For the last forty years, the gold standard of mental health care has been Cognitive Behavioral Therapy (CBT). The premise of CBT is elegant and logical: your thoughts create your feelings. Therefore, if you can catch your negative thoughts (cognitive distortions) and replace them with rational ones, your anxiety and depression should subside. For many people, especially those dealing with situational stress or workplace anxiety, this works beautifully. But for trauma survivors, this model often hits a frustrating wall.
You might sit in a therapist’s office, logically deconstructing your fear. You know you are safe. You know your boss isn’t trying to fire you. You know you are lovable. Yet, your heart is still pounding, your palms are sweating, and your stomach is in knots. This disconnect—between what you know and what you feel—is the defining feature of trauma. It is also the primary reason why talk therapy fails for PTSD. You cannot logic your way out of a survival response because the part of your brain that “knows” things has gone offline.
The Neuroscience: Top-Down vs. Bottom-Up Processing
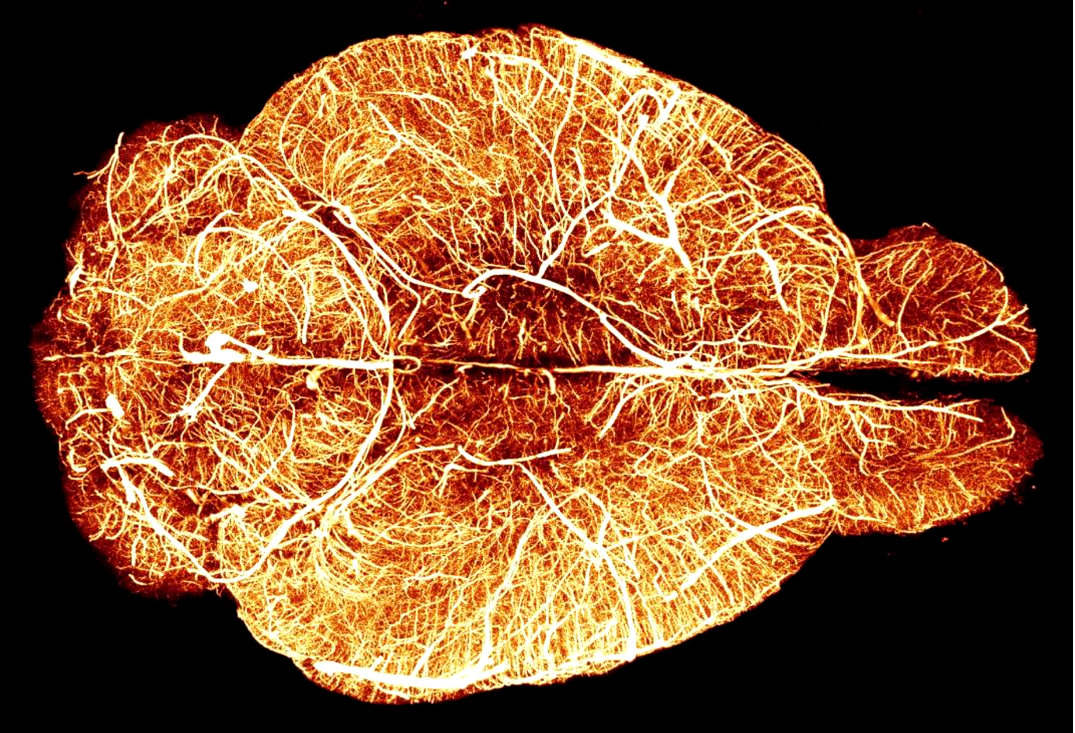
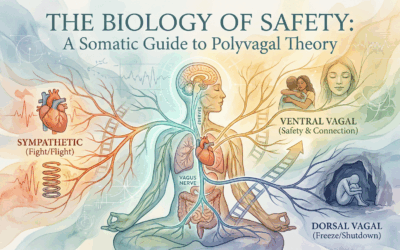
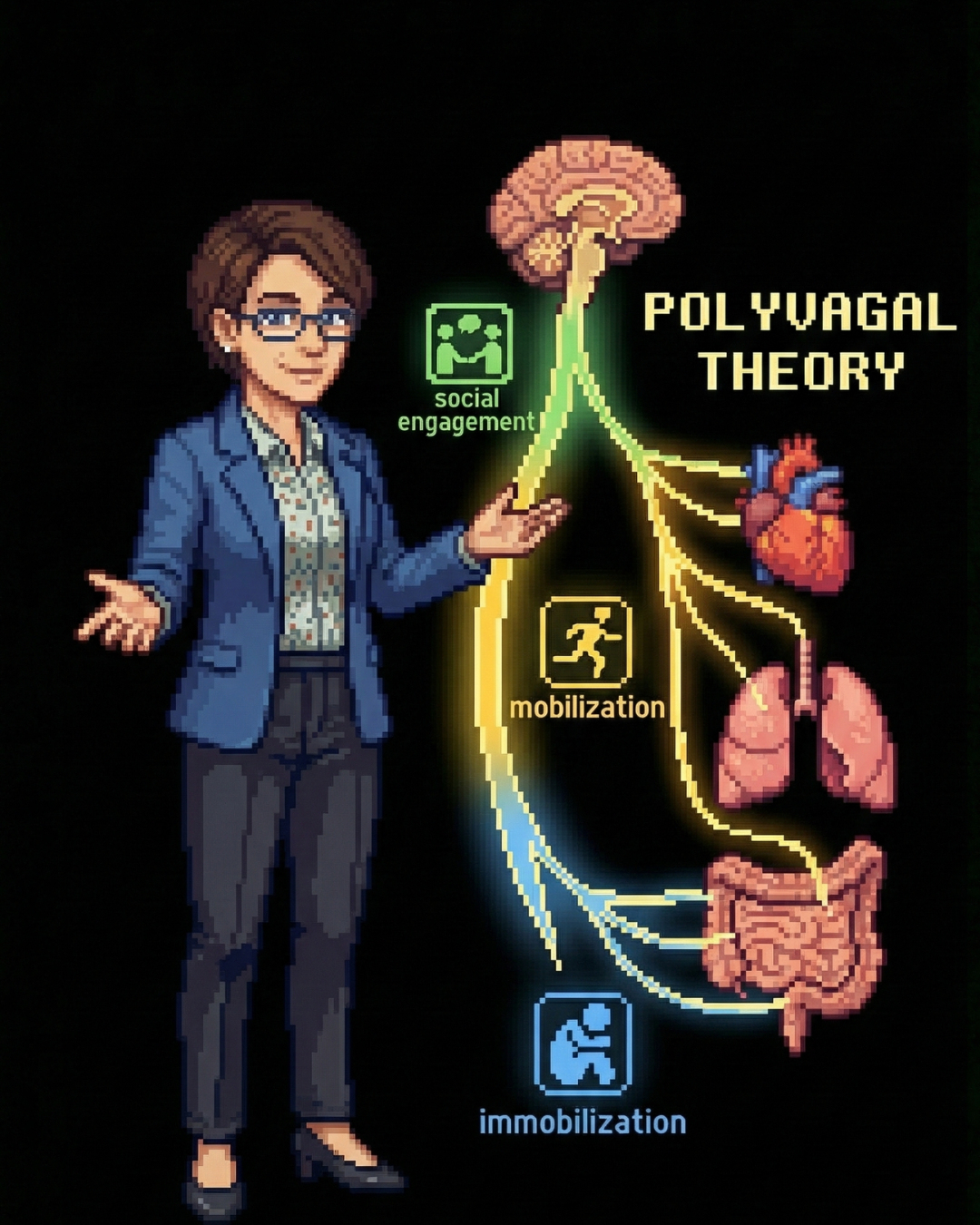
To understand why talking isn’t enough, we have to look at the architecture of the brain. CBT is a “Top-Down” therapy. It engages the Prefrontal Cortex (the newest, most logical part of the brain) and tries to send calming signals down to the limbic system (the emotional brain). This works fine when you are calm. However, when you are triggered, the brain undergoes an Amygdala Hijack.
During a trauma response, the amygdala (the brain’s smoke detector) screams “Fire!” and instantly shuts down the Prefrontal Cortex. This is a survival mechanism; you don’t want to waste time debating philosophy when a tiger is chasing you. But this means that in the exact moment you need your CBT tools, the part of your brain that processes CBT is physically inaccessible. You are not “resistant” or “lazy”; you are biologically incapable of accessing logic because your brain is in survival mode.
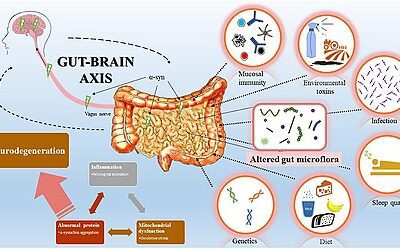
Somatic Therapy works in the opposite direction: “Bottom-Up.” It targets the brainstem and the limbic system first. By changing the physiological state of the body—slowing the breath, releasing muscle tension, tracking sensation—we send a signal up to the brain that says, “We are safe now.” Only once the body is regulated can the thinking brain come back online.
3 Major Somatic Modalities for Trauma
If talk therapy is about insight, somatic therapy is about release. Here are the three primary bottom-up approaches we use to treat complex trauma:
1. Somatic Experiencing (SE)
Developed by Dr. Peter Levine, SE is based on the observation that wild animals rarely get traumatized, despite constant threats. When a gazelle escapes a cheetah, it physically shakes off the excess adrenaline—a “freeze discharge”—and returns to grazing. Humans, socialized to be polite, suppress this shaking. We “keep it together.” SE helps clients slowly access and release this trapped survival energy through bodily sensation (interoception) rather than retelling the story. It is particularly effective for somatic trauma mapping, locating where memories are stored in the muscles.
2. EMDR (Eye Movement Desensitization and Reprocessing)
EMDR uses bilateral stimulation (moving eyes back and forth, tapping, or buzzers) to stimulate the brain’s information processing system. It mimics the REM sleep cycle, allowing the brain to take a “stuck” traumatic memory—which feels like it is happening right now—and file it away as a memory that happened in the past. Unlike CBT, EMDR does not require you to analyze the trauma extensively; it focuses on the dual attention of the memory and the body sensation.
3. Brainspotting
An evolution of EMDR, Brainspotting posits that “where you look affects how you feel.” It identifies specific eye positions (Brainspots) that correlate with deep subcortical trauma capsules. By holding the gaze on a specific spot, the therapist helps the client access deep parts of the midbrain that are inaccessible to speech. It is often described as a “surgical” approach to processing trauma without the need for excessive talking.
The Verdict: Integration is Key
This does not mean CBT is useless. It is an excellent tool for maintenance, integration, and handling the day-to-day stressors of life. But for deep trauma recovery, it is often like trying to put a roof on a house that has no foundation. You must build the foundation of safety in the nervous system first.
If you have spent years in talk therapy retelling your story without feeling relief, it is likely not your fault. You may have been using a top-down tool for a bottom-up problem. Healing happens when we respect the biology of the body, recognizing that the “issues” are not just in our tissues—they are our tissues. By combining the insight of the mind with the wisdom of the body, we can finally move from “managing” symptoms to resolving them.
Timeline of Trauma Therapy Evolution
- 1890s: The “Talking Cure” is established by Freud; focus is on insight and catharsis through speech.
- 1960s: Aaron Beck develops CBT, shifting focus to cognitive distortions and logic.
- 1980s: PTSD is officially recognized in the DSM-III, acknowledging that external events cause internal pathology.
- 1990s: The “Decade of the Brain” leads to imaging studies showing how trauma alters brain structure (Amygdala/Hippocampus).
- 1997: Peter Levine publishes Waking the Tiger, popularizing Somatic Experiencing.
- 2014: Bessel van der Kolk publishes The Body Keeps the Score, bringing somatic therapy into the mainstream zeitgeist.
Select Bibliography
- Van der Kolk, B. (2014). The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma. Viking.
- Levine, P. A. (1997). Waking the Tiger: Healing Trauma. North Atlantic Books.
- Ogden, P., Minton, K., & Pain, C. (2006). Trauma and the Body: A Sensorimotor Approach to Psychotherapy. W. W. Norton & Company.
- Grand, D. (2013). Brainspotting: The Revolutionary New Therapy for Rapid and Effective Change. Sounds True.














0 Comments