You know your triggers. Most of us do. The sharp tone of voice that makes your stomach clench. The email notification that spikes your heart rate. The family gathering that leaves you exhausted for days.
But do you know your glimmers?
If you’ve spent any time in trauma therapy or scrolling mental health content, you’ve likely encountered this term. “Glimmers” has become one of those words that circulates widely—but the depth of what it actually means, and why it matters so much for healing, often gets lost in the sharing.
As a somatic trauma therapist, I want to offer you something more than a definition. I want to help you understand why glimmers might be the most underutilized tool in your nervous system’s healing toolkit—and how to start working with them in ways that actually change your baseline state over time.
What Are Glimmers, Really?
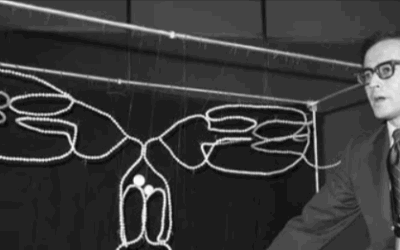
The term “glimmers” was coined by Deb Dana, a clinician and consultant specializing in complex trauma who has done more than perhaps anyone to translate Polyvagal Theory into accessible, practical language.
In Dana’s framework, glimmers are the opposite of triggers. While triggers are cues of danger that activate our survival responses (fight, flight, freeze, or shutdown), glimmers are cues of safety that activate our ventral vagal system—the part of our nervous system associated with calm, connection, and social engagement.
But here’s what’s important: glimmers aren’t big moments of joy or peak experiences. They’re micro-moments. Fleeting. Often barely noticed. The warmth of morning sunlight on your skin. A stranger’s genuine smile. The particular way your coffee smells. Your cat’s purr vibrating against your chest. A song that shifts something in you for just a few seconds.
These moments might seem too small to matter. That’s precisely why they’re so often missed—and why learning to notice them can be transformative.
The Neuroscience: Why Small Moments Have Big Impact
To understand why glimmers matter, we need to understand what’s happening in the nervous system.
According to Polyvagal Theory research, our autonomic nervous system operates through a process called neuroception—a kind of unconscious surveillance system that’s constantly scanning for cues of safety and danger. This scanning happens below conscious awareness, in the brainstem and body, before we have any thoughts about whether we’re safe or not.
When neuroception detects danger cues, the nervous system shifts into protective mode: sympathetic activation (fight/flight) or dorsal vagal shutdown (freeze/collapse). When neuroception detects safety cues, the system can settle into what’s called ventral vagal tone—the state that supports connection, creativity, digestion, immune function, and all the repair processes our bodies need.
Here’s the key insight: for people who’ve experienced trauma or chronic stress, neuroception often becomes biased toward detecting danger. The surveillance system gets tuned to high alert. It finds threats everywhere and struggles to register safety cues even when they’re present.
This isn’t a character flaw or a cognitive distortion. It’s an adaptive survival response that helped you survive difficult circumstances. But it means that your nervous system may be missing the glimmers that are actually there—the small moments of safety that could help resource your system toward regulation.
Glimmers work because they gently interrupt this pattern. Each time you notice a glimmer—truly notice it, letting it register in your body—you’re essentially providing your neuroception with evidence that safety exists. You’re training your nervous system to recognize cues it may have been filtering out.
Why Therapy Focuses on Triggers (And Why That’s Not Enough)
As Deb Dana often notes, “Clients come to me because of their triggers, not their glimmers.”
This makes sense. Triggers cause pain, disruption, suffering. Of course we want to address them. And understanding your triggers is genuinely valuable—it helps you anticipate difficulty, develop coping strategies, and make sense of reactions that might otherwise feel confusing or shameful.
But here’s what the biomedical model often misses: wellbeing isn’t just the absence of distress. It’s also the presence of regulation, connection, and moments of genuine safety. You can reduce triggers and still feel chronically dysregulated if your system has no experience of—or capacity for—ventral vagal states.
Think of it this way: if you’re trying to fill a bathtub but the drain is open, you have two options. You can try to plug the drain (reducing triggers), or you can also turn on the faucet (increasing glimmers). Most approaches focus almost entirely on the drain. Glimmer work turns on the faucet.
This is especially important for complex trauma, where the nervous system may have limited experience of safety. You can’t just remove triggers and expect regulation to spontaneously appear. The system needs positive experiences of safety to build new patterns.
The Glimmer Practice: How to Actually Do This
Noticing glimmers sounds simple, but for many people—especially those with trauma histories—it’s surprisingly difficult. The nervous system has gotten efficient at filtering out safety cues. The cognitive mind may dismiss small moments as “not counting.” There may even be resistance to feeling good, if positive states have historically been followed by disappointment or danger.
So we need to approach this gently, with curiosity rather than demand.
Start With Noticing
For one day, simply set an intention to notice any moment—no matter how brief—when something in you settles, softens, or feels even slightly okay. You’re not trying to create anything. You’re just watching for what’s already there.
Some questions that can help:
- What am I seeing right now that my eyes enjoy resting on?
- Is there any sound in my environment that feels pleasant or neutral?
- What does my body appreciate in this moment—temperature, texture, support?
- Is there any relationship (human, animal, plant, place) that brings a sense of ease?
Glimmers are highly personal. What registers as safety for one person may be neutral or even triggering for another. This is about discovering your specific nervous system’s cues of safety.
Let It Land
When you notice a potential glimmer, pause. This is the crucial step most people skip.
Don’t just note it cognitively (“oh, that’s a glimmer”) and move on. Let yourself actually feel it. Where in your body do you notice the effect? Maybe a slight release in your shoulders. A deepening of breath. A softening in your belly. A settling in your chest.
Stay with this sensation for 10-30 seconds. This duration matters—it gives your nervous system time to actually register the experience and begin encoding it. Fleeting awareness doesn’t create the same neuroplastic change as sustained attention.
This is similar to what we do in Brainspotting—using focused attention and body awareness to help the nervous system process and integrate experience. The somatic and neurological mechanisms are related.
Name It (If That Helps)
Some people find it useful to name their glimmers, either in the moment or by keeping a glimmer journal. “Morning coffee warmth.” “Cat purr.” “Sarah’s laugh.” “That particular tree on my walk.”
Naming can help bring implicit experience into explicit awareness, which supports integration. But if naming feels like it pulls you out of the felt sense, skip it and stay with the body experience.
Build a Glimmer Map
Over time, you can begin to map where your glimmers tend to live. Dana’s framework suggests looking in three domains:
Inside the body: What internal sensations cue safety? Maybe the feeling of your feet on the ground, or the rhythm of your own heartbeat when it’s calm, or the sensation of a full exhale.
In the environment: What in your external surroundings cues safety? Natural light, certain colors, particular spaces, familiar objects, the presence or absence of sound.
Between people: What in relationships cues safety? Certain tones of voice, particular kinds of eye contact, specific people whose presence settles your system, even memories of connection.
Mapping your glimmers helps you intentionally create more opportunities for your nervous system to encounter safety cues. This connects to the work of somatic trauma mapping—understanding your body’s patterns so you can work with them more skillfully.
Common Obstacles (And How to Work With Them)
“I can’t find any glimmers”
If you’re in a significantly dysregulated state—deep dorsal vagal shutdown or intense sympathetic activation—glimmers may genuinely be hard to access. This isn’t failure; it’s information about your nervous system’s current state.
Start smaller. Can you find a moment that’s even slightly less bad? A moment of neutral rather than positive? Sometimes the path back to ventral vagal goes through incremental shifts rather than direct jumps to “good.”
Our guide to fast interventions for panic and dissociation offers some starting points for working with more intense states.
“I notice it but nothing happens in my body”
This may indicate dissociation or reduced interoceptive awareness—both common after trauma. The connection between noticing and feeling has been disrupted.
This is workable, but it often needs support. Somatic approaches like EMDR, Brainspotting, or mindfulness practice can help restore the capacity to feel. Working with a therapist trained in these approaches is often valuable here.
“I feel guilty or anxious when something good happens”
This is surprisingly common, especially in trauma survivors. Sometimes called “foreboding joy” or “upper limit problems,” this pattern reflects a nervous system that has learned to associate positive states with subsequent disappointment, danger, or loss.
If good feelings were historically followed by bad things, your system may have learned to preemptively shut down positive states as a form of protection. “Don’t get too happy—something bad is coming.”
This is important shadow material. From a parts-based perspective, there’s likely a protector part that’s trying to keep you safe by preventing hope or joy. This part needs understanding and reassurance, not override.
Work very gently here. Perhaps start with glimmers that feel safe enough—neutral or mildly pleasant rather than intensely positive. Let your system gradually learn that small good things can happen without disaster following.
“This seems too simple to actually help”
I understand this skepticism. If you’re dealing with serious trauma, chronic illness, or significant life challenges, the suggestion to “notice nice moments” can feel dismissive or naive.
But glimmer work isn’t about positive thinking or pretending things are fine when they’re not. It’s about providing your nervous system with accurate information. If you’re currently safe—if in this specific moment, there’s no immediate threat—your nervous system may not know that. Glimmers help it know.
This doesn’t fix external circumstances. It doesn’t erase trauma. But it can gradually shift your baseline nervous system state, which affects everything: your capacity to think clearly, connect with others, make decisions, and access resources for dealing with actual challenges.
Glimmers and Co-Regulation
One of Polyvagal Theory’s most important contributions is the concept of co-regulation—the way nervous systems influence each other in relationship. We’re not meant to regulate in isolation. Our systems are designed to calibrate off other systems.
This has implications for glimmers. Some of your most potent glimmers may be relational. The feeling of being truly seen by another person. A moment of genuine laughter shared. The experience of someone’s calm presence helping your system settle.
And it works the other way too: as you build more capacity for ventral vagal states, your presence becomes a potential glimmer for others. Your regulated nervous system sends safety cues that other systems can pick up.
This is particularly relevant in therapy. One of the things a skilled trauma therapist provides is regulated presence—a nervous system that can stay grounded while you explore difficult territory. The therapeutic relationship itself can become a source of glimmers and a laboratory for building co-regulatory capacity.
Donald Kalsched’s work on archetypal defenses illuminates how early relational trauma creates protective systems that can block connection. Understanding these patterns helps us work more skillfully with the relational dimensions of glimmer work.
Beyond Individual Practice: Creating Glimmer-Rich Environments
Once you understand glimmers, you start noticing how environments either support or undermine nervous system regulation.
Think about the last time you walked into a space and immediately felt your shoulders drop, your breathing deepen. That environment was sending your neuroception safety cues—through lighting, sound, temperature, aesthetics, the energy of people present.
Now think about spaces that make you feel activated or shut down. Harsh lighting. Crowded conditions. Aggressive visual design. The felt sense of people being stressed or performative.
You can intentionally design your personal spaces to include more glimmers. This isn’t about perfection or Instagram aesthetics—it’s about paying attention to what genuinely settles your specific nervous system and including more of that in your environment.
Glimmers and Neurodivergent Burnout
For autistic individuals, those with ADHD, and other neurodivergent folks, glimmer work may need some adaptation.
Sensory sensitivities mean that glimmers and triggers can be closely related—the same sensation might be soothing at one intensity and overwhelming at another. Additionally, many neurodivergent people have had their natural glimmers pathologized or discouraged (stimming, special interests, need for solitude or routine).
If you’re neurodivergent, part of glimmer work may involve reclaiming the things that actually regulate your specific nervous system, even if they look different from neurotypical norms. Your glimmers are valid even if others don’t understand them.
The Deeper Pattern: Reclaiming Capacity for Good
At the deepest level, glimmer work is about reclaiming your capacity to experience goodness, safety, and connection—capacities that trauma can diminish but never fully destroy.
Jung’s work on holding the tension of opposites is relevant here. Healing isn’t about eliminating difficulty or achieving perpetual positive states. It’s about building a nervous system flexible enough to hold both—to experience the full range of life without getting stuck in survival mode.
Glimmers don’t deny your pain. They don’t minimize your triggers. They simply remind your nervous system that safety exists, connection is possible, and your body can still experience moments of regulation. From that foundation, you can face difficult things with more resource.
Getting Support
Glimmer work can be done on your own, but it’s often enhanced by working with a therapist who understands nervous system regulation and can help you navigate obstacles.
At Taproot Therapy Collective in Birmingham, Alabama, we specialize in somatic and brain-based approaches to trauma, including Brainspotting, EMDR, Somatic Experiencing, and parts-based therapy. These approaches work directly with the nervous system to build capacity for regulation—including the ability to notice and metabolize glimmers.
We serve clients in Hoover and greater Birmingham, and offer teletherapy throughout Alabama including Montgomery and Tuscaloosa. Learn more about our approach to trauma and PTSD treatment.
Your nervous system learned to survive. Now it can learn to recognize safety. Glimmers are part of how that happens—one micro-moment at a time.
Related Reading
- 20 Fast Interventions for Panic and Dissociation
- The Somatic and Neurological Experience of Brainspotting
- Navigating Neurodivergent Burnout
- Donald Kalsched: Archetypal Defenses and Trauma
- Find Your Inner Child
- The Body Keeps the Score 2: The Path Forward
- Karen Horney’s 3 Neurotic Personality Styles
- Mapping Your Shadow: A Somatic Meditation













0 Comments