developing psychotic symptoms than those without such a family history.
This idea of a gene-environment interaction is consistent with the concept of a schizophrenia spectrum, as it suggests that the development of psychosis is not purely a matter of nature or nurture, but rather a complex interplay between the two. It also highlights the importance of considering both biological and psychological factors in the assessment and treatment of schizophrenia and related disorders.
The relationship between schizophrenia and trauma has long been a subject of fascination and debate in the fields of psychiatry and psychology. Over the past century, our understanding of these conditions has evolved significantly, moving from the purely psychodynamic theories of the early 20th century to the neurobiological models of today. Yet despite these advances, there remains much to be learned from the pioneering work of figures like Gregory Bateson, Ernest Becker, Carl Jung, and R.D. Laing. By tracing the connections between their ideas and contemporary research on sensory gating, the double bind, and the spectrum of psychosis, we can shed new light on the origins of schizophrenia, the neurological impact of trauma, and the pathways to healing and integration.
Part 2: The Role of Trauma in Schizophrenia
“In schizophrenia, we see the terrible process of psychic fragmentation. The individual, having lost the cohesion of the ego, becomes flooded with autonomous, archaic contents from the unconscious.” (CW 3, The Psychogenesis of Mental Disease)
One of the most significant environmental factors in the development of schizophrenia is psychological trauma. A growing body of research has shown that individuals who experience severe or chronic trauma, particularly during childhood, are at a higher risk of developing psychotic symptoms later in life.
The link between trauma and schizophrenia can be understood through the lens of the double bind theory, first proposed by anthropologist Gregory Bateson in the 1950s. Bateson argued that schizophrenia arises, in part, from chronic exposure to contradictory messages within family relationships. These double binds place the individual in an impossible situation, where they are punished for correctly perceiving the contradiction and punished for failing to acknowledge it. Over time, this leads to a breakdown in the ability to communicate and think clearly, as the individual becomes trapped in a web of paradoxical injunctions.
As Bateson explained in his seminal paper, Toward a Theory of Schizophrenia (1956), “The child is faced with an impossible situation: to obey is to disobey, to disobey is to obey. This inescapable paradox forces a breakdown in reality processing.” For Bateson, “schizophrenia is not a disease of the brain alone, but of communication—an illness that arises when messages contradict each other at fundamental levels.” He argued that chronic exposure to double binds in early life (especially from caregivers) could train the brain into schizophrenic thinking patterns—where reality itself becomes fluid and unstable.
While Bateson’s theory was originally developed to explain the family dynamics of schizophrenia, it has since been applied more broadly to the experience of trauma. Contemporary research on post-traumatic stress disorder (PTSD) has revealed that trauma creates a similar double bind in the nervous system, with the sympathetic (fight/flight) and parasympathetic (freeze/shutdown) branches of the autonomic nervous system activating simultaneously in response to the traumatic event.
This neurological impasse prevents the completion of the stress response cycle, leaving the individual stuck in a state of heightened arousal and emotional dysregulation. The brain becomes trapped in a loop of conflicting signals, unable to fully process and integrate the traumatic experience. Dissociation, a common feature of both PTSD and schizophrenia, emerges as a psychological escape hatch from this double bind, allowing the individual to detach from the overwhelming emotions associated with the trauma.
“What is called ‘madness’ may be a perfectly rational adjustment to an irrational world.” – R.D. Laing
Part 3: Sensory Gating and the Neurobiology of Psychosis
“Schizophrenia is not a breakdown; it is a breakthrough. It is an attempt by the psyche to survive in an unlivable world.” (The Divided Self) – R.D. Laing
Recent research on sensory gating has provided further insights into the neurological underpinnings of schizophrenia and its relationship to trauma and intuition. Sensory gating refers to the brain’s ability to filter out irrelevant stimuli and focus on the most salient information in the environment. In individuals with schizophrenia, this filtering process is often impaired, leading to a flood of sensory input that can be overwhelming and difficult to process.
Studies have shown that abnormalities in the development of the brain’s indirect pathway, a neural circuit that connects the striatum, globus pallidus, and thalamus, may be responsible for the sensory gating deficits seen in schizophrenia. This same pathway has also been implicated in the neurobiology of PTSD, suggesting a common neurological substrate for both conditions.
The link between sensory gating, trauma, and psychosis can be understood through the concept of the “double bind of perception.” In a normally functioning brain, sensory information is filtered and processed in a coherent, integrated way. However, in individuals with a history of trauma, this integrative process is disrupted. The brain becomes trapped between hypervigilance and dissociation, unable to find a middle ground between being flooded with sensory input and shutting down entirely.
This perceptual double bind mirrors the emotional double bind of trauma, creating a self-reinforcing loop of dysregulation and distress. The individual becomes caught between the need to process and make sense of their experiences and the overwhelming nature of those experiences themselves. In this state, the line between internal and external reality becomes blurred, leading to the hallucinations, delusions, and thought disturbances characteristic of psychosis.
“The schizophrenic is drowning in the very material that the mystic swims in.” (CW 18, The Symbolic Life)
-Carl Jung
Part 4: The Spectrum of Psychosis and the Existential Crisis
“Schizophrenia is not a disease of the brain alone, but of communication—an illness that arises when messages contradict each other at fundamental levels.” – Gregory Bateson
The relationship between trauma and schizophrenia is further complicated by the fact that not all individuals who experience trauma go on to develop psychotic symptoms. This has led researchers to conceptualize psychosis as existing on a spectrum, with some individuals being more genetically vulnerable to developing the disorder while others are more resilient.
One factor that may contribute to this differential vulnerability is the existential crisis that often accompanies trauma and psychosis. As existential psychologist Ernest Becker argued in his book The Denial of Death, “The schizophrenic is burdened by a much higher amount of truth than he can bear, and in trying to shuffle off the burden, he is strangled by it.” For Becker, schizophrenia represented the collapse of cultural and psychological defenses, leaving the individual exposed to the raw terror of existence without the protective illusions that most people rely on to function.
Becker saw schizophrenia as the result of an existential terror—the inability to construct a stable symbolic self in the face of overwhelming anxiety. He connected it to the human struggle with mortality and the need for illusions to function. As he wrote in Escape from Evil, “When the defenses of a culture fail, the person is left alone to face the full terror of existence. This is the schizophrenic dilemma: too much reality and not enough illusion.” Becker argued that schizophrenia is the collapse of cultural and psychological defenses, leaving the individual exposed to raw, unfiltered reality—a terrifying condition that most people repress.
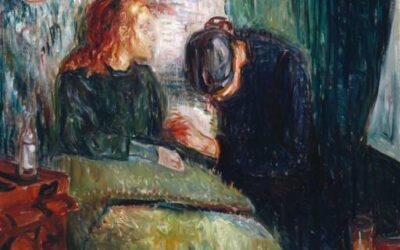
This existential perspective on schizophrenia was shared by other depth psychologists, such as Carl Jung and R.D. Laing. Jung saw schizophrenia as a disintegration of the ego under the weight of an uncontrolled, chaotic unconscious. He believed that the psyche, when overwhelmed by conflicting forces, could split into dissociated parts. As he wrote in The Tavistock Lectures, “Schizophrenia is a condition in which the dream takes the place of reality.” Jung argued that “the schizophrenic is drowning in the very material that the mystic swims in” (CW 18, The Symbolic Life), suggesting that psychosis represents an immersion in the same archetypal forces that spiritual seekers consciously engage with.
For Jung, trauma and unresolved unconscious conflicts could allow these archetypal forces to overtake the ego, resulting in hallucinations and delusions. As he explained in The Psychogenesis of Mental Disease (CW 3), “In schizophrenia, we see the terrible process of psychic fragmentation. The individual, having lost the cohesion of the ego, becomes flooded with autonomous, archaic contents from the unconscious.” Jung believed that the goal of therapy was to help the individual reintegrate these dissociated parts of the psyche and find a new balance between the conscious and unconscious realms.
Laing, in his book The Divided Self, took a similar view, arguing that schizophrenia was not a biological disease but a response to an insane social environment. He saw schizophrenia as a radical coping mechanism, where the self retreats into an internal world to escape overwhelming external demands. As Laing famously wrote, “Schizophrenia is not a breakdown; it is a breakthrough. It is an attempt by the psyche to survive in an unlivable world.” He believed that some schizophrenic symptoms were attempts to resolve unbearable emotional contradictions, stating that “what is called ‘madness’ may be a perfectly rational adjustment to an irrational world.”
Laing was particularly critical of the way that modern capitalist society places impossible demands on the individual, creating a breeding ground for mental illness. He argued that the pressure to conform to social norms, to be productive and successful in a competitive economic system, can create an unbearable sense of alienation and self-doubt. For Laing, schizophrenia was a way of escaping this existential bind, of retreating into a private world where the self can be preserved, even at the cost of losing touch with consensus reality.
Part 5: The Double Bind of Addiction and the Cycle of Dissociation
“The child is faced with an impossible situation: to obey is to disobey, to disobey is to obey. This inescapable paradox forces a breakdown in reality processing.” (Toward a Theory of Schizophrenia, 1956) – Gregory Bateson
The relationship between trauma, dissociation, and addiction is another key piece of the puzzle when it comes to understanding the complex interplay of factors that can lead to schizophrenia and other psychotic disorders. As we have seen, trauma often creates a double bind in the nervous system, where the individual is caught between conflicting impulses to fight, flee, or freeze. Dissociation emerges as a way of escaping this impossible situation, of retreating into an altered state of consciousness where the overwhelming emotions associated with the trauma can be temporarily avoided.
However, this dissociative response can also become a trap in its own right, leading to a cycle of avoidance and numbing that can be difficult to break. As addiction specialist Gabor Maté has argued, substance abuse is often a way of self-medicating the pain of unresolved trauma, of seeking a chemically-induced state of dissociation that provides temporary relief from the underlying emotional wounds.
In his book In the Realm of Hungry Ghosts, Maté writes that “addiction is a response to trauma. It’s an attempt to regulate the dysregulated nervous system, to soothe the pain of unresolved emotional wounds, and to fill the emptiness of a self that has been shattered by neglect and abuse.” He argues that addiction is not a moral failing or a lack of willpower, but a desperate attempt to cope with the overwhelming pain of trauma in the only way that the individual knows how.
This perspective is echoed by other addiction researchers, such as Bruce Alexander, who has argued that addiction is a response to social dislocation and the breakdown of community bonds in modern society. In his book The Globalisation of Addiction, Alexander writes that “addiction is a way of adapting to the dislocation and fragmentation of modern life. It is a response to the loss of meaning and purpose that comes with the breakdown of traditional social structures and the rise of individualism and consumerism.”
For individuals with a genetic predisposition to schizophrenia or other psychotic disorders, the cycle of trauma, dissociation, and addiction can be particularly devastating. The repeated exposure to altered states of consciousness, whether through substance abuse or dissociative coping mechanisms, can further destabilize the already fragile sense of self and reality that characterizes these conditions. The result can be a downward spiral of increasing isolation, paranoia, and psychosis, as the individual becomes more and more disconnected from the social world and the anchors of consensus reality.
“The schizophrenic is burdened by a much higher amount of truth than he can bear, and in trying to shuffle off the burden, he is strangled by it.” (The Denial of Death) – Ernest Becker
Towards an Integrated Understanding of Schizophrenia and Trauma
The relationship between schizophrenia and trauma is a complex and multifaceted one, with roots in both the biological reality of the brain and the subjective experience of the individual. By drawing on the insights of pioneers like Bateson, Becker, Jung, and Laing, as well as the latest research in neuroscience and developmental psychology, we can begin to unravel the mysteries of this relationship and develop more effective strategies for healing and recovery.
At the heart of this understanding is the recognition that schizophrenia is not a monolithic disease entity, but a spectrum of experiences that are shaped by a wide range of genetic, environmental, and existential factors. While some cases of schizophrenia may be primarily driven by biological vulnerabilities, others are more heavily influenced by trauma, social dislocation, and the breakdown of meaning and purpose in modern life.
By taking a more holistic and integrative approach to the treatment of schizophrenia and related disorders, one that addresses the biological, psychological, social, and spiritual dimensions of the individual’s experience, we can begin to create a more compassionate and effective system of care. This may involve a greater emphasis on trauma-informed therapies, such as emotional transformation therapy (ETT), micronutrition, brainspotting, or eye movement desensitization and reprocessing (EMDR), somatic experiencing, and other body-based approaches that help to regulate the nervous system and resolve the underlying emotional wounds.
It may also involve a greater recognition of the existential and spiritual dimensions of psychosis, and a willingness to engage with the individual’s internal world on its own terms, rather than simply trying to suppress or eliminate their symptoms. As Laing and others have argued, the goal of therapy should not be to force the individual to conform to a narrow definition of “normality,” but to help them find a way of being in the world that is authentic, meaningful, and fulfilling, even if it differs from the mainstream.
Ultimately, the key to healing the wounds of trauma and resolving the double binds that can lead to schizophrenia and other forms of psychosis may lie in a fundamental reorientation of our society and our values. By creating a world that is more just, compassionate, and inclusive, one that values human connection and spiritual growth over material success and individual achievement, we can begin to address the root causes of mental illness and create the conditions for true healing and transformation.
References:
- Alexander, B. K. (2008). The globalisation of addiction: A study in poverty of the spirit. Oxford University Press.
- Bateson, G., Jackson, D. D., Haley, J., & Weakland, J. (1956). Toward a theory of schizophrenia. Behavioral Science, 1(4), 251-264.
- Becker, E. (1973). The denial of death. Free Press.
- Freud, S. (1958). Psycho-analytic notes on an autobiographical account of a case of paranoia (dementia paranoides). In J. Strachey (Ed.), The standard edition of the complete psychological works of Sigmund Freud (Vol. 12, pp. 3-82). Hogarth Press. (Original work published 1911)
- Freud, S. (1963). Introductory lectures on psychoanalysis. In J. Strachey (Ed.), The standard edition of the complete psychological works of Sigmund Freud (Vol. 16, pp. 243-463). Hogarth Press. (Original work published 1917)
- Jung, C. G. (1960). The psychology of dementia praecox. In The psychogenesis of mental disease (R. F. C. Hull, Trans.; pp. 3-151). Princeton University Press. (Original work published 1907)
- Jung, C. G. (1968). Analytical psychology: Its theory and practice (The Tavistock Lectures). Vintage Books.
- Laing, R. D. (1960). The divided self: An existential study in sanity and madness. Tavistock Publications.
- Maté, G. (2008). In the realm of hungry ghosts: Close encounters with addiction. Knopf Canada.
- Read, J., van Os, J., Morrison, A. P., & Ross, C. A. (2005). Childhood trauma, psychosis and schizophrenia: A literature review with theoretical and clinical implications. Acta Psychiatrica Scandinavica, 112(5), 330-350.
- Svoboda, E., McKinnon, M. C., & Levine, B. (2006). The functional neuroanatomy of autobiographical memory: A meta-analysis. Neuropsychologia, 44(12), 2189-2208.
- Teicher, M. H., Samson, J. A., Anderson, C. M., & Ohashi, K. (2016). The effects of childhood maltreatment on brain structure, function and connectivity. Nature Reviews Neuroscience, 17(10), 652-666.
- van der Kolk, B. A. (2014). The body keeps the score: Brain, mind, and body in the healing of trauma. Viking.
- Varese, F., Smeets, F., Drukker, M., Lieverse, R., Lataster, T., Viechtbauer, W., Read, J., van Os, J., & Bentall, R. P. (2012). Childhood adversities increase the risk of psychosis: A meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophrenia Bulletin, 38(4), 661-671.
- Walker, E. F., & Diforio, D. (1997). Schizophrenia: A neural diathesis-stress model. Psychological Review, 104(4), 667-685.
Further Resources on Schizophrenia
-
National Institute of Mental Health (NIMH): Schizophrenia
- Comprehensive information on schizophrenia, including symptoms, treatment options, and current research.
-
National Alliance on Mental Illness (NAMI): Schizophrenia
- Detailed overview of schizophrenia, treatment options, and support resources.
-
Substance Abuse and Mental Health Services Administration (SAMHSA): Schizophrenia
- Information on schizophrenia and resources for finding treatment facilities or providers.
-
Mayo Clinic: Schizophrenia
- Overview of schizophrenia, including symptoms, causes, diagnosis, and treatment options.
-
Psych Central: Resources for Schizophrenia
- Information to help understand schizophrenia and connect with treatments or support groups.
-
WebMD: Schizophrenia Resources
- Links to more information and support for those with schizophrenia and their loved ones.
-
Schizophrenia Society of Canada: Resources & Links
- In-depth information about schizophrenia, psychosis, and the path to mental health recovery.
-
Centre for Addiction and Mental Health (CAMH): Schizophrenia
- Information on schizophrenia and crisis resources for areas in and around Toronto.
-
HelpGuide.org: How to Help Someone with Schizophrenia
- Tips for helping a loved one with schizophrenia, including stress reduction and support strategies.
-
Wikipedia: Schizophrenia
- Comprehensive article covering various aspects of schizophrenia, including symptoms, causes, and treatments.

















0 Comments