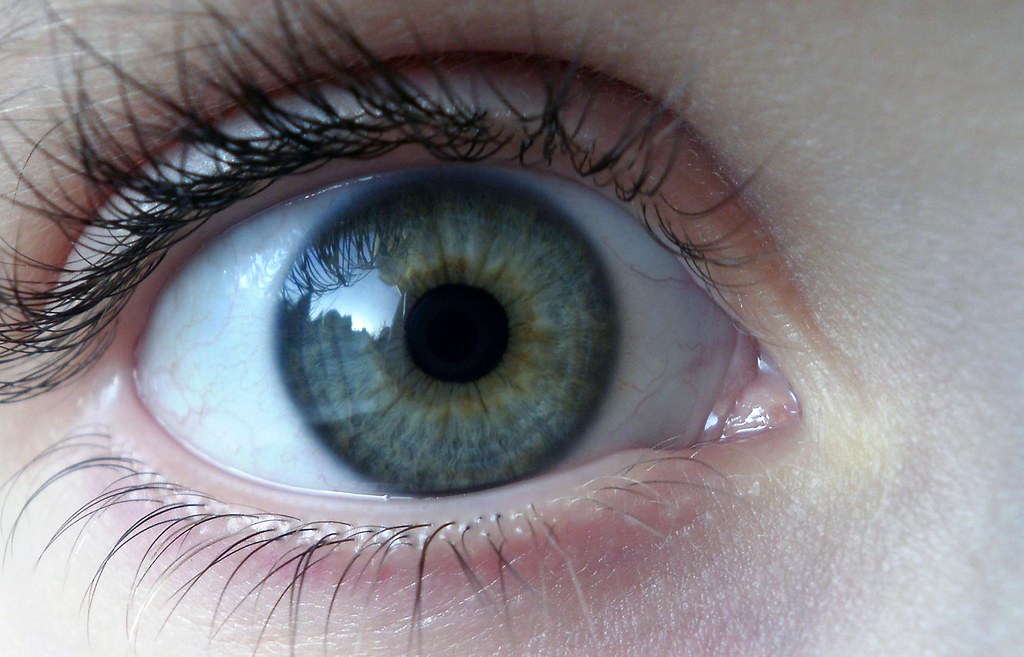
Brainspotting Trauma Therapy Uses Eye Movement
F.A.Q. about Brainspotting
What is Brainspotting? Brainspotting is an innovative psychotherapy approach that uses specific eye positions to access unprocessed trauma in the subcortical brain (Grand, 2013). It was developed by Dr. David Grand in 2003 as an offshoot of EMDR therapy.
How does Brainspotting work?
Brainspotting works by using focused eye positions to access survival-based subcortical parts of the brain like the amygdala that are often inaccessible through talk therapy alone (Grand, 2013). The therapist guides the client’s eyes to find brainspots correlated with specific somatic activations where trauma is held in the brain and body (Schwarz, 2020). The brainspot correlates with traumatic memories or negative emotions that are then processed by keeping the gaze focused on that spot (Corrigan & Grand, 2013). This appears to allow frozen trauma responses from the past to be completed and released (Grand, 2013).
What is the neurobiology behind how Brainspotting works?
Looking at specific eye positions stimulates the brain activity that underlies traumatic experiences, accessing subcortical brain structures including the amygdala, hippocampus, and brain stem (Schwarz, 2020). Focusing the eyes on the brainspot appears to activate and release traumatic memories from these lower brain networks without engaging the conscious neocortex, allowing implicit subcortical memories to process rapidly (Corrigan & Grand, 2013). Brainspotting may work by “rewiring” neural connections in the brain, increasing cross-talk between the hemispheres via the corpus callosum (Grand, 2013).
Why did Dr. David Grand develop Brainspotting?
Dr. Grand, an EMDR therapist, discovered Brainspotting in 2003 when working with an ice skater who had experienced performance issues after a traumatic fall (Schwarz, 2020). He observed that when she looked in a specific direction while thinking of the fall, her distress level rapidly dropped and her performance improved. Through further experimentation, he developed the Brainspotting approach (Grand, 2013).
What is the difference between EMDR, Brainspotting, EMI and ETT?
While all use eye movements to reprocess trauma, they differ in origin, techniques, and procedures:
- EMDR (Eye Movement Desensitization and Reprocessing) is the oldest and most extensively researched. It uses standardized protocols and bilateral stimulation (eye movements, sounds or taps) to reprocess traumatic memories (Shapiro, 2017).
- Brainspotting uses focused eye positions and “mindful body awareness” to target unprocessed trauma in the midbrain without a structured protocol (Grand, 2013).
- EMI (Eye Movement Integration) combines EMDR with hypnosis and NLP techniques to reprocess negative beliefs with eye positions (Beaulieu, 2003).
- ETT (Emotional Transformation Therapy) uses color and eye movements to address emotional imbalances (Vazquez, 2014).
Is Brainspotting like other somatic therapies such as Sensorimotor Therapy, Somatic Experiencing, or Lifespan Integration?
Brainspotting is most similar to Somatic Experiencing in focusing on physiological trauma responses in the body.
While each has unique methods, Brainspotting and other body-based therapies all aim to treat trauma and emotional wounds through physiological processes rather than cognitive methods alone. Similarities include:
- Focus on felt sense and somatic experience to access implicit memories outside conscious awareness
- Follow the client’s organic process rather than predetermined treatment agendas
- Bottom-up processing using interoception and proprioception versus top-down insight and understanding (Ogden, 2015)
Key differences are that Sensorimotor Therapy and Somatic Experiencing focus more on nervous system regulation and titration than Brainspotting (Payne et al., 2015). Lifespan Integration uses a time line and active imagination instead of eye positions to integrate traumatic memories (Pace, 2003).
Which is better, EMDR or Brainspotting?
Currently no head-to-head research exists comparing EMDR and Brainspotting efficacy. Clinical reports suggest Brainspotting may be more efficient for some issues, but EMDR has a much more extensive evidence base from controlled studies for treating PTSD and other conditions (Shapiro, 2017). Ultimately, therapist skill and the client-therapist relationship are more important than modality in therapy outcomes. The best approach depends on a client’s individual needs, preferences and response.
When was Brainspotting invented? Dr. David Grand discovered Brainspotting in 2003 and presented it for the first time at a conference in 2003 (Grand, 2013).
How well researched is Brainspotting? Brainspotting is an evidence-based treatment with a growing research base. To date there have been:
- 2 randomized controlled trials showing Brainspotting significantly reduced PTSD symptoms compared to control groups (Hildebrand et al., 2014; Bellon-Saameno et al, 2023).
- 6 peer-reviewed clinical outcome studies demonstrating Brainspotting’s effectiveness for treating trauma, anxiety, anger and other issues (Grand, 2013; Hildebrand et al., 2017; Fiorini, 2018; Sandberg et al., 2020; Muratori et al., 2021, Tavakoly et al, 2022).
- Over 50 published papers, book chapters and dissertations on Brainspotting theory, practice and outcomes (Brainspotting bibliography, 2023).
However, more controlled research is needed comparing Brainspotting to other treatments. The current evidence base, while promising, is still limited compared to EMDR and other trauma therapies.
What is Brainspotting used to treat?
Brainspotting can treat a wide range of psychological and physical conditions stemming from unresolved trauma, including:
- Post-Traumatic Stress Disorder (PTSD)
- Anxiety, panic attacks & phobias
- Depression
- Addiction & substance abuse
- Chronic pain & illness
- Traumatic brain injury & stroke rehabilitation
- Sports performance & creativity blocks
- Attachment & relationship issues (Grand, 2013)
It has been used effectively with children, adolescents and adults of all ages (Schwarz, 2020).
What happens in Brainspotting therapy sessions?
What is Brainspotting processing like? In a typical Brainspotting session, the therapist helps the client locate brainspots using either a pointer or fixed eye positions. The client focuses their gaze on the brainspot while mindfully observing their inner experience, including thoughts, memories, emotions, and body sensations. The therapist uses bilateral sounds to deepen processing. Processing can feel intense yet often passes quickly as the nervous system releases and rebalances itself. The client does not need to talk extensively about traumatic memories. Afterwards, many people feel a sense of relief, relaxation and empowerment (Grand, 2013).
How many Brainspotting sessions are needed?
The number of Brainspotting sessions needed varies depending on a person’s history, treatment goals and response to the therapy. Straightforward traumas like car accidents may resolve in 1-5 sessions, whereas complex PTSD can take much longer. Many clients report significant improvement within 3-10 sessions (Schwarz, 2020). Some find additional sessions helpful to address other issues that emerge after initial processing. Ultimately treatment should continue until the client feels they have met their goals.
Can Brainspotting be harmful? What are the risks?
Brainspotting is a gentle yet powerful treatment that can evoke strong emotions and sensations as part of the healing process. Some clients may feel emotionally raw, fatigued or “activated” after a session. However, adverse reactions are rare when done under the care of a certified Brainspotting therapist. Potential risks include surfacing traumatic memories the client is not yet ready to process, or flooding/overwhelm from opening up too much unresolved trauma at once. An experienced Brainspotting clinician can help pace and contain the process to minimize these risks (Grand, 2013). As with any therapy, some people will not find Brainspotting helpful or a good fit for their needs.
What happens if Brainspotting doesn’t work? If someone does not experience improvement after several Brainspotting sessions, there could be various reasons:
- More sessions are needed to access and resolve deeper layers of trauma
- Other modalities like EMDR or talk therapy may be a better fit for the client’s issues and preferences
- Unaddressed factors are blocking progress, like current life stressors, secondary gains, or lack of safety/resources
- The therapist-client relationship is not ideal due to poor rapport, mismatch of personalities or therapist inexperience (Grand, 2013)
In such cases, the client and therapist should discuss the reasons Brainspotting may not be working and collaborate on a new treatment plan. This may involve switching to a different therapist or modality, increasing outside support and resources, or taking a break from therapy. What’s most important is empowering clients to trust their own inner healing wisdom.
Can Brainspotting be done online or virtually?
Yes, Brainspotting can be conducted effectively via telehealth platforms, as demonstrated during the COVID-19 pandemic. The therapist uses remote desktop control to move their pointer on the client’s screen and guide their eye movements. Bilateral music can be streamed through the video platform to facilitate processing. Clients can experience the same powerful releases and neural integration as in-person sessions (Schwarz, 2020). However, virtual Brainspotting may not be suitable for people with severe dissociation, psychosis, or safety issues who need direct care.
Can Brainspotting help with Insomnia? OCD? Chronic Pain? Yes, Brainspotting has been used successfully to treat insomnia, OCD, chronic pain and many other issues by healing the underlying trauma that drives these conditions. For example:
- Insomnia is often rooted in hyperarousal from unresolved trauma. Brainspotting can downregulate the nervous system and reprocess the trauma, leading to improved sleep (Schwarz, 2020).
- OCD can be an attempt to control anxiety and intrusive thoughts/images resulting from trauma. Brainspotting can release the trauma and reduce the need for compulsive rituals (Grand, 2013).
- Chronic pain frequently has an emotional component, even if there is also tissue damage. Brainspotting can address the trauma, dissociation or emotional conflicts held in the body and decrease pain sensations (Schwarz, 2020).
However, more research is needed to establish Brainspotting’s efficacy for these specific conditions compared to other treatments. Clients should consult their healthcare providers to determine if Brainspotting is appropriate for their diagnoses and medical history.
What is involved in Brainspotting training?
The Brainspotting training program involves a series of in-person and online seminars, supervision, and practice leading to certification. The core curriculum includes:
Phase 1:
Introduction to Brainspotting principles, neurobiology, setup, therapist presence and attunement skills, Gazespotting technique.
Phase 2:
Expanding with Brainspotting using Outside Window, Rolling Eye and Body Resource techniques; adapting Brainspotting for different diagnoses.
Phase 3:
Advanced Brainspotting techniques including Z-Axis, Convergence and 3-Dimensional BSP; case conceptualization and treatment planning.
Phase 4:
Advanced Resourcing and Body-based BSP approaches to enhance integration.
Trainees must complete at least 50 BSP sessions, 10 hours of consultation, and a written exam to be certified as a Brainspotting therapist. The International Brainspotting Association (IBA) sets training standards and oversees certification (Brainspotting Trainings, 2023).
Can you do Brainspotting on yourself?
While it is possible to use self-administered Brainspotting techniques for stress relief and emotional regulation, it is not advisable to try to process trauma alone without the guidance and support of a trained therapist. Some potential risks of solo Brainspotting include:
- Overlooking blind spots in our own experience and getting stuck in unproductive brainspots
- Flooding the nervous system by opening up too much traumatic material at once without tools to stabilize
- Reinforcing dissociation or unhealthy coping mechanisms rather than discharging trauma
- Missing opportunities for relational healing that come from working with an attuned therapist (Schwarz, 2020)
For these reasons, it is recommended to work with a certified Brainspotting therapist, especially when addressing significant trauma or mental health issues. That said, a therapist can teach clients self-BSP techniques to use between sessions to support their treatment.
Key Points on Brainspotting
- Originated from EMDR therapy
- Uses focused eye positions to target trauma
- Accesses deep brain areas often unreachable through talk therapy
The Science Behind Brainspotting: How Does it Heal Trauma?
Brainspotting’s effectiveness lies in its ability to stimulate and process trauma stored in the brain’s subcortical regions.
Neurobiological Mechanisms:
- Activates amygdala, hippocampus, and brain stem
- Releases traumatic memories without engaging the conscious neocortex
- Potentially “rewires” neural connections, enhancing interhemispheric communication
Brainspotting vs. Other Therapies: What’s the Difference?
Understanding how Brainspotting compares to other trauma therapies can help you choose the right treatment.
Brainspotting vs. EMDR:
- Both use eye movements for trauma processing
- EMDR has more extensive research
- Brainspotting may offer faster results for some issues
Brainspotting vs. Somatic Therapies:
- Similarities: Focus on body awareness and bottom-up processing
- Differences: Brainspotting’s unique use of eye positions
Is Brainspotting Effective? What Does the Research Say?
While newer than some therapies, Brainspotting has a growing body of evidence supporting its effectiveness.
Research Highlights:
- 2 randomized controlled trials showing PTSD symptom reduction
- 6 peer-reviewed clinical outcome studies
- Over 50 published papers and dissertations
Common Applications:
- Post-Traumatic Stress Disorder (PTSD)
- Anxiety and depression
- Addiction and substance abuse
- Chronic pain and illness
- Sports performance and creativity blocks
What Happens in a Brainspotting Session? A Step-by-Step Guide
Understanding the Brainspotting process can help you feel more prepared and comfortable during treatment.
Typical Session Flow:
- Locating brainspots with a pointer or fixed eye positions
- Focusing gaze while observing inner experiences
- Using bilateral sounds to deepen processing
- Minimal talking required during trauma processing
How Many Brainspotting Sessions Will I Need?
The number of sessions varies based on individual needs and the complexity of the issues being addressed.
General Guidelines:
- Simple traumas: 1-5 sessions
- Complex PTSD: Longer treatment duration
- Many clients report significant improvement within 3-10 sessions
Is Brainspotting Safe? Understanding Potential Risks and Side Effects
While generally considered safe, it’s important to be aware of potential risks and side effects of Brainspotting.
Safety Considerations:
- Rare adverse reactions when conducted by certified therapists
- Possible emotional intensity or fatigue after sessions
- Not recommended for self-administration without professional guidance
Can Brainspotting Be Done Online? Exploring Virtual Treatment Options
The COVID-19 pandemic has accelerated the adoption of online Brainspotting sessions.
Virtual Brainspotting:
- Conducted via telehealth platforms
- Uses remote desktop control for eye guidance
- May not be suitable for severe dissociation or safety issues
Brainspotting for Specific Conditions: Insomnia, OCD, and Chronic Pain
Brainspotting’s versatility extends to treating various specific conditions by addressing underlying trauma.
Potential Benefits for:
- Insomnia: Reducing hyperarousal from unresolved trauma
- OCD: Releasing trauma that drives compulsive behaviors
- Chronic Pain: Addressing emotional components of pain
How to Become a Brainspotting Therapist: Training and Certification
For mental health professionals interested in offering Brainspotting, understanding the training process is crucial.
Training Overview:
- 4 phases of core curriculum
- 50 BSP sessions and 10 hours of consultation required
- Certification exam administered by the International Brainspotting Association
Next Steps if You Want to try Brainspotting :
- Consult with a certified Brainspotting therapist
- Discuss if Brainspotting aligns with your treatment goals
- Visit https://brainspotting.com for more information
Remember, the most effective therapy is one that resonates with you and addresses your specific needs. Brainspotting may be a powerful tool in your healing journey.
To learn more about Brainspotting, please visit https://brainspotting.com or consult a local Brainspotting therapist.
References
Beaulieu, D. (2003). Eye Movement Integration Therapy: The Comprehensive Clinical Guide. Crown House Publishing.
Bellon-Saameno, J.A., Amador-Marin, B., Dominguez-Rodriguez, M., Herrera-Mercadal, P., & Navarro-Gil, M. (2023). Effectiveness of brainspotting in women with symptoms of anxiety and related to stress: a randomized controlled trial. Actas Esp Psiquiatr, 51(1), 24-33.
Brainspotting bibliography. (2023). Brainspotting.com. https://brainspotting.com/research-bibliography/
Brainspotting Trainings. (2023). Brainspotting.com. https://brainspottingtrainings.com/
Corrigan, F.M., & Grand, D. (2013). Brainspotting: Recruiting the midbrain for accessing and healing sensorimotor memories of traumatic activation. Medical Hypotheses, 80, 759–766.
Fiorini, M. (2018). Brainspotting: A phenomenological analysis of the clinicians’ experience as Brainspotting practitioners. The Chicago School of Professional Psychology. ProQuest Dissertations Publishing.
Grand, D. (2013). Brainspotting: The Revolutionary New Therapy for Rapid and Effective Change. Sounds True.
Hildebrand, A., Grand, D., & Stemmler, M. (2014). Brainspotting-the efficacy of a new therapy approach for the treatment of Posttraumatic Stress Disorder in comparison to Eye Movement Desensitization and Reprocessing. Mediterranean Journal of Clinical Psychology, 5(1), 1-17.
Hildebrand, A., Stemmler, M., & Grand, D. (2017). Emotionsregulation und Therapieerfolg: Vergleich der Wirksamkeit von EMDR und Brainspotting [Emotion regulation and therapy success: A comparison of the efficacy of EMDR and Brainspotting]. Trauma and Gewalt, 11(3), 204-216.
Muratori, M., Giannino, C., & Cook, H. (2021). The Effectiveness of Trauma-Informed Wilderness Therapy with Adolescents: A Pilot Study. Research in Outdoor Education, 19, 47-67.
Ogden, P. (2015). Sensorimotor Psychotherapy: Interventions for Trauma and Attachment. W. W. Norton.
Pace, P. (2003). Lifespan Integration: Connecting Ego States through Time. Lifespan Integration.
Payne, P., Levine, P.A., & Crane-Godreau, M.A. (2015). Somatic experiencing: using interoception and proprioception as core elements of trauma therapy. Frontiers in Psychology, 6, 93.
Sandberg, H., Doos, M.K., & Wästberg, B. (2020). A Randomized Controlled Study Comparing EMDR and Brainspotting in the Treatment of Psychological Trauma. Journal of Nervous & Mental Disease, 208(12), 950-954.
Schwarz, L. (2020). Brainspotting with Children and Adolescents: An Attuned Treatment Approach for Effective Brain-Body Healing. Routledge.
Shapiro, F. (2017). Eye Movement Desensitization and Reprocessing (EMDR) Therapy, Third Edition: Basic Principles, Protocols, and Procedures. Guilford Press.
Tavakoly, F., Zahraei, M., Jamali, Y., & Alimoradi, F. (2022). The Effectiveness of Brainspotting Therapy on Posttraumatic Growth, Resilience, and Emotion Regulation of Veterans. Journal of Military Medicine, 24(4), 390-399.
Vazquez, S.R. (2014). Emotional Transformation Therapy: An Interactive Ecological Psychotherapy. Rowman & Littlefield.
















0 Comments